Key Points
- ▪
Coronary artery bypass grafts are amenable to cardiac CT angiography assessment because they are larger in size than native arteries and are subject to little motion artifact and little calcification, factors that otherwise present major limitations to CCT.
- ▪
The abundance of surgical clips on internal thoracic and mammary grafts is an impediment to adequate CCT angiography.
- ▪
Unfortunately, the need to assess native coronary artery disease, which is always advanced in patients who have had a prior bypass, renders coronary graft assessment only a portion of the necessary evaluation.
- ▪
However, CCT coronary graft angiography may be useful in well-chosen cases, such as mapping graft course in cases where reoperation is anticipated.
Coronary Bypass Graft Assessment
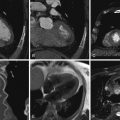
Coronary bypass grafts, both venous and arterial, are more readily evaluated by CT angiography (CTA) than are coronary arteries, because of:
- □
Their large diameter (more so for venous than arterial conduits)
- □
Their minimal motion, when compared with coronary arteries, because they are largely extracardiac
- □
Their general lack of calcification, versus the common and often extensive calcification of native coronary arteries
- □
Simpler courses (but not always) with little overlap. Some exceptions:
- •
Posterior transverse sinus course of a venous graft or right internal mammary artery (RIMA) graft to the circumflex
- •
Twisted course of vein grafts if multiple and adjacent
- •
The presence of jump-grafts (sequential graft insertions; usually saphenous)
- •
Internal thoracic artery positioned tightly against the chest wall, in which case the use of bone extraction software when post-processing may eliminate depiction of the internal mammary artery (IMA) graft
- •
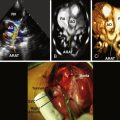
Potential Uses of Coronary CTA in Patients with Coronary Artery Bypass Grafts
- □
Nonvisualization of a coronary artery bypass graft (CABG) at the time of catheter angiography
- □
Chest pain in a patient with CABG
- □
Prior to repeat open heart surgery (CABG or valve surgery), to localize the bypass grafts relative to the sternum and intended sternotomy
Problems with Bypass Graft Assessment
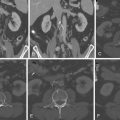
- □
The large field of view. This is especially true if there is an internal thoracic artery to be imaged, because the field of view will extend from above the subclavian artery down to the diaphragm. This requires:
- •
Longer breath-hold and greater chance for motion artifact
- •
Greater radiation exposure
- •
- □
Surgical clips abound around mammary arteries and may present a challenge and sometimes a problem when the adjacent lumen is being imaged.
- □
Sternal wires also may cause artifacts, as may ECG electrodes, which can confound assessment of anterior bypass grafts.
- □
The direction of flow within a graft cannot be established by its opacification. It is tempting to view opacification as indicative of anterograde flow. This becomes a problem, however, when there is a proximal severe-appearing lesion: assumption of anterograde filling implies nonocclusion, whereas retrograde filling of a proximally occluded graft may have been the case.
- □
If a left internal thoracic artery graft is present, the contrast will have to be injected via the right arm to avoid high-attenuation artifacts in the left subclavian artery; such artifacts may confound imaging of the ostium of the internal thoracic artery.
- □
If both the left and right internal thoracic arteries are used as conduits, then the ostium of one of the two will be obscured by subclavian vein overattenuation artifacts.
- □
Often a larger concentration of metallic clips is seen at the graft-native vessel anastomosis, resulting in a beam-hardening artifact and obscuring the depiction of the anastomosis.
- □
Cardiac CT (CCT) is better at assessing bypass grafts than native vessels, which are, of course, always diseased in the scenario of bypass grafting, often extensively, and may be calcified. Adequate and complete visualization of the native vessels distal to the bypass graft anastomosis may be (often is) problematic, because the native coronary arteries at this level tend to be smaller.
- □
Stenting within bypass grafts is still a challenge; however, stents within grafts often are better assessed than native stented vessels due to the larger size of the grafts and less cardiac motion.
- □
Interobserver agreement of quantification of lesions is poor: less than 50%.
- □
For more information, see Tables 8-1 and 8-2 .
TABLE 8-1
Cardiac CT Assessment of Coronary Artery Bypass Grafts
AUTHOR
JOURNAL
YEAR
CT
NO. PTS/NO. GRAFTS
NONASSESS. (%)
GRAFT TYPES (SVG:IMA)
LESION
SENSITIVITY (%)
SPECIFICITY (%)
PPV (%)
NPV (%)
Achenbach et al.
Am J Cardiol
1997
EBCT
25
4
55:1
Occlusion
100
100
16
Stenosis
100
97
Chiurlia et al.
Am J Cardiol
2005
16-CT
52
99
117:47
Occlusion
100
100
Stenosis
96
100
Martuscelli et al.
Circulation
2004
16-CT
96
166:85
Occlusion
100
100
Stenosis
90
100
84
Anastomosis
97
100
Nieman et al.
Radiology
2003
4-CT
109
16
93
42
70
81
Ropers et al.
Am J Cardiol
2001
MSCT
65
0
162:20
Occlusion
97
98
97
98
38
Stenosis
75
92
71
93
Schlosser et al.
JACC
2004
16-CT
51
0
91:40
96
95
81
99
Anders et al.
Eur J Radiol
2006
16-CT
32
18
74:19
Occlusion
100
98
Stenosis
81
87
Salm et al.
Am Heart J
2005
16-CT
25
8
53:14
Occlusion
100
100
100
100
8
53:14
Stenosis
100
94
50
100
Moore et al.
Clin Radiol
2005
50
0%
Occlusion
100
100
0%
Stenosis
100
99
Burgstahler et al.
Int J Cardiol
2006
16-CT
0
43 g
Occlusion
100
100
100
5
Stenosis
100
93
100
Schuijf et al.
Am J Cardiol
2004
16-CT
1
43 g
Occlusion
96
100
99
15
Stenosis
100
96
100
Pache et al.
Eur Heart J
2006
64-CT
0
93 g
Occlusion
100
100
100
6
Stenosis
100
100
100
Stauder et al.
Eur Radiol
2006
16-CT
20
22.5
80 art
Stenosis
96
97
96
97
7.3
180 svg
Stenosis
99
94
92
99
31
Native
Stenosis
92
77
88
85
Malagutti et al.
52/109
Grafts
99
96
Native
89
93
50
Ropers et al.
Graft occlusion
Graft stenosis
Native arteries
0
0
9
100
100
86
100
94
76
100
92
44
100
100
96
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree