Congenital Elevation of the Scapula
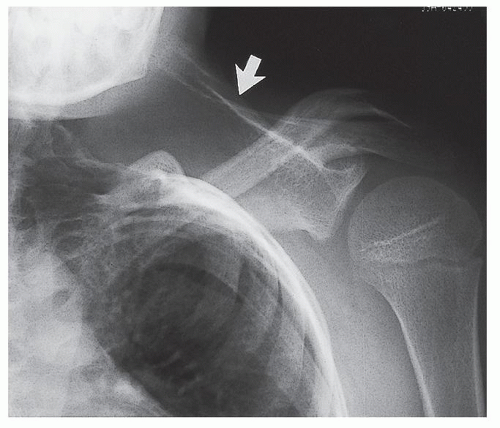
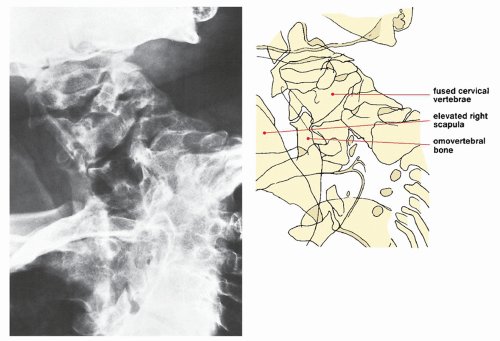
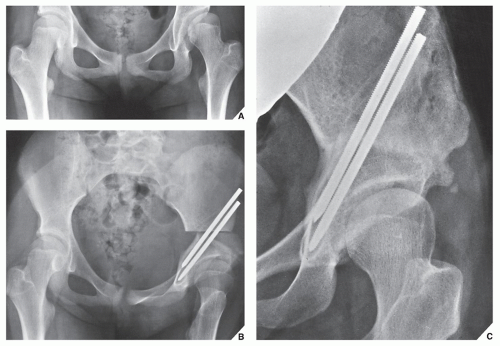
Sprengel deformity, as congenital elevation of the scapula is also known, may be unilateral or bilateral. It is marked by the appearance of a scapula that is small, high in position, and rotated with its inferior edge pointing toward the spine—features that are easily identified on an anteroposterior radiograph of the shoulder or chest (
Fig. 32.1). The left shoulder is the most commonly affected, and about 75% of all cases are observed in girls. Some cases of this anomaly are inherited in an autosomal dominant manner, although most cases are sporadic. A familial form of the Sprengel deformity is known as
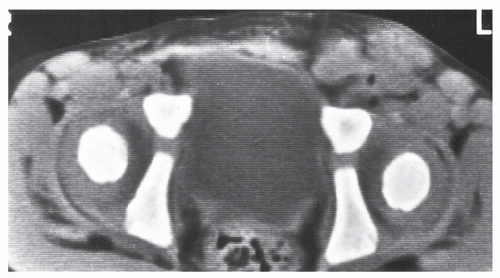
Corno disease. The finding of a congenitally elevated scapula is important because of this condition’s frequent association with other anomalies, such as congenital scoliosis, fused ribs, spina bifida, and fusion of the cervical or upper thoracic vertebrae, the latter deformity known as
Klippel-Feil syndrome, also a congenital disorder (
Fig. 32.2) caused by mutations in the
GDF3 and
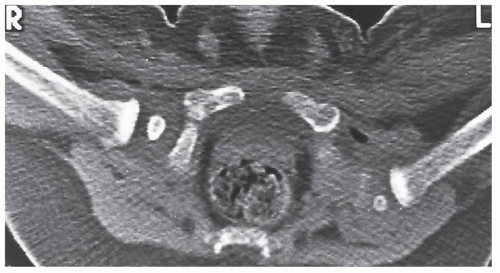
GDF6 genes. Furthermore, there is sometimes a bony connection between the elevated scapula and one of the vertebrae (usually the C5 or C6 vertebra), creating what is known as the
omovertebral bone (
Fig. 32.3).
Madelung Deformity
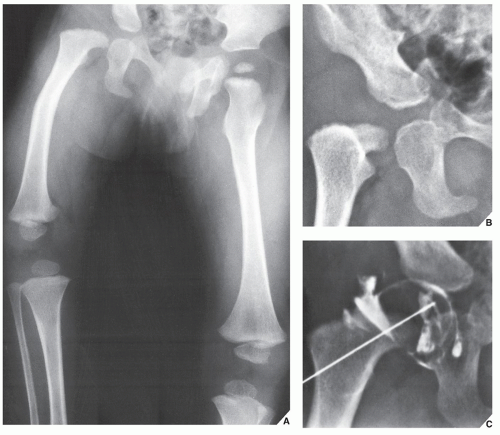
This developmental anomaly of the distal radius and carpus, originally described by the German surgeon Otto Madelung in 1879, usually manifests in adolescent girls presenting with pain in the wrist and decreased range of motion but with no history of previous trauma or infection. Today, the term Madelung deformity is often used to describe a variety of conditions in the wrist marked by premature fusion of the distal physis of the radius, with consequent deformity of the distal ulna and wrist. From the etiologic viewpoint, these abnormalities can be divided into posttraumatic deformities, dysplasias, and idiopathic conditions. A genetic cause has also been proposed. Association with mesomelic dwarfism (e.g., Leri-Weill dyschondrosteosis, caused by deletion or duplication of the SHOX gene located within the band Xp22.3 of the chromosome X) and a mutation on the X chromosome (e.g., Turner syndrome) has also been described. The posttraumatic deformity may occur after repetitive injury or after a single event that disrupts the growth of the distal radius. Among the bone dysplasias associated with Madelung deformity are multiple hereditary cartilaginous exostoses, Ollier disease, achondroplasia, multiple epiphyseal dysplasia, and the mucopolysaccharidoses including Hurler and Morquio syndromes.
On physical examination, the hand is translated volarly to the long axis of the forearm and there is dorsal subluxation of the ulna. A decreased range of motion limits supination, dorsiflexion, and radial deviation, but pronation and palmar flexion are usually preserved.
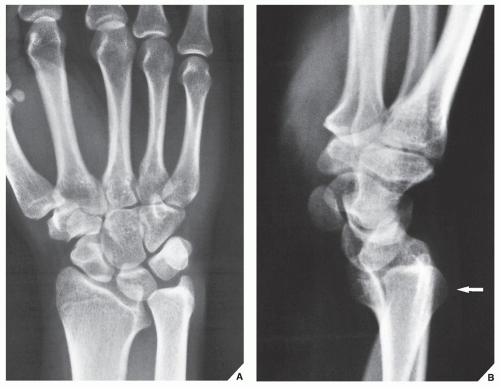
The radiographic criteria for the diagnosis of Madelung deformity were proposed by Dannenberg and colleagues (
Table 32.1). The posteroanterior and lateral projections of the distal forearm and wrist are sufficient to demonstrate any of the abnormalities associated with this deformity (
Figs. 32.4 and
32.5) .
Surgical treatment of Madelung deformity is indicated for pain relief and cosmetic improvement. A variety of procedures are available. These include ligament release (Vickers physiolysis), wedge osteotomy, Carter-Ezaki dome osteotomy, and radioscaphocapitate arthrodesis. Occasionally, a Darrach or a Suavé-Kapandji procedure is indicated.