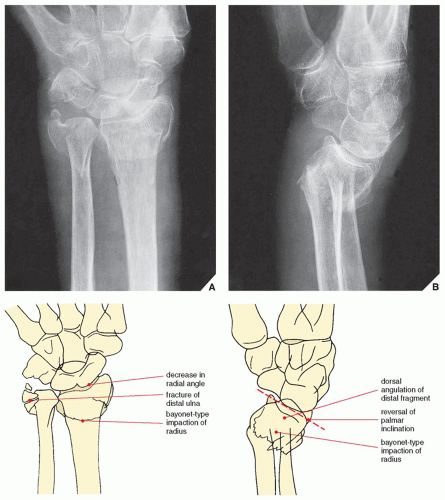
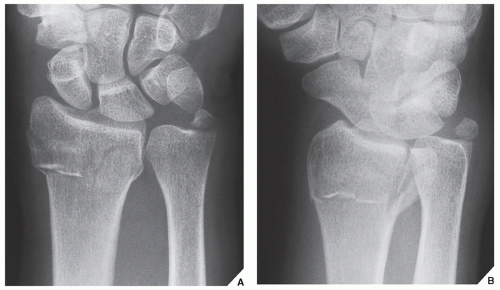
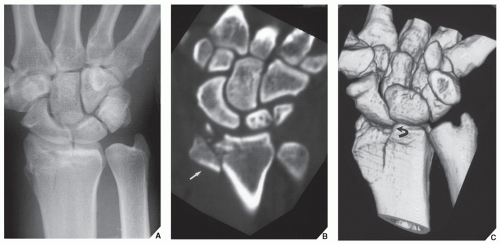
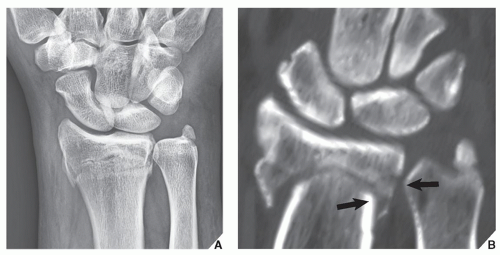
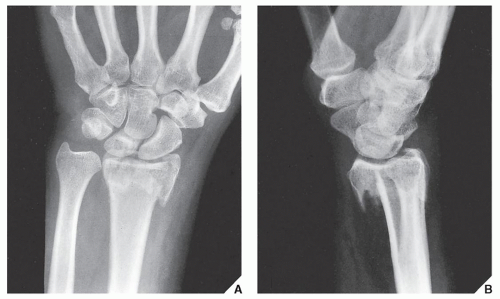
to impaction or bayonet-type displacement (Figs. 7.11 and 7.12). CT scanning may provide additional information concerning the exact position of displaced fragments (Figs. 7.13, 7.14, 7.15).
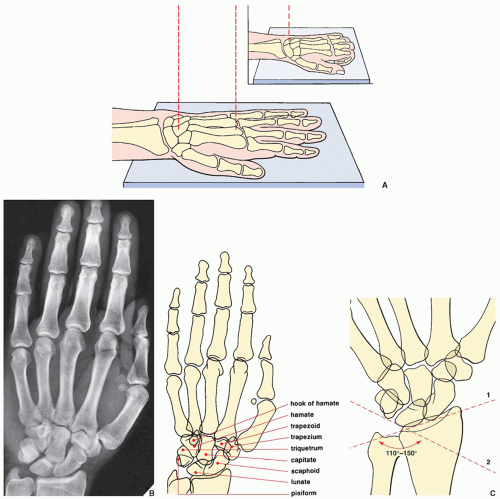
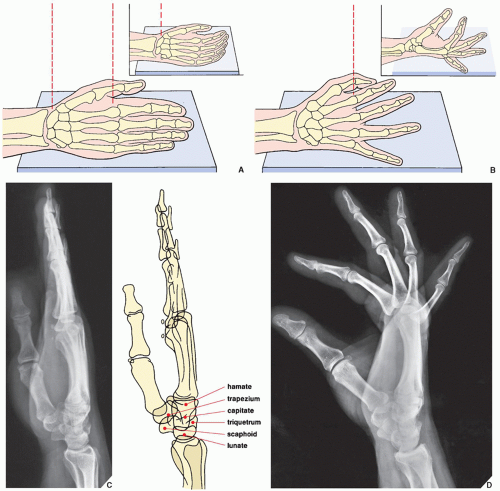 FIGURE 7.2 Lateral view of the wrist and hand. (A) For the lateral projection of the wrist area and the hand, the patient’s arm is fully extended and resting on its ulnar side. The fingers may be fully extended or, preferably, slightly flexed (inset), with the thumb slightly in front of the fingers. For the evaluation of the wrist area, the central beam is directed toward the center of the carpus, while for the hand, it is directed toward the head of the second metacarpal (B). On the radiograph obtained in this projection (C), the distal radius and the ulna overlap, but the relation of the longitudinal axes of the capitate, the lunate, and the radius can sufficiently be evaluated (see Fig. 7.84). Although the metacarpals and the phalanges also overlap, dorsal or volar displacement of a fracture of these bones can easily be detected (see Fig. 4.1). The thumb is imaged in true dorsovolar projection. A more effective way of imaging the fingers in the lateral projection is to have the patient spread the fingers in a fan-like manner, with the ulnar side of the fifth phalanx resting on the film cassette. The central beam is directed toward the heads of the metacarpals. (D) On the film in this projection, the overlap of the phalanges commonly seen on the standard lateral view is eliminated. The interphalangeal joints can readily be evaluated. |
TABLE 7.1 Standard Radiographic Projections for Evaluating Injury to the Distal Forearm | ||||||
|---|---|---|---|---|---|---|
|
TABLE 7.2 Ancillary Imaging Techniques for Evaluating Injury to the Distal Forearm | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||
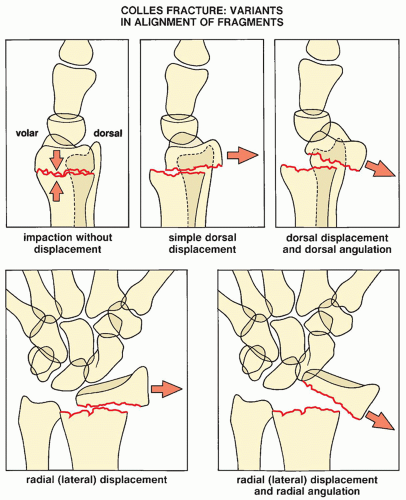 FIGURE 7.9 Colles fracture. Five variants of displacement and angulation of the distal fragment in Colles fracture. Some of these patterns may occur in combinations, yielding a complex deformity. |
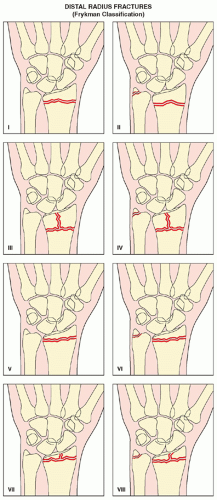
TABLE 7.3 Frykman Classification of Distal Radius Fractures | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
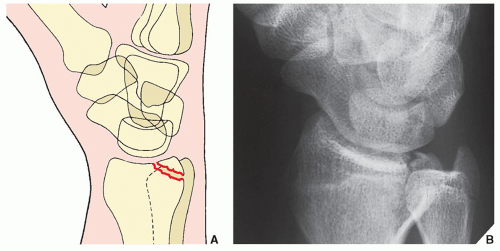
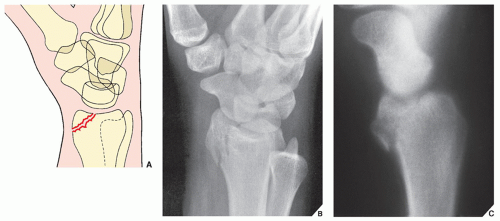
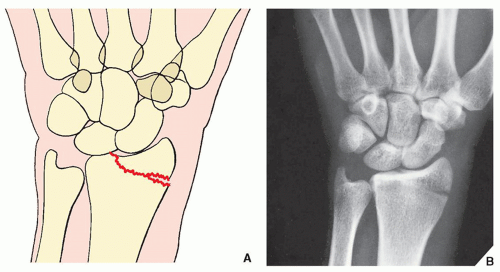
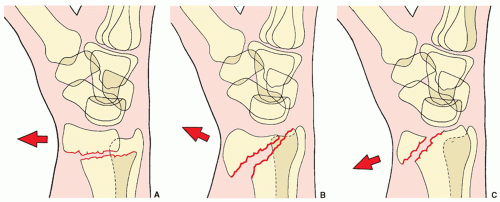 FIGURE 7.20 Smith fracture. The three types of Smith fracture are distinguished by the obliquity of the fracture line. Volar displacement of the distal fragment is characteristic of all three types. (A) In Smith type I, the fracture line is transverse, extending from the dorsal to the volar cortices of the radius. (B) The oblique fracture line in type II extends from the dorsal lip of the distal radius to the volar cortex. (C) Type III, which is almost identical to the reverse Barton fracture (see Fig. 7.17), is an intraarticular fracture with an extension to the volar cortex of the distal radius. |
such as those described in the preceding sections or independently after an injury to the distal forearm and wrist.
 FIGURE 7.25 Ulnar impingement syndrome. Posteroanterior radiograph of the wrist shows a negative ulnar variance. The distal ulna impinges on the medial cortex of distal radius. |
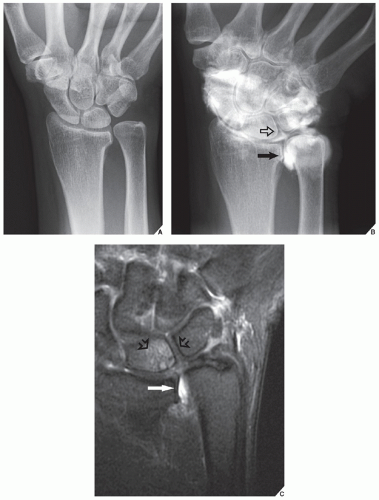
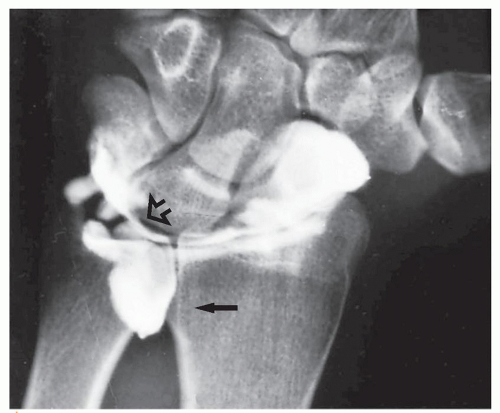 FIGURE 7.30 Arthrography of a TFCC tear. A single-contrast arthrogram of the wrist shows a leak of contrast into the space occupied by the triangular cartilage (open arrow), with characteristic filling of the distal radioulnar compartment (arrow), confirming a tear of the TFCC (compare with Fig. 7.7B). |
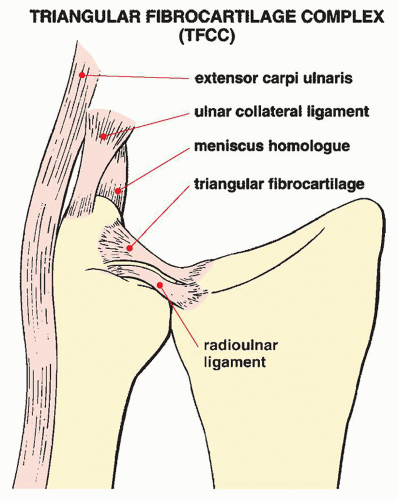
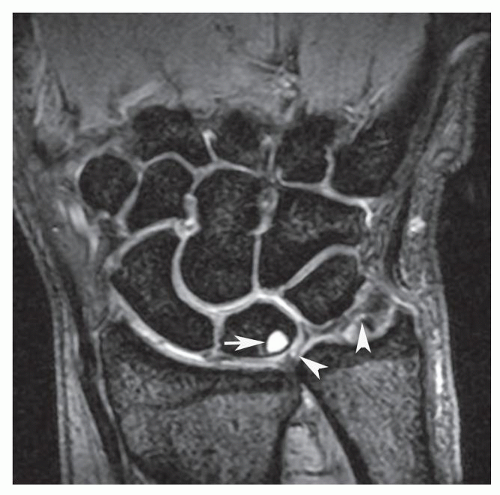
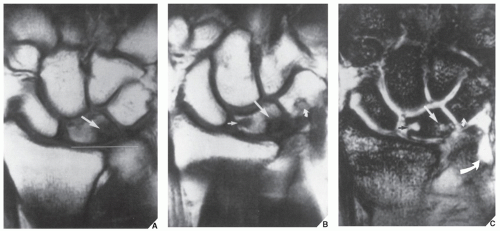
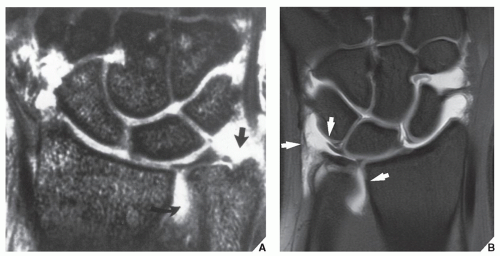
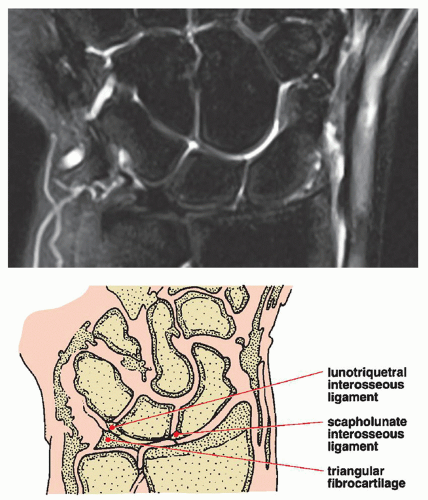
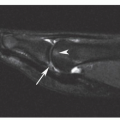
lunate bones (Fig. 7.31; see also Fig. 7.8). Tears of the TFCC manifest as discontinuities and fragmentation of this structure. The torn fibrocartilage becomes irregular in contour and is interrupted by high-signal intensity areas on T2-weighted images (Fig. 7.32). However, one of the studies published by Haims and colleagues questions the sensitivity of MRI in diagnosing peripheral tears of the triangular fibrocartilage. In this respect, the authors reported the sensitivity of MRI of only 17%, with a specificity of 79%, and accuracy of 64%.
Dorsovolar obtained in ulnar deviation of the wrist for the evaluation of the scaphoid bone, which appears foreshortened on the standard dorsovolar projection as a result of its normal volar tilt (Fig. 7.33)
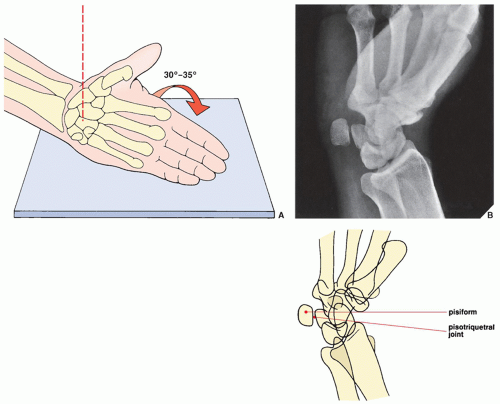
Supinated oblique for visualizing the pisiform bone and the pisotriquetral joint (Fig. 7.34)
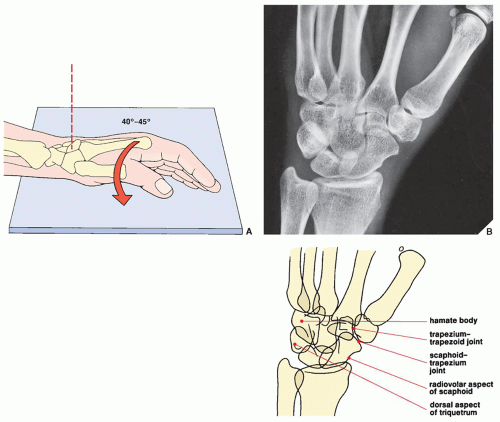
Pronated oblique for imaging the triquetral bone, the radiovolar aspect of the scaphoid, and the radial styloid process (Fig. 7.35)
Carpal tunnel for demonstrating the hook of the hamate, the pisiform, and the volar aspect of the trapezium (Fig. 7.36)
combined with arthrography (see Fig. 2.19) or can be enhanced by an intravenous contrast material. It is effective in demonstrating subluxation in the distal radioulnar joint and in evaluating the so-called humpback deformity of the scaphoid, osteonecrosis of the lunate (Kienböck disease), and fractures of the hook of the hamate, among other abnormalities. Axial sections are obtained after positioning the patient prone with the arm extended above the head. Contiguous sections of 1 or 2 mm are acquired, preferably using a spiral (helical) technique. Direct coronal sections can also be obtained with the wrist in maximal volar flexion or dorsal extension.
