Anatomy, embryology, and pathophysiology
Anatomy
- ◼
The kidneys are paired, bean-shaped, retroperitoneal organs that primarily function in the excretion of metabolic waste.
- ◼
The concave medial surface is known as the renal hilum.
- ◼
Each collecting system consists of the minor calyces, major calyces (infundibula), and renal pelvis. There are 10 to 25 minor calyces in each kidney.
- ◼
The perirenal space is confined by the anterior (Gerota) and posterior (Zuckerkandl) renal fascia.
Embryology
- ◼
The renal parenchyma arises from the metanephros (a derivative of the mesoderm) in the fifth week of gestation.
- ◼
The collecting system arises from the mesonephric duct and ureteric bud in the fourth week of gestation.
- ◼
Development takes place in the pelvis followed by migration into the abdomen.
- ◼
In the setting of horseshoe kidney, the fused lower renal poles become caught on the inferior mesenteric artery and remain low in the abdomen.
Physiology
- ◼
Supplied by a single renal artery arising from the abdominal aorta.
- ◼
Near the renal hilum, the main renal artery divides into one posterior and four anterior segmental renal arteries (upper, apical, middle, and lower) that course through the renal sinus.
- ◼
The segmental arteries give rise to the lobar arteries that branch to form the interlobar, arcuate, and interlobular arteries.
- ◼
Accessory renal arteries can occur, and are unilateral in 30% and bilateral in 10%.
- ◼
The kidney is usually drained by a single renal vein.
- ◼
Variant venous anatomy includes multiple right renal veins (30%), a circumaortic left renal vein (17%), and a retroaortic left renal vein (3%).
Techniques
Ultrasonography
- ◼
Many renal lesions are initially identified and characterized with ultrasound.
- ◼
Longitudinal and transverse images are obtained sequentially through the upper pole, interpolar region, and lower pole of each kidney.
- ◼
The perirenal areas, retroperitoneum, and bladder are imaged for completion.
- ◼
Color Doppler and spectral waveform analysis may be performed.
- ◼
The kidney is surrounded by an echogenic fibrous capsule and perirenal fat.
- ◼
The renal cortex is normally equal or slightly less echogenic than the adjacent liver and spleen.
- ◼
The renal sinus is composed of echogenic fat.
Computed tomography
- ◼
Computed tomography (CT) is the primary imaging modality used in evaluation of the cystic renal mass.
- ◼
Typically, a three-phase examination is performed, beginning with an unenhanced phase followed by the administration of an iodinated contrast medium.
- ◼
The corticomedullary phase (40 second delay) differentiates between the markedly enhancing renal cortex and relatively unenhanced renal medulla.
- ◼
The nephrographic phase (90–120 second delay) demonstrates homogenous renal parenchymal enhancement.
- ◼
The delayed (excretory/pyelographic) phase (6–10 minute delay) shows excretion of contrast into the collecting system with progression into the ureters and bladder.
- ◼
- ◼
An increase in attenuation by at least 15 to 20 HU in a renal lesion from the unenhanced to the postcontrast phases is considered enhancement.
- ◼
Dual energy CT offers improved evaluation for enhancement by providing material decomposition images to display actual iodine uptake on postcontrast images. It may also serve to decrease radiation dose by creation of a virtual unenhanced image on multiphase acquisitions.
Magnetic resonance imaging
- ◼
Increasingly used as a problem-solving tool when CT and/or ultrasonography is not definitive.
- ◼
T1-weighted sequences are helpful to depict hemorrhage and protein, whereas T2-weighted sequences often demonstrate septa and nodules.
- ◼
Postgadolinium images are used to identify enhancement, particularly in cases with indeterminate enhancement on CT. Subtraction images are especially useful in clarifying enhancement, provided that the reader is aware of potential misregistration artifact.
- ◼
Magnetic resonance imaging (MRI) is relatively insensitive in detecting calcification.
Protocols
Computed tomography
Multiphase imaging in the evaluation of a cystic renal mass should include thin-slice unenhanced and postcontrast imaging in the corticomedullary and nephrographic phases. An excretory phase may be performed to define the relationship between a cystic mass and the renal collecting system or to evaluate for potential urinary complications following nephrectomy or cryoablation.
Magnetic resonance imaging
Similarly, multiphase imaging of the kidneys is performed on MRI with the added benefit of no ionizing radiation. Subtraction imaging is helpful in differentiating enhancement from intrinsic blood products or proteinaceous debris. Diffusion-weighted imaging should be performed to evaluate for areas of hypercellularity, which can aid in the diagnosis of solid components in cystic renal cell carcinoma.
Classification system for cystic renal masses
Bosniak criteria for renal cysts
- ◼
An approach to renal cysts that attempts to categorize each cyst as benign/nonsurgical, probably benign but requires follow-up, and suspicious/surgical.
- ◼
Limitations include interobserver variation, particularly in categorizing category II and III lesions.
- ◼
Although originally based on CT findings, the Bosniak classification has been successfully applied to both contrast-enhanced MRI and ultrasonography.
- ◼
The most worrisome features should guide lesion classification and management.
I (simple benign cyst)
- ◼
Hairline thin wall without septa, calcifications, or solid components.
II (benign minimally complicated cyst)
- ◼
May contain few hairline thin septa, which may enhance.
- ◼
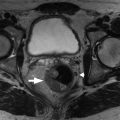
Fine calcification or a short segment of slightly thickened calcification may be present in the wall or septa ( Fig. 23.1 ).

Fig. 23.1
Axial unenhanced (A) and coronal contrast-enhanced (B) computed tomography images show benign calcifications along the wall of a right renal cyst. There is no wall thickening, mural nodularity, or measurable enhancement.
(From Sahani DV, Samir AE. Abdominal Imaging, ed 2. Philadelphia: Elsevier, 2017.)
- ◼
Uniformly high-attenuation lesions smaller than 3 cm are also included in this category.
IIF
- ◼
May contain multiple hairline-thin septa or minimally thickened and smooth wall or septa.
- ◼
Calcification and perceived enhancement of the wall or septa may be present ( Fig. 23.2 ).