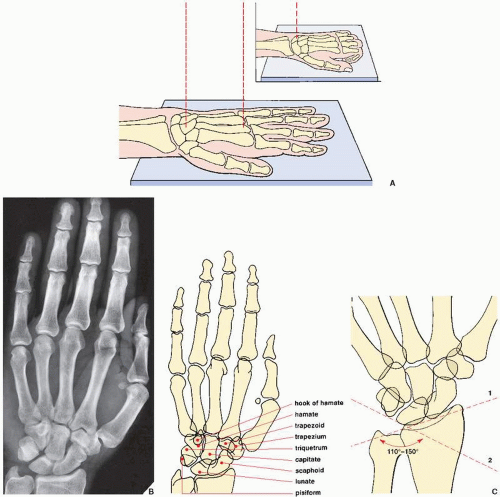
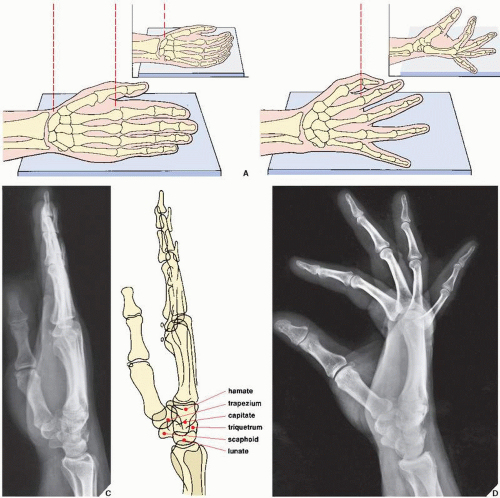
 FIGURE 7.2 Lateral view of the wrist and hand. (A) For the lateral projection of the wrist area and the hand, the patient’s arm is fully extended and resting on its ulnar side. The fingers may be fully extended or, preferably, slightly flexed (inset), with the thumb slightly in front of the fingers. For the evaluation of the wrist area, the central beam is directed toward the center of the carpus, while for the hand, it is directed toward the head of the second metacarpal (B). On the radiograph obtained in this projection (C), the distal radius and the ulna overlap, but the relation of the longitudinal axes of the capitate, the lunate, and the radius can sufficiently be evaluated (see Fig. 7.80). Although the metacarpals and the phalanges also overlap, dorsal or volar displacement of a fracture of these bones can easily be detected (see Fig. 4.1). The thumb is imaged in true dorsovolar projection. A more effective way of imaging the fingers in the lateral projection is to have the patient spread the fingers in a fan-like manner, with the ulnar side of the fifth phalanx resting on the film cassette. The central beam is directed toward the heads of the metacarpals. (D) On the film in this projection, the overlap of the phalanges commonly seen on the standard lateral view is eliminated. The interphalangeal joints can readily be evaluated. |
TABLE 7.1 Standard Radiographic Projections for Evaluating Injury to the Distal Forearm | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 7.2 Ancillary Imaging Techniques for Evaluating Injury to the Distal Forearm | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
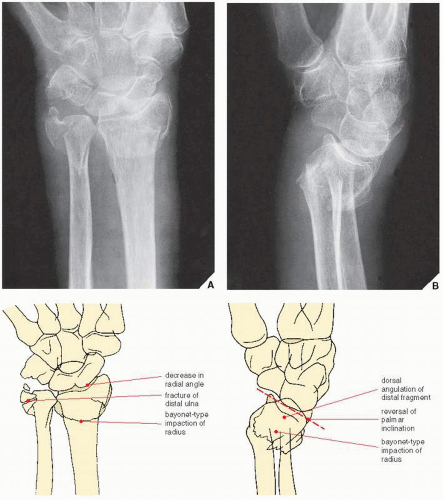
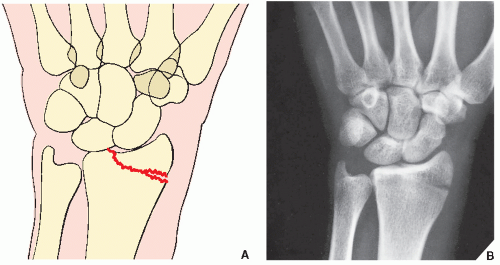
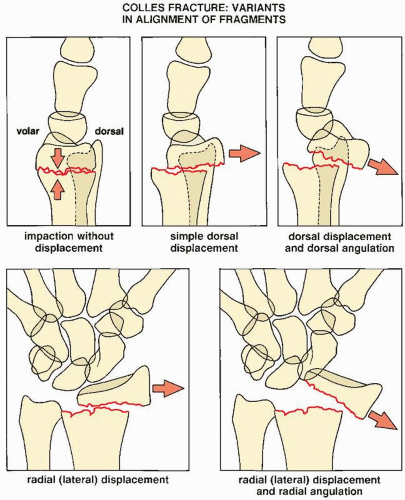 FIGURE 7.9 Colles fracture. Five variants of displacement and angulation of the distal fragment in Colles fracture. Some of these patterns may occur in combinations, yielding a complex deformity. |
fusion of the distal ulnar growth plate, or radial scalloping and radioulnar convergence, in cases of distal ulnar resection. Before these findings become obvious on conventional radiologic studies, magnetic resonance imaging (MRI) may be helpful in early recognition of this condition.
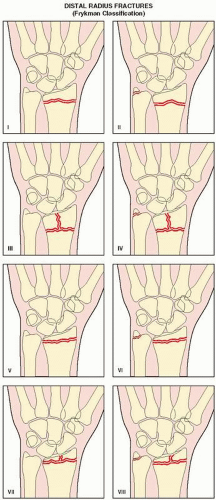
TABLE 7.3 Frykman Classification of Distal Radius Fractures | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
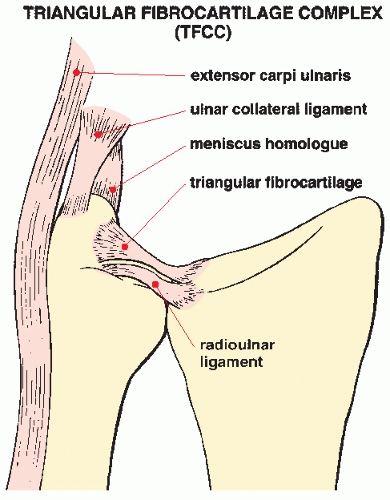
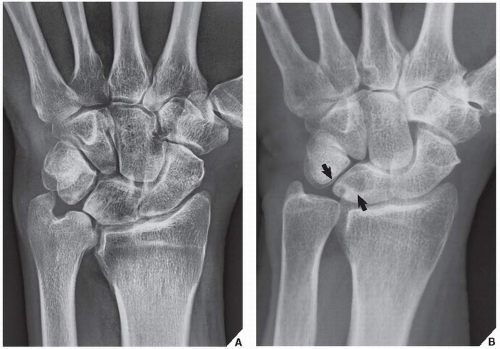
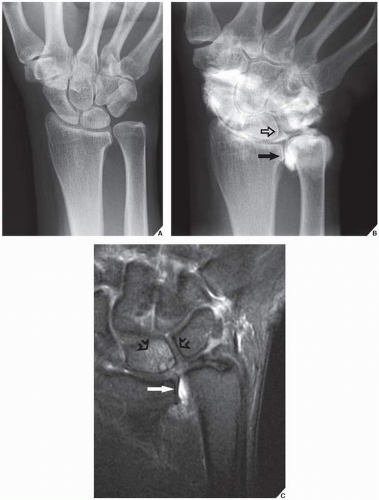
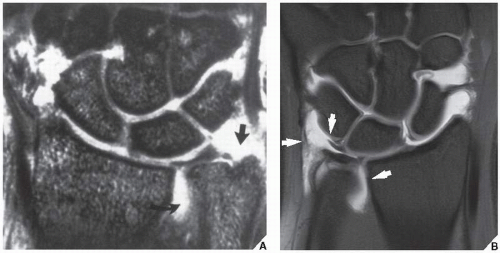
ulna on the medial surface of the lunate bone. This causes the development of degenerative changes in the cartilage covering both bones. In addition, frequent association of the tear of the triangular fibrocartilage has been reported. In cases of excessive ulnar length, dorsal subluxation of the ulna is present compromising supination of the forearm. The conventional radiography shows a positive ulnar variance associated with significantly decreased ulnolunate interval and occasionally foci of sclerosis or cystic changes in the lunate (Fig. 7.26). MRI is the most effective technique for the diagnosis of this syndrome and demonstration of pathologic changes in the affected bones and surrounding soft tissues. MRI reveals bone marrow edema of the distal ulna and lunate, subchondral sclerosis and cyst formation, and destruction of the cartilage. Associated abnormalities, such as tears of the triangular fibrocartilage and lunotriquetral ligament, are also well imaged (Figs. 7.27 and 7.28). Treatment of this condition includes TFCC debridement and ulnar shortening.