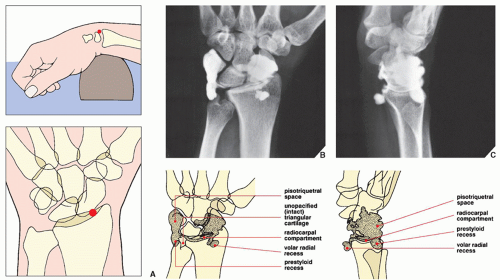
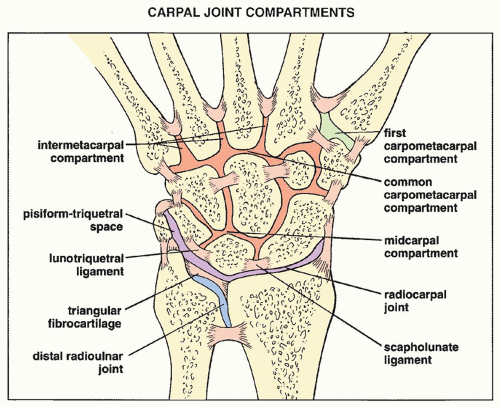 FIGURE 7.37 Compartments of the carpus. Carpal joint compartments are separated from one another by various interosseous ligaments. |
view is recommended. This technique may image not only abnormalities of the soft tissues, including various muscles, tendons, interosseous ligaments, and triangular fibrocartilage, but also osseous abnormalities such as occult fractures and early osteonecrosis, particularly of the lunate and scaphoid. It is also very useful in imaging the carpal tunnel (Fig. 7.39) and detecting the subtle abnormalities of carpal tunnel syndrome (Fig. 7.40; see also Fig. 7.115) and Guyon canal syndrome (see Fig. 7.116). Commonly, MRI is performed after an intraarticular injection of a contrast agent (diluted gadolinium) into the radiocarpal compartment (see Fig. 7.31).
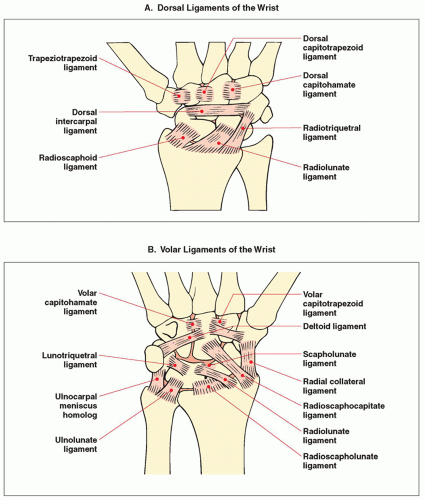 FIGURE 7.41 Ligaments of the wrist. A schematic representation of the dorsal (A) and volar (B) ligaments of the wrist. |
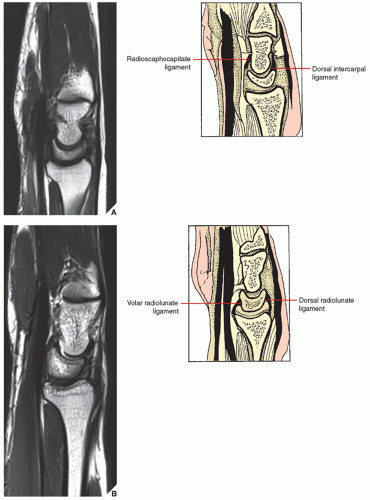 FIGURE 7.42 MRI of the wrist. Sagittal MRI through the wrist from the midaspect (A,B) to the ulnar aspect (C,D). The volar and dorsal radiolunate components of the radioscapholunate ligaments are well demonstrated. The radiolunotriquetral ligament is seen volar to the capitate-lunate articulation. The radioscaphocapitate ligament is seen inserting at the volar and proximal one third of the capitate bone.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|