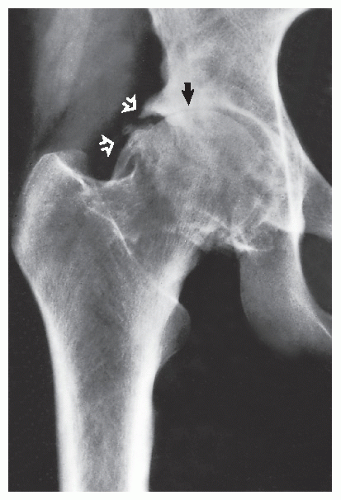
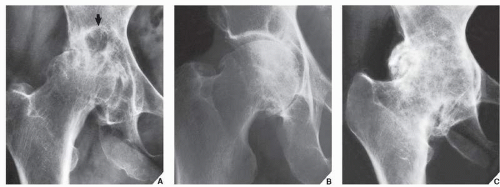
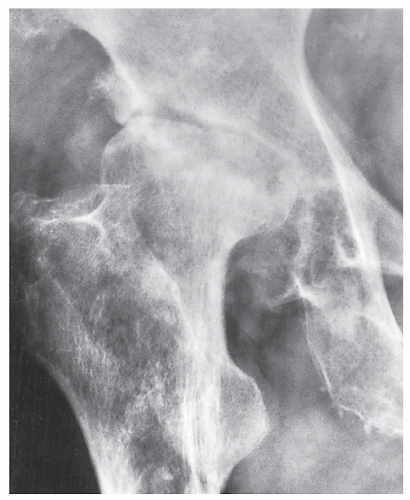
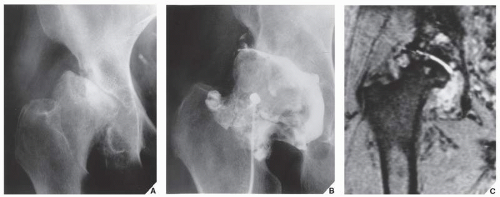
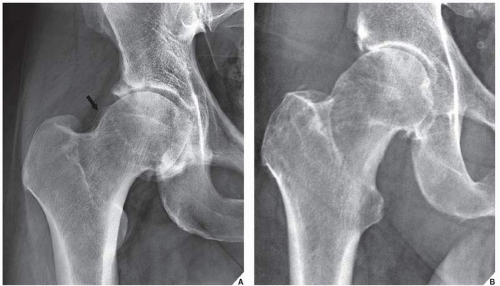
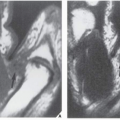
Narrowing of the joint space as a result of thinning of the articular cartilage
Subchondral sclerosis (eburnation) caused by reparative processes (remodeling)
Osteophyte formation (osteophytosis) as a result of reparative processes in sites not subjected to stress (so-called low-stress areas), which are usually marginal (peripheral) in distribution
Cyst or pseudocyst formation resulting from bone contusions that lead to microfractures and intrusion of synovial fluid into the altered spongy bone; in the acetabulum, these subchondral cystlike lesions are referred to as Eggers cysts.
inflammatory process. Thus, one may see secondary osteoarthritis with axial migration (Fig. 13.5).
 FIGURE 13.1 Highlights of the morphology and distribution of arthritic lesions in primary osteoarthritis. |
TABLE 13.1 Clinical and Radiographic Hallmarks of Degenerative Joint Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
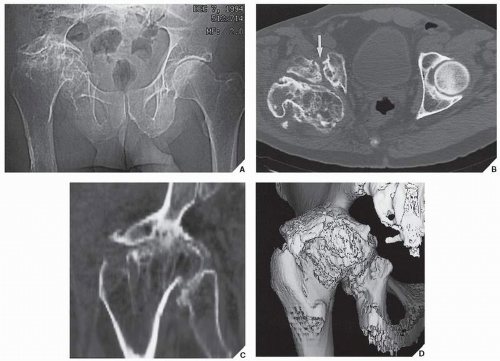
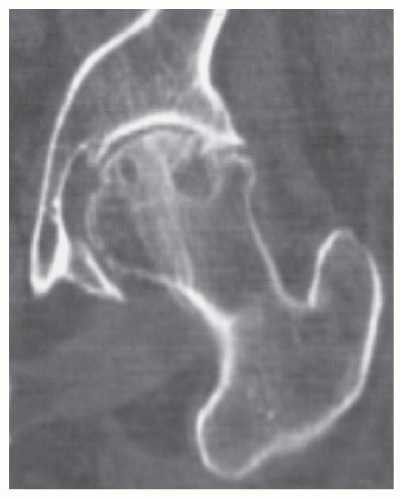 FIGURE 13.3 CT of osteoarthritis of the hip. Coronal reformatted image shows diminution of the joint space, osteophytes, and subchondral cysts in the femoral head. |
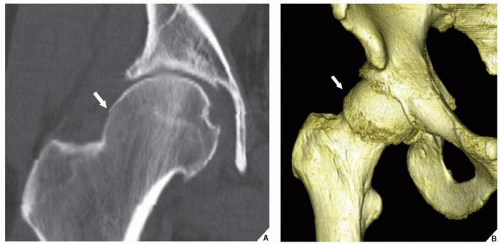
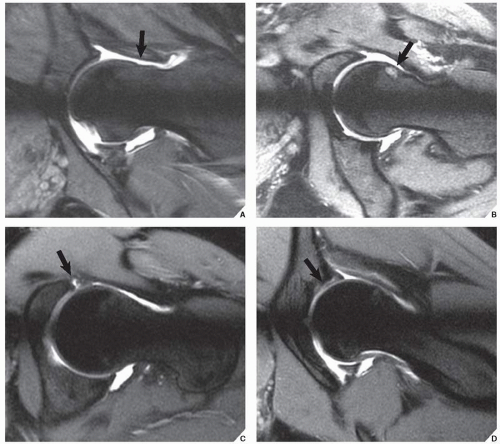
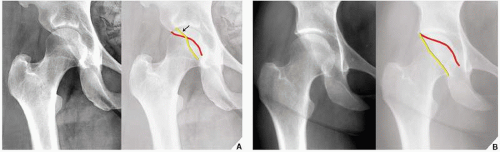
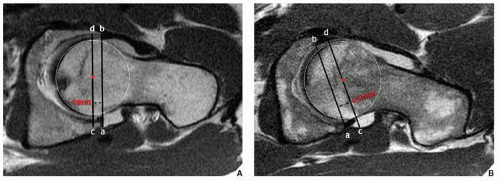
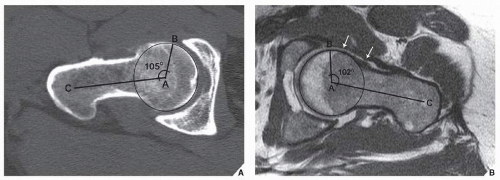
lateral projection of anterior acetabulum, which normally should project medially to the posterior acetabulum, “crosses” the posterior acetabular outline (Fig. 13.12). MRI demonstrates acetabular version and depth of the femoral head coverage (Fig. 13.13). To determine the sphericity of the femoral head and the prominence of the anterior femoral head/neck junction, the alpha angle is calculated on the oblique axial CT or oblique axial MR images (Fig. 13.14). Radial reformatted MR images are of particular value in this respect, because they allow optimal visualization of the anterosuperior region of the femoral head/neck junction, where the most significant changes in the alpha angle occur (see Fig. 13.14B). The normal alpha angle should not exceed 50 degrees. The larger the alpha angle, the more pronounced is nonspherical shape of the femoral head, and the greater is predisposition for anterior FAI.
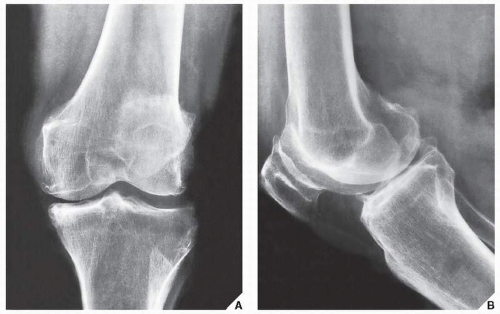
bodies, which can be demonstrated on the standard projections of the knee (Figs. 13.18 and 13.19); however, MRI may also be effective in this respect (Figs. 13.20,13.21,13.22). The femoropatellar joint compartment is also commonly involved in primary osteoarthritis. The lateral radiograph of the knee and axial view of the patella are the most effective means of visualizing degenerative changes of the femoropatellar compartment (Fig. 13.23).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree