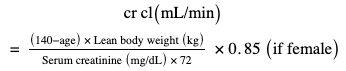
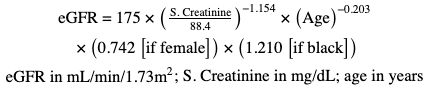
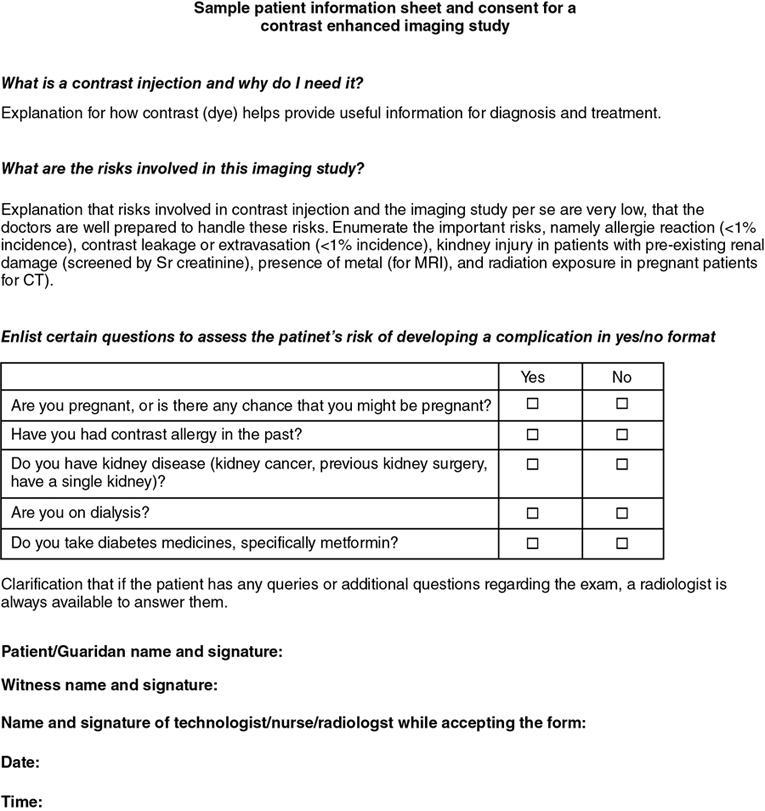
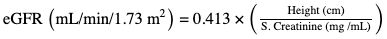
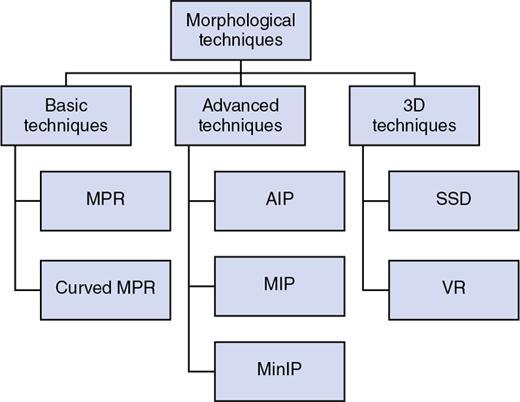
PATIENT PREPARATION FOR CT SCAN Aditi Raina, Gurdashdeep Singh Madan, Gaurav Goswami An adequate prescan patient preparation is as important as the optimization of the CT technique to ensure safe and clinically useful examinations. Broadly speaking, the patient preparation is more elaborate in case of contrast-enhanced CT scan as compared to the noncontrast scan. Also, it is imperative to note that the points discussed henceforth are standardized and common to the routinely performed CT scans in the radiology department. However, certain CT scans like CT enteroclysis or enterography, CT coronary angiography, etc., require specialized preparation and premedication. They will be discussed in detail in the relevant sections. The first and foremost is accurate patient identification. This can be done by the technologist asking the full name of the patient and confirming the unique registration ID. Checking the patient’s arm band can also be used when patient is unable to communicate. Errors of identification pose risks like performing wrong investigation, exposure of unnecessary radiation and iodinated contrast to the patient. Also, there is a possibility of administration of iodinated contrast to an allergic patient and a worst possible scenario of incorrect treatment given on the basis of erroneous diagnostic information. It is also important to note that the appropriateness of the type of CT scan requested should also be verified as to whether it is the optimal investigation for patient’s disease condition or clinical suspicion. The appropriateness criteria like those given by American College of Radiology (ACR), European Society of Radiology (ESR) and Royal college of Radiologists (RCR) are readily available to make a correct decision in conjunction with the referring clinician. The risk–benefit ratio to the patient and the cost–benefit ratio to the patient and to the organization should also be considered. An appropriate detailed medical history is vital to all CT examinations. It will help to ensure a patient’s safety (including contraindication to contrast media use). Also, it will offer the radiologist valuable diagnostic information and aid in guiding the selection of examination protocol. It is important that the patient is preinformed to bring his previous medical records and investigations at the time of the scan as most serial or follow-up scans require comparative analysis to reach a conclusion about status of disease (Fig. 2.20.1.1). Screening for the conditions and medications detailed below is recommended prior to the CT scan (this is usually needed for contrast-enhanced CT scans). Allergy: this is the most important point elicited in history pertaining to radiological examination. The risk of allergic-like contrast reaction in patients with known allergies is two- to threefolds that of the general population. Also, a prior history of reaction to a class of contrast medium (whether allergic-like or unknown type reaction) increases the risk to as high as fivefolds. However, it is important to note that a prior reaction to gadolinium-based contrast media does not increase the probability of reaction to iodinated contrast media. Beta-blockers: They are shown to reduce the threshold and increase severity of contrast reactions and reduce the responsiveness of treatment with epinephrine. However, restriction of contrast or discontinuation of drug is not required prior to contrast administration (Table 2.20.1.1). Systemic disorders: Concerns and recommendations for specific systemic disorders are tabulated below: Certain prerequisites for postcontrast CT scans or for patients requiring sedation are required to be followed. Nil by mouth or Nil per oral (NBM/NPO) is a safety precautionary measure. Patient is expected to be NBM for at least 4 hours prior to the imaging. Few centres stress for 6 hours or more of fasting. The basis for this requirement is that nausea and vomiting are relatively frequent side effects of contrast administration. These are worse if the patient is not fasting. Also, scanning in supine position increases the risk of aspiration and subsequent complications. Water intake is allowed to avoid dehydration during the period (Table 2.20.1.2). Assessment of renal function is of utmost importance before commencement of postcontrast CT scans. It is imperative to have a baseline serum creatinine (with or without eGFR) value available before injecting contrast medium in all patients who could be at risk of developing contrast-induced nephropathy (CIN). Cockcroft–Gault formula for creatinine clearance cr cl ( mL / min ) = ( 140 − age ) × Lean body weight ( kg ) Serum creatinine ( mg / dL ) × 72 × 0 . 85 ( if female ) Though, in routine practice, serum creatinine estimation is required for all patients undergoing contrast-enhanced scans, ACR Committee on Drugs and Contrast Media recommends that patients ‘without the above risk factors may be exempted from renal function assessment’. The creatinine tests done within 30 days of the CT scan are admissible. The formula for calculation of Creatinine clearance is Cockcroft–Gault formula. eGFR (estimated GFR) calculated by the abbreviated Modification of Diet in Renal Disease (MDRD) equation: Modification of Diet in Renal Disease (MDRD) equation for eGFR eGFR = 175 × ( S. Creatinine 88.4 ) − 1.154 × ( Age ) − 0.203 × ( 0.742 [ if female ] ) × ( 1.210 [ if black ] ) eGFR in mL/min/1.73m 2 ; S. Creatinine in mg/dL; age in years eGFR calculators are also available online, which can be used in routine practice. The calculation of eGFR is of utmost importance in high-risk patients or patients who have high serum creatinine levels. As per recommendations by the American College of Radiology and National Kidney Foundation, prophylaxis is prescribed in patients who have eGFR values of less than 30 mL/min/1.73 m2 in high-risk patients not undergoing maintenance dialysis and in high-risk patients with eGFR of 30–44 mL/min/1.73 m2. Consent or filling the patient information form is a method of effective mutual communication between the patient and the doctor/technologist, which leads to the patient giving (or withholding) permission from the doctor to act in a particular way. It can either be implied or express (verbal or written), preferably written. Information should be in plain language, commensurate with the person’s age, education and cultural background. The technologist should describe to the patient in brief the overall method of the procedure, the approximate time duration, whether contrast agents will be administered and any associated potential side effects which can be expected and instructions for patient (e.g., remove metallic objects, change into a patient gown, breath holding on hearing command, etc.). The consent or the patient information sheet should include questions pertaining to the patient’s risk for developing a contrast related complication, procedure details and the potential risks such as anaphylaxis and death with their incidence. Also, the proforma should include information regarding imaging of pregnant patients. It should be conveyed to the patient that in case of any doubts or queries, a discussion with the radiologist can be initiated. The need to inform all patients about radiation risks is an equivocal topic. In the case of paediatric patients, a parent or a legal guardian must sign the consent form. In case of emergency, when informed consent cannot be obtained, the medical imaging examination should be performed, provided it is limited to what is immediately necessary to save life and avoid significant deterioration in the patient’s health (Fig. 2.20.1.2). Multiple studies have proven that in utero exposure of ionizing radiation has significant detrimental effects on fetus. Hence, it is very important to rule out pregnancy in female patients of childbearing age before undergoing CT scan examinations. This can be done by eliciting menstrual history and/or pregnancy tests and it is recommended to delay the examination till the pregnancy status is determined. If a patient is found to be pregnant, careful ‘risk versus benefit’ analysis of the examination must be carried out. The procedure may be postponed, modified or cancelled to reduce the likelihood of direct exposure to the conceptus. If the CT scan is unavoidable or its benefits outweigh the risks involved, it should be performed after discussion between the radiologist and the clinician and after obtaining additional informed consent. If the scan in performed during pregnancy, use of narrow collimation and wide pitch (thus the patient’s movement through the scanner is at a faster pace) will result in some deterioration of image quality, but there is significant reduction in radiation exposure. Also, efforts should be made to monitor dose by placing personnel dose monitors above and below patient’s pelvis to have a proper documentation which can be used later to decide further course of management. The pregnant female is at a relative higher lifetime risk of development of breast cancer as compared to a nonpregnant female. Hence, minimal chance of exposure of chest should be practiced whenever necessary. Another aspect to be kept in mind is the iodine content of contrast media which has the potential to cross blood–brain barrier and thus cause hypothyroidism in the neonate. Hence, the patients are advised to get neonatal thyroid function checked in the first week of life. Breastfeeding: A very small percentage of iodinated contrast medium can be excreted into the breast milk and absorbed by the infant’s gut. The initiation of breast feeding after receiving such an agent is considered safe for both infant and mother. The patient should refrain from breastfeeding for a period of 24 hours and prefer to discard the expressed breast milk from both the breasts during that period. Metformin necessitates a special mention for contrast administration. It is a routinely prescribed antihyperglycaemic drug which is excreted unchanged by the kidneys, probably by both glomerular filtration and tubular excretion. It is estimated that approximately 90% of the absorbed drug is eliminated within the first 24 hours. The most important adverse effect due to metformin is lactic acidosis which may occur if the metformin excretion is hampered. Thus, setting of renal insufficiency is an independent risk factor to be considered by radiologists for patients on metformin. Therefore, the management of patients on metformin is important to be addressed. The management of patients taking metformin is as described below: ACR Committee on Drugs and Contrast Media has classified patients based on the patient’s renal function (as measured by eGFR) as follows (Table 2.20.1.3): No need to discontinue metformin before or after the procedure. No need to reassess patient’s renal function. Discontinue metformin at the time or before procedure and to not take the drug for 48 hours post the procedure. Should be reinstituted only when renal function test is found to be normal. The use of these drugs is to lower the possibility of allergic-like reactions in high-risk patients undergoing contrast study. Low cost and convenience of administration make oral premedication preferable to IV premedication. Inclusion of diphenhydramine (or any other nonselective antihistamine) orally or intravenously 1 hour before contrast medium administration may reduce the frequency of urticaria, angioedema and respiratory symptoms. Due to the meticulously balanced ratio of risks and benefits of premedication, it is used in specific scenarios and indications which are discussed in detail below. In certain clinical and emergency situations, there might be a need to administer contrast medium to a high-risk patient without any premedication. The decision is made jointly by the referring doctor, radiologist and, if possible, the patient as well. In such situations, a team of individuals highly skilled in resuscitation should be present whilst the injection is administered to look for and manage any possible developing reaction. However, if in any scenario there is history of a prior severe contrast reaction, it is considered to be a relative contraindication to receive same class of contrast medium in the future. But if there is no other option and same class of contrast medium is necessary and there are no alternatives, premedication should be considered. As per ACR guidelines, certain recommended premedication regimens should be followed: If a patient is unable to take oral medication, substituting 200 mg hydrocortisone IV for each dose of oral prednisone will suffice. No documented efficacy is seen for all the above mentioned regimens if given for a duration of less than 4–5 hours. These regimens may be considered in emergency situations if no other alternative is present. It is important to note that premedication strategy does not substitute for preadministration preparedness. Contrast reactions can occur despite premedications and so the radiology team must be prepared to treat any such contrast reactions if they occur. In certain circumstances, sedation or anaesthesia may be necessary prior to commencement of CT examination to ensure procurement of good quality images and avoid repeated examinations and radiation exposures. This is an integral part of NORA – nonoperating room anaesthesia. The medications used depend on the duration and depth of anaesthesia required for the test. Though it is primarily the responsibility of the anaesthetist on duty, the radiologist should be familiar with the fundamentals of this step. In children, for elective procedures, the 2-4-6 fasting rule holds true in which no clear fluids inclusion 2 hours prior to the procedure, no breast milk 4 hours prior to the procedure and no solids 6 hours prior to the procedure. For adults, fasting of at least 4 hours is acceptable. Triclofos syrup is available in most departments as an oral sedative for paediatric patients with dosage of approx. 30–50 mg/kg. Variety of intravenous/intramuscular medications can be employed like midazolam, pentobarbital, ketamine, propofol and fentanyl; of these, midazolam (0.02–0.03 mg/kg) and ketamine are used commonly. Patient preparation module in paediatrics includes a few variations as compared to the adult population. The steps include the following: Emphasis must be given to simple, age and intellect-adapted information to the child and information for the parents about the CT examination. Children friendly environment like projection of pictures and painting on the ceiling can have a positive impact on the child. Sometimes use of a vacuum pillow can help fixate a small baby or a part of the body. If successful, these steps ensure good quality data acquisition and obviate the need for sedation or anaesthesia. Normal serum creatinine concentrations are quite variable in paediatric patients, even in the presence of preserved renal function. Also, serum creatinine levels increase with increasing age. The estimated glomerular filtration rate (eGFR) calculation in children is done by the following: Bedside Schwartz equation for eGFR in paediatric age group eGFR ( mL/min/1.73 m 2 ) = 0.413 × ( Height (cm) S. Creatinine (mg /mL) ) Use of hyperosmolar contrast can lead to high-volume intravascular osmotic loads which occur due to fluid migration from extravascular soft tissues into blood vessels in neonates and small children as they are susceptible. It may precipitate cardiac failure and pulmonary oedema in some patients who are at risk. If contrast medium viscosity is high and the angio-catheter is small, the desired injection flow rate may not be achieved, and it may lead to adverse events like catheter failure and/or vessel injury. Rise in temperature reduces the viscosity of contrast media resulting in increased flow rates at lower pressures. A study by Vergara and Segue has concluded that fewer adverse effects of contrast media are seen on using warmed up contrast as compared to that at room temperature in both adult and paediatric patients. The standard contrast material which is used for IV administration is a nonionic, low-osmolar contrast agent with a concentration between 240 and 400 mg I/mL (most frequently 300 mg I/mL). The standard administered dose is approximately 1–2.0 mL/kg (concentration 300 mg I/mL). However, it is considered safe to increase the dose to 3.0–4.0 mL/kg (or a maximum of 150 mL) even in children, when the renal function is normal. The scan and technical parameters should be tailored to achieve the primary goal of optimal diagnostic image quality rather than optimal image quality in order to minimize the radiation dose to the child (ALARA). In other words, if by using low dose the clinical question is answered, then a certain amount of image noise can be considered acceptable. Apart from routine prerequisites like NBM and renal function assessment, CT coronary angiography requires other measures particularly like continuous monitoring of heart rate and ECG and sometimes even premedication like a beta blocker. Administration of positive or negative (water, mannitol) oral contrast and rectal contrast as per the indication of the scan and required diagnostic information. These examinations require meticulous prior bowel preparation. These include low-residue diet, ample amount of fluids as well as laxative on the day prior to the examination. Also, the patient is needed to be nil by mouth on the day of the examination. CT enterography is done using negative or neutral oral contrast whose attenuation is similar to that of water, e.g., water, polyethylene glycol, mannitol, methylcellulose and low-density barium sulphate preparations (Volume, 0.1% W/V) The radiology technician or technologist plays a vital role in patient care. The fundamentals include the following: POSTPROCESSING TECHNIQUES OF CT SCAN Ankita Dhawan, Aditi Raina, Gaurav Goswami Multidetector CT and its capacity of postprocessing of voluminous data has brought a revolution in the field of radiology. Its use has brought about a great deal of change in interpretation of simple axial data. This feature has not only improved interpretation skills for radiologists but has also helped in improving the understanding for referring clinicians. Postprocessing has a variety of clinical implications in different organs and systems as it provides additional diagnostic information. These postprocessing techniques can be broadly categorized into two types: Multiplanar reformation (MPR) is a technique of creating nonaxial images from originally acquired axial CT images. These MPR images can be acquired in coronal, sagittal, curved or oblique planes. The raw data for this is obtained from a stack of axial planes, with the stack being only one voxel in thickness 1. Such technique is particularly useful for eyeing structural anomaly within skeletal framework which is not well appreciated in plain axial images. Multiplanar images can be converted to thickened slab which is created along a particular ray of projection. This thickened slab consists of variety of data including air, fat, fluid, vascular contrast, bone, etc., which can be postprocessed by different algorithms including maximum intensity projection (MIP), minimum intensity projection (minIP), average intensity projection (AIP), ray sum and volume rendering to give relevant required information. Curved planar reformation (CPR) is another important type of MPR. CPR is specifically used to study an anatomical structure like blood vessels in their respective entire course. Such formations are acquired by first targeting the specific anatomic structure and then aligning the imaging plane along that particular structure. Apart from blood vessels, other tubular structures including ureter and long length of intestine can be reconstructed and thus facilitating their study. Such reformations can help in disease characterization involving these tubular structures like narrowing or any intraluminal structural anomaly. Manual creation of such reformation can be a tedious process and can also produce certain pseudolesions. However, certain automated methods can be used to decrease a significant percentage of user interaction time and still provide reasonably good images. Being one of the algorithms used to thicken MPRs, the fundamental application of AIP is for characterizing the internal structures of a solid organ or the walls of hollow structures (e.g., blood vessels, intestine). It basically represents the average of each component attenuation value encountered by a ray cast through an object towards the viewer’s eye. A subtype of AIP called ‘ray sum’ is used in which the appearance similar to the conventional radiograph can be obtained by summing up the attenuation value of each voxel along the projection line. For, e.g., this technique can be used to obtain frontal or lateral chest X-ray projection-like images, which are beneficial in better visualization and characterization of X-ray findings. MIP is one of the commonly employed techniques in routine day to day imaging. MIP images show only the highest attenuation values within the voxel on every view throughout the volume on to a 2D image. Commonly used for CT angiography and CT urography, i.e., the contrast-filled structures as this application is most beneficial in demonstrating the brightest objects in the image. Another essential use is for detection of small lung nodules which are best visualized on MIP images rather than routine lung window (these nodules can indicate infective, inflammatory or neoplastic aetiologies). Thick slab MIP (>10 