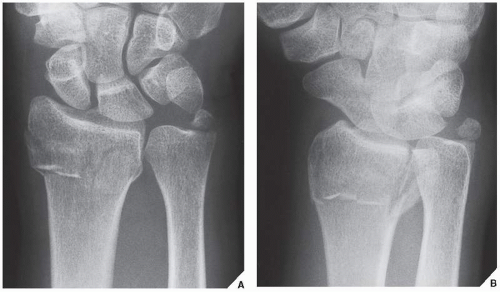
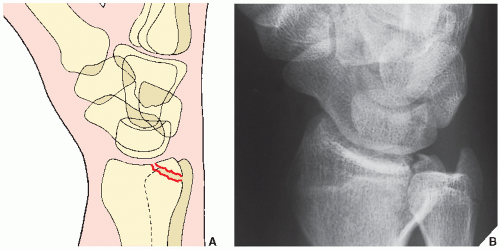
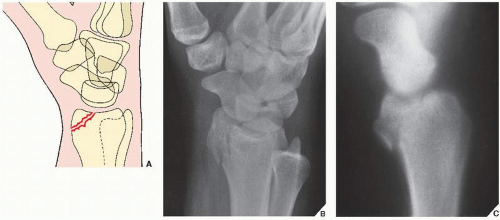
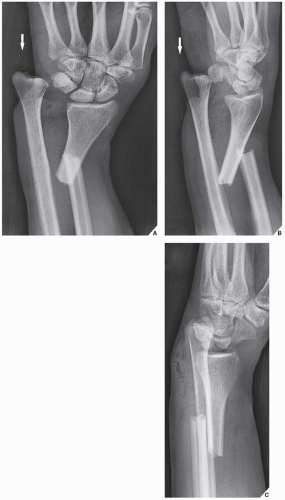
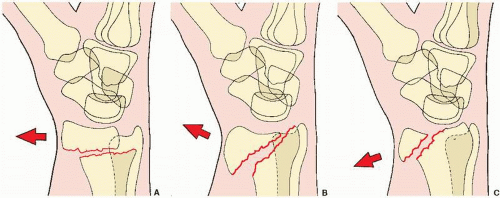 FIGURE 7.20 Smith fracture. The three types of Smith fracture are distinguished by the obliquity of the fracture line. Volar displacement of the distal fragment is characteristic of all three types. (A) In Smith type I, the fracture line is transverse, extending from the dorsal to the volar cortices of the radius. (B) The oblique fracture line in type II extends from the dorsal lip of the distal radius to the volar cortex. (C) Type III, which is almost identical to the reverse Barton fracture (see Fig. 7.17), is an intraarticular fracture with an extension to the volar cortex of the distal radius. |
 FIGURE 7.25 Ulnar impingement syndrome. Posteroanterior radiograph of the wrist shows a negative ulnar variance. The distal ulna impinges on the medial cortex of distal radius. |
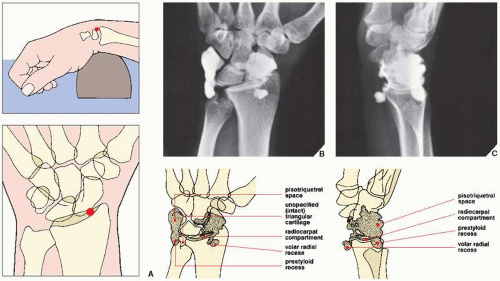
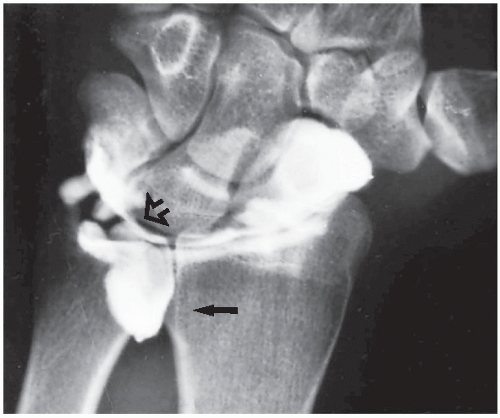 FIGURE 7.29 Arthrography of a TFCC tear. A single-contrast arthrogram of the wrist shows a leak of contrast into the space occupied by the triangular cartilage (open arrow), with characteristic filling of the distal radioulnar compartment (arrow), confirming a tear of the TFCC (compare with Fig. 7.7B). |
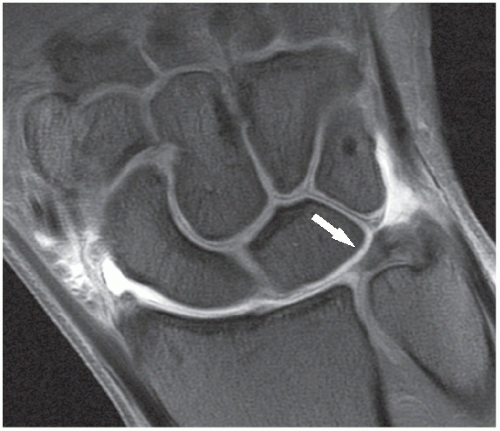 FIGURE 7.30 MRI of the wrist. Coronal T1-weighted fat-suppressed MR arthrographic image of the wrist shows a normal appearance of the TFCC (arrow). |
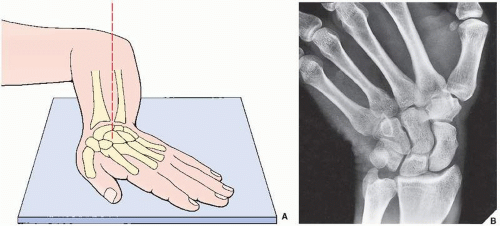
Dorsovolar obtained in ulnar deviation of the wrist for the evaluation of the scaphoid bone, which appears foreshortened on the standard dorsovolar projection as a result of its normal volar tilt (Fig. 7.32)
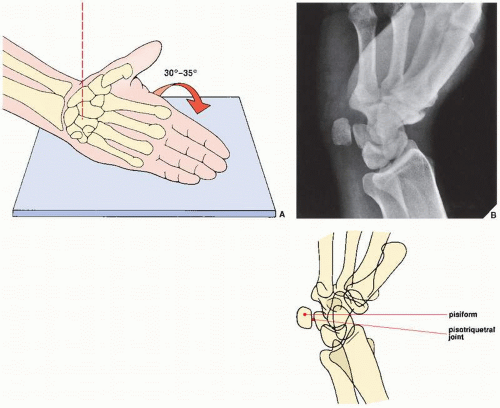
Supinated oblique for visualizing the pisiform bone and the pisotriquetral joint (Fig. 7.33)
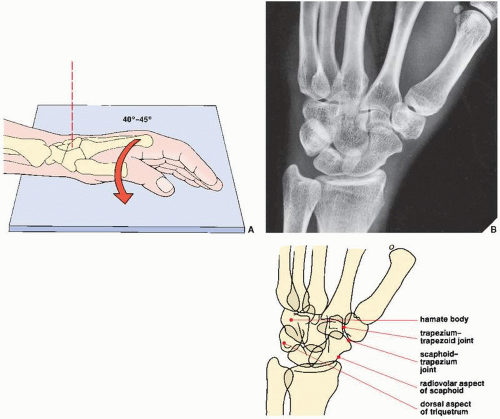
Pronated oblique for imaging the triquetral bone, the radiovolar aspect of the scaphoid, and the radial styloid process (Fig. 7.34)
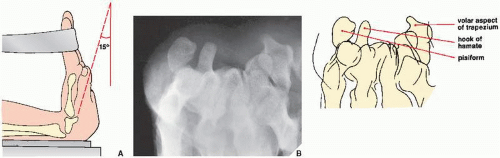
Carpal tunnel for demonstrating the hook of the hamate, the pisiform, and the volar aspect of the trapezium (Fig. 7.35)
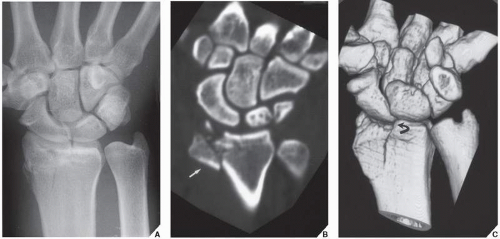
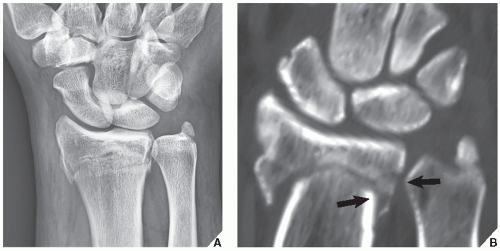
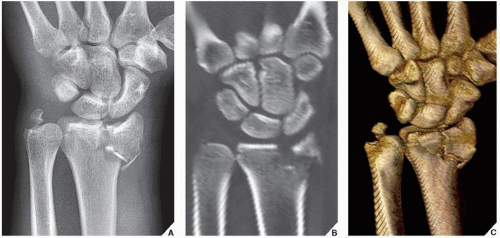
detecting subtle fractures and early complications of fracture healing. CT has evolved as a versatile tool and adjunctive procedure for imaging various traumatic abnormalities of the wrist. In many institutions, this technique virtually replaced conventional tomography, because it is easier to perform, is faster, and has a lower radiation