mm) may cause obscuration of small structures and hence thin slab MIPs (<10 mm) are preferable. Depth perception is suboptimal and hence anatomical or 3D relations can be difficult to decipher. This technique can result in loss of information and artefacts as high-density materials (calcification and metallic stents or prosthesis) can mask or obscure information about intravascular contrast material and lead to erroneous diagnosis. minIP is a relatively uncommonly employed data visualization method that enables detection of low-density structures in a given volume. minIP images are obtained on projecting the voxel with the lowest attenuation value on every view throughout the volume onto a 2D image. It basically demonstrates the organs filled with air on CT. To assess airways, areas of air trapping in lung and small airway disease for diagnosis of pathologies as well as surgical planning in a few cases. It may be used to visualize the biliary tract and pancreatic duct. Multiple varied mathematical algorithms are used to reassemble and edit and produce various 3D medical images. The algorithms are useful to give a specific ‘sense of depth’ to the 2D raw data which was initially acquired. 3D reconstruction of data offers many benefits like the following:
2.20: CT imaging protocol
General considerations and patient identification
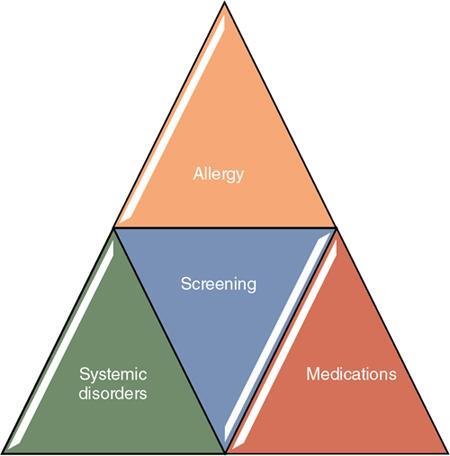
Clinical history and screening
Drugs
Medical Condition
Concern
Recommendation
Asthma
Increased risk of allergic like contrast reaction and bronchospasm
Premedication or restricted use of contrast media is not recommended
Renal insufficiency
Increased risk of contrast-induced nephrotoxicity
Need of screening
Contrast dose reduction and alternative contrast media if applicable
Cardiac status
Moderate to severe cardiac disease causes modest increase risk of a cardiac event
Restriction of contrast media and premedication is not recommended
Anxiety
Can precipitate mild adverse effects or contrast reactions as per few studies
Reassurance and thorough patient communication may be helpful in lowering these incidents
Sickle-cell trait/disease
Increased risk of acute sickle crisis on exposure to contrast medium
Such instances have not been reported with modern iodinated contrast media
Myasthenia gravis
Contrast medium causing exacerbations of myasthenic symptoms is controversial issue
Contrast medium as a relative contraindication in these patients is debatable
Hyperthyroidism
Patients with acute thyroid storm
Iodinated contrast may precipitate or worsen thyrotoxicosis
Radioactive iodine imaging/radioactive iodine therapy for thyroid gland
The iodinated contrast impedes the uptake of diagnostic or therapeutic dose.
Advisable to keep a washout period of at least 3–4 weeks for diminishing this interaction for hyperthyroid patient and 6 weeks for hypothyroid patient
Preprocedural investigations and fasting
CONDITIONS THAT DEMAND MANDATORY ASSESSMENT OF RENAL FUNCTIONS PRIOR TO CONTRAST ADMINISTRATION
Age > 60 years
History of hypertension requiring medical therapy
A patient with renal disease ± dialysis
History of diabetes mellitus
Renal transplant/Single kidney
Metformin or metformin-containing drug combinations
Renal cancer
Renal surgery
Consent/patient information form
Pregnancy and breastfeeding
Metformin
Category
Renal Status
Implication
I
No evidence of acute kidney injury and eGFR ≥ 30 mL/min/1.73 m2
II
Past H/O acute kidney injury or severe CKD (eGFR< 30)
Premedication
Elective premedication (12- or 13-hour oral premedication)
Accelerated IV premedication (in decreasing order of desirability)
Sedation and anaesthesia (NORA – nonoperating room anaesthesia)
Unique considerations in children
Contrast in children
Alara principle in paediatric radiology
Brief about specialized preparations for different regional scans
Basic preparedness from technician’s perspective/checklist for technologist prior to commencement of scan
Introduction
Postprocessing techniques
(a) Morphological or anatomical postprocessing techniques
Basic techniques
Multiplanar reformation
Curved planar reformation
Advantage
Disadvantage
Advanced techniques
Average intensity projection
Maximum intensity projection
Applications/advantages
Disadvantages
Minimum intensity projection
Applications
3D reconstruction techniques
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