dose. After standard axial sections are obtained, reformation images in additional imaging planes can be acquired and 3D reconstruction can be performed (see Fig. 2.8A,B). CT can be combined with arthrography (see Fig. 2.18) or can be enhanced by an intravenous contrast material. It is effective in demonstrating subluxation in the distal radioulnar joint and in evaluating the so-called humpback deformity of the scaphoid, osteonecrosis of the lunate (Kienböck disease), and fractures of the hook of the hamate, among other abnormalities. Axial sections are obtained after positioning the patient prone with the arm extended above the head. Contiguous sections of 1 or 2 mm are acquired, preferably using a spiral (helical) technique. Direct coronal sections can also be obtained with the wrist in maximal volar flexion or dorsal extension.
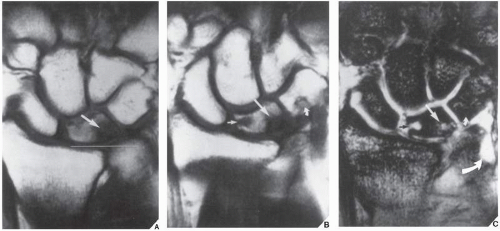
the carpal tunnel (Fig. 7.38) and detecting the subtle abnormalities of carpal tunnel syndrome (Fig. 7.39). Commonly, MRI is performed after an intraarticular injection of a contrast agent (diluted gadolinium) into the radiocarpal compartment (see Fig. 7.30).
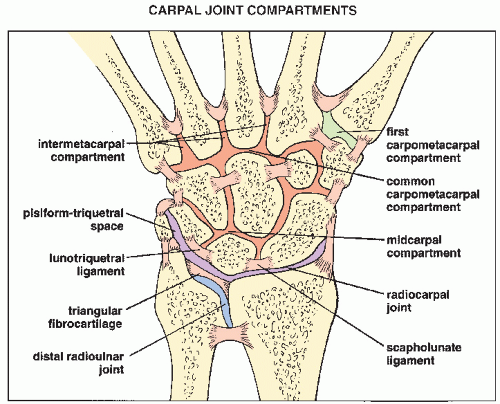 FIGURE 7.36 Compartments of the carpus. Carpal joint compartments are separated from one another by various interosseous ligaments. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree