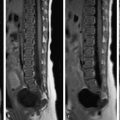
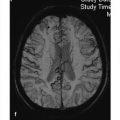
Thus, imaging results can be accurately interpreted only within the context of a detailed history and clinical examination. Of course, this principle applies to all radiologic findings. Degenerative changes in the spinal column should never be interpreted without clinical correlation. If patients with little or no back pain are informed that they have “severe degenerative spinal changes,” it is likely that their pain will take on a radically different quality. Back pain is among the most widespread health problems in our society. Approximately 80% of all people have experienced some degree of back pain in their lifetime. The point prevalence of back pain today is approximately 35%. Only about 14% of survey participants claim to have experienced back pain for more than 2 weeks. Only 4% of patients require inpatient treatment, and only 1% of all back-pain sufferers require surgery. The great majority of patients suffer “nonspecific” back pain, meaning that an underlying morphologic abnormality cannot be identified as the source of their pain. Approximately 90% of patients recover within a few weeks. These data make it clear that low back pain is a highly prevalent but benign condition that is often self-limiting. Epidemiology The incidence of lumbar disk herniations is 5% in the male population and 3.7% in the female population. Due to the high pressure loads combined with high mobility in the lumbar spine, lumbar disk herniations are most common (90% of cases) in the lowest segments of the spinal column, occurring predominantly at the L4–L5 and L5–S1 levels. Only 5 to 7% of herniations occur at L3–L4. The peak incidence is between 30 and 50 years of age, although disk herniations may also occur in children and older people. Clinical manifestations Clinically relevant disk herniations usually protrude in a posterior or posterolateral direction. Compression of the spinal nerve or dural sac produces corresponding clinical manifestations ranging from radicular pain, segmental hypoesthesia, and weakness to cauda equina compression symptoms or even transverse cord syndrome. The low back pain, often lancinating and of sudden onset, leads to lumbar postural and movement disorders, which are detectable even on plain radiographs. Physiologic lumbar lordosis is usually decreased and is accompanied by antalgic scoliosis. Typical pain on bearing down, coughing, or sneezing is often present. Physical examination elicits a positive Lasegue test. The posterior longitudinal ligament, the outer portions of the annulus fibrosus, portions of the periosteum and vertebral body, and the meninges and blood vessels in the epidural space receive a direct somatosensory supply. Disk protrusions in those areas may lead to circumscribed discogenic pain (lumbago; ▶ Fig. 12.1). Fig. 12.1 Radicular symptoms associated with disk herniations. Different nerve roots may be compressed depending on the location and direction of the herniation. A typical mediolateral disk protrusion at L4–L5 compresses the L5 root. A lateral herniation may compress the L4 root, while a medial herniation can compress the S1 root. Pathology Disk herniations may have a traumatic or degenerative etiology. Degenerative disk herniations result from aging processes marked by increasing desiccation of the nucleus pulposus and a diminishing disk volume. The water loss leads to a decrease in internal pressure and loss of disk height. This in turn lowers the resting tension of the ligaments that attach to the vertebral bodies. The altered static stability of the spinal column leads to increasing unphysiologic loads. Degenerative disk changes may allow disk material to herniate through a tear in the annulus fibrosus. Definition of terms Disk protrusion: This refers to the displacement of disk material while the annulus fibrosus is still essentially intact. A special type of protrusion is the disk bulge, in which the annulus fibrosus is uniformly thinned about its circumference and there is associated posterior displacement of the nucleus pulposus. Disk herniation (herniated disk, prolapsed disk, ruptured disk): Nucleus pulposus is displaced through a tear in the annulus fibrosus. Subligamentous disk herniation: The herniated material is still contained by the posterior longitudinal ligament. Extraligamentous disk herniation: The herniated material penetrates the posterior longitudinal ligament but is still in continuity with the parent disk. Extraligamentous sequestrum: The herniated material has lost continuity with the parent disk. The “sequestered” fragment of nucleus pulposus is posterior to the posterior longitudinal ligament within the spinal canal or intervertebral foramen and is generally extradural. In very rare cases, the sequestrum may be intradural. Posterior disk herniations Posterior disk herniations are classified by their location as medial, mediolateral, intraforaminal, or lateral ( ▶ Fig. 12.2). The majority are mediolateral. Rare types are foraminal herniations (approximately 6%, see ▶ Fig. 12.2) and lateral (extraforaminal) herniations, which impinge only on the nerve root rather than the dural sac or root sleeve and therefore are not visualized, or are visualized only indirectly, on conventional myelograms. Unlike medial or mediolateral herniations, lateral herniations most commonly occur at the L3–L4 and L4–L5 levels. They may occupy an intraforaminal, intra- and extraforaminal, or purely extraforaminal position. The intradural herniation of disk tissue requires a perforation of the annulus fibrosus combined with coexisting tears of the posterior longitudinal ligament and dura mater. Adhesions between the annulus fibrosus, posterior longitudinal ligament, and dura mater are a predisposing anatomic factor. A congenitally small spinal canal with a very small epidural space also predisposes to the compression of intraspinal structures and perforation of the dura. Congenital or iatrogenic weakness of the dura also plays a role. The L4–L5 level is affected in more than one-half of cases, followed by L3–L4. In contrast to extradural lumbar disk herniations, the lumbosacral disk is rarely involved (10% of cases). Fig. 12.2 Lumbar disk herniations. Diagrammatic representation. (a) Medial herniation. (b) Mediolateral herniation. (c) Intraforaminal herniation. Anterior disk herniations Anterior disk herniations are almost always subligamentous because the anterior longitudinal ligament is very thick and is firmly attached to the bone and annulus fibrosus. Anterior herniations typically lead to lipping of the vertebral margins. These “spondylophytes” often form higher at the L3–L4 and L4–L5 levels because stresses in the spinal column are concentrated farther anteriorly at those levels. Anterior herniations are controversial in terms of their clinical relevance. Mostly they are not believed to cause clinical complaints. A rare special case is an anterior limbus vertebra in young patients, caused by the intraosseous herniation of disk material beneath the ring apophysis, separating it from the rest of the vertebral body. Indications for imaging of low back pain Back pain may have various causes, so a differential diagnosis is needed. History-taking and clinical examination are of primary importance. The standard international classification consists of three parts based on clinical presentation: Simple back pain (local lumbar syndrome). Radicular pain (lumbar root syndrome). Alarming spinal symptoms (“red flags”). Note The main diagnostic tasks are to differentiate simple, nonradicular pain from radicular pain due to root compression and to recognize the few alarming cases with a more serious cause such as infection, tumor, or severe nerve entrapment. Imaging studies have an important role in this process, as they can help verify and supplement physical findings or provide a comprehensive overview in cases where the course of a disease is inconsistent with clinical or laboratory data. Selecting the appropriate imaging modality is crucial from the standpoint of cost-effective medicine. In particular, it should be decided whether imaging will influence therapeutic decision-making. Simple back pain Simple, nonradicular back pain usually has a mechanical and degenerative cause and accounts for 98% of back complaints. Simple back pain generally has a sudden onset and is characterized by position-dependent and load-dependent pain at the lumbosacral junction. Most patients are less than 40 years of age and may report a prior history of stress to the back from prolonged sitting, lifting, carrying, cold exposure, etc. As a general rule, this kind of simple back pain is self-limiting. In approximately 90% of cases, simple back pain will resolve within a few days or weeks, regardless of the type of treatment given. Since most patients experience marked improvement within a matter of weeks, this uncomplicated back pain does not require radiologic investigation. Simple back pain does not even require lumbar spine radiographs. When the criteria for simple back pain are present, the negative predictive value of lumbar spine radiographs is 99%. This means that only 1% of plain radiographs in patients with simple low back pain will detect an underlying cause. Consequently, radiographs of the lumbar spine are not only resource-intensive (in the United States, radiographs are ordered in 87% of patients with back pain) but also cause unnecessary radiation exposure. Note Provided there are no signs of a serious spinal disorder, plain radiographs should not be recommended in patients with low back pain. Even in cases of simple vertebragenic leg pain, imaging can be withheld during the acute phase if the complaints resolve within 6 weeks. Based on the results of a meta-analysis of the data from more than 1800 patients with acute and subacute low back pain (Chou et al, 2009), routine imaging is not advised unless there is evidence of a serious underlying condition. When patients who received immediate lumbar imaging (radiographs, CT, MRI) were compared with patients who did not, no significant differences were found with regard to function, quality of life, or mental health. Imaging findings may even prompt surgical procedures that do not always benefit the patient, quite apart from the increased costs. Accordingly, the current guidelines of various professional societies on the management of back pain include a clear recommendation that clinicians refrain from immediate imaging in patients with uncomplicated back pain. Red flags The situation is different when alarming spinal symptoms, or “red flags,” are present. A cauda equina syndrome and sudden weakness of functionally important muscles require prompt action and should be referred for immediate imaging. Other red flags such as weight loss, fever and malaise, a spinal mass, trauma, or persistent position-dependent pain also require further investigation to rule out inflammation, tumors, and metastases. Every physician is obliged to detect serious conditions such as tumors and inflammations without delay. This can be done by careful history-taking, clinical examination, and a few laboratory markers following unsuccessful initial treatment. Standard management should include referral to a specialist and early directed imaging. Radicular pain Imaging should also be part of the preoperative workup in patients with radicular complaints unresponsive to 4 to 6 weeks of conservative therapy. Immediate imaging is advised in patients with severe clinical symptoms or neurologic deterioration. Imaging in these cases can verify the clinical diagnosis and help direct surgical treatment planning. Note The indication for surgical treatment in patients with radicular pain should always be based primarily on clinical signs and symptoms, not on imaging findings. Imaging studies As sectional imaging modalities, CT and MRI are of key importance in spinal imaging. CT can provide acceptable views of intervertebral disk morphology in the lumbar spine. CT is generally accessible, cost-effective, and superior to MRI in the investigation of osseous pathology. On the other hand, radiation exposure from CT may be a concern, especially in younger patients. MRI is a more rewarding study in the primary imaging investigation of back pain due mainly to its multiplanar capabilities. It also provides much higher contrast resolution than CT. Changes in soft tissues such as nerves, the spinal cord, and intervertebral disks are detectable with high sensitivity. Also, the severity of degenerative disk changes can be evaluated on the basis of decreased T2w signal intensity, which is not possible with any other noninvasive procedure. MRI is equivalent to CT in the evaluation of facet joint osteoarthritis. Although MRI costs considerably more than CT, it has almost completely replaced CT as an initial imaging study. MRI also has considerably higher sensitivity and specificity in patients with suspected inflammatory or neoplastic disease and should therefore be the primary recommended imaging modality whenever it is available. Note Although it was formerly recommended that back pain be investigated by a staged approach (from conventional radiographs to MRI), MRI should now almost always be the initial modality in cases where imaging is clinically indicated. The following MRI techniques are useful for the investigation of back pain: Imaging planes: The sagittal plane is usually the most rewarding for spinal MRI. The basic sequences generally consist of sagittal T1w and T2w spin echo (SE) sequences ( ▶ Fig. 12.3). TSE sequences have the advantage of shorter acquisition times with less motion artifact. As the turbo factor increases, however, so does the signal-to-noise ratio. Cerebrospinal fluid (CSF) pulsation artifacts and transmitted pulsation artifacts from large vessels can be reduced by electroencephalographic (ECG) gating. The advantage of gradient echo (GRE) sequences over SE sequences is their shorter acquisition time. GRE sequences are particularly helpful in the cervical spine, where CSF pulsation artifacts are more pronounced than in the lumbar and thoracic regions. One disadvantage is that they are more sensitive to susceptibility artifacts. Consequently, GRE sequences should not be used if there are metallic foreign bodies (e.g., internal fixators) in the field of view. Sagittal coverage should extend far enough laterally that the intervertebral foramina are imaged and lateral disk herniations can be detected. It should be noted that sagittal images permit the level of the imaging volume to be determined with high precision. Coverage should therefore include the craniocervical junction or lumbosacral junction for localization purposes. Possible sources of error in identifying a specific level include supernumerary vertebrae and lumbosacral or thoracolumbar transitional vertebrae. Axial images (preferably in the plane of the disk space) are generally added at levels that appear suspicious based on clinical or sagittal imaging findings. Axial images are excellent for displaying the contents and borders of the spinal canal. Coronal images can supply useful additional information in certain types of investigation. Sequences: T2w inversion–recovery sequences with fat suppression (e.g., STIR sequences) are very sensitive for detecting edematous changes in the bony spinal column. This is particularly important in the investigation of skeletal metastases. CISS and MEDIC (multi-echo data image combination) sequences are other GRE sequences that can be used in spinal examinations. MEDIC is a heavily T2-weighted GRE sequence that is insensitive to flow artifacts and chemical shift artifacts. This makes MEDIC sequences particularly useful for axial examinations of the cervical spine. CISS sequences are three-dimensional GRE sequences with very high T2 contrast and a high signal-to-noise ratio that can provide resolution in the submillimeter range. MR myelography: Various techniques such as CISS, HASTE (half Fourier-acquired single-shot TSE), RARE (rapid acquisition with relaxation enhancement), or FISP, are available for obtaining myelogram-like views of the CSF spaces using two- or three-dimensional technique. They provide heavily T2-weighted images with a small slice thickness. Newer single-shot sequences can acquire MR myelographic images in seconds. Image quality can be improved by repetition of the sequences. Selected slices can then be reconstructed from the raw data matrix in various projections using the maximum-intensity projection (MIP) technique. Thus, MR myelography can provide a comprehensive survey of the dural sac and nerve roots at little additional cost ( ▶ Fig. 12.4), providing rapid orientation on possible pathologic changes (see ▶ Fig. 12.31c and ▶ Fig. 12.32d,e). Contrast medium: While the use of intravenous contrast medium is well established for inflammatory and neoplastic spinal diseases, its use in degenerative disorders depends on the purpose of the study. The most common applications are in the differentiation of recurrent disk herniation from postoperative scarring and the differential diagnosis of other lesions. Fig. 12.3 Spinal MRI, standard protocol for the cervical spine. (a) Sagittal T2w image. (b) Sagittal T1w image. (c) Sagittal T2w STIR image (with fat suppression). (d) Axial T2w image. Fig. 12.4 Cervical MR myelography at 3 T. (a) Sagittal T2w image. (b) MR myelography; T2w SPACE sequence (sampling perfection with application optimized contrasts using different flip angle evolutions), sagittal image. (c) MR myelography, coronal image. MRI findings Disk degeneration with associated changes in adjacent vertebral bodies Degenerative changes in the annulus fibrosus of the intervertebral disk cause structural changes involving the adjacent subchondral portions of the vertebral bodies. MRI can show characteristic signal intensity changes in the portions of the vertebral bodies adjacent to the endplates, which Modic classified into three types: Type 1 (edematous phase): This type involves an edematous inflammatory reaction, presumably based on the formation of vascular granulation tissue. MRI shows decreased signal intensity on T1w images and increased signal intensity on T2w images. Type 2 (fatty replacement): This type denotes the early chronic stage of vertebral body inflammation adjacent to the endplate. Type 2 develops from type 1 and is characterized by a streaky subcortical conversion of red marrow to yellow fatty marrow, which is hyperintense on T1w images and isointense or slightly hyperintense in T2w SE and GRE sequences ( ▶ Fig. 12.5). Type 3 (sclerosis): This type represents the late form of osteochondrosis and is characterized by vertebral body sclerosis adjacent to the endplate. The increased sclerosis is visible on plain radiographs and is hypointense in both T1w and T2w sequences. Fig. 12.5 Subligamentous disk herniation at L4–L5 with cranial migration. The sagittal T2w and T1w images show a subligamentous herniation of the L4–L5 disk with cranial migration. The continuity of the posterior longitudinal ligament is intact, and the sagittal T2w image defines the ligament particularly well as a hypointense band. Fatty degenerative changes are noted in the posterior upper and lower end plates of L4 and the lower end plate of L5 (Modic type 2). The axial T2w image shows the mass effect from the left mediolateral disk herniation with severe impingement on the dural sac. (a) Sagittal T2w image. (b) Sagittal T1w image. (c) Axial T2w image. MRI can demonstrate various affected structures: Disk protrusion or sequestrum: A protruding or sequestered disk normally has the same signal intensity as the affected disk on MRI. T2w images are particularly useful owing to the sharp contrast between degenerative disk material and CSF. Anterior and posterior longitudinal ligaments: The anterior and posterior longitudinal ligaments appear on MRI as black bandlike structures in contact with the bone and annulus. They are most clearly depicted on PDw and T2w images. With a subligamentous disk herniation, the posterior longitudinal ligament may appear elevated from the bone and disk tissue but its margins are intact with no discontinuities (see ▶ Fig. 12.5). With an extraligamentous herniation, the posterior longitudinal ligament is disrupted and there is disk material between the dura and ligament. Extraligamentous herniations are usually of considerable size and may be sequestered above or below the level of the parent disk ( ▶ Fig. 12.6, ▶ Fig. 12.7, and ▶ Fig. 12.8). Nerve root: MRI has proven highly effective in the detection of lateral disk herniation ( ▶ Fig. 12.9). Axial as well as sagittal images of the foramina or extraforaminal structures can demonstrate the herniation. In evaluating the intraforaminal segment of the nerve root, it should be noted whether the root is surrounded normally by periradicular epidural fat. An intraforaminal signal void from fat can be seen in sagittal T1w sequences. Disk herniations at a far lateral site may also affect the extraforaminal segment of the nerve root. This segment is well demonstrated in both T1w and T2w images. In the acute stage, it is not uncommon for nerve root compression to be associated with significant nerve root swelling, which mainly develops distal to the compression site. T2w images may show edema causing impingement on the nerve root sleeve. Contrast enhancement of the nerve root may signify compression. Intervertebral space: A gaseous collection in the intervertebral space (vacuum phenomenon) normally appears as a signal void in T1w and T2w images. Annulus fibrosus: Disk degeneration begins with a tear in the outer annular fibers. Some of these tears appear as a “high-intensity zone” on T2w images ( ▶ Fig. 12.10). Over time, these tears may enhance due to connective tissue ingrowth. Enhancement may also be detectable peridiscally and in the affected nerve root. T1w sequences before and after intravenous contrast administration are also helpful in the differential diagnosis of sequestered disk herniations. Even older disk herniations may show peripheral enhancement depending on the degree of scarring and vascularization. Dural sac and root sleeves: MR myelography can provide a rapid survey view of focal indentations in the dural sac or shortened root sleeves but is less sensitive in detecting nerve root compression or stenosis of the lateral recess. MR myelography does not detect lateral disk herniations, but the same problem exists in conventional myelography. Oblique views in the coronal plane are better for detecting sites of nerve root compression. Fig. 12.6 Lumbar disk herniation at the lumbosacral junction. Sagittal T2w and T1w images show a disk herniation at L5–S1 and small disk protrusions at L3–L4 and L4–L5. Axial T2w image shows a left mediolateral disk herniation with compression of the left S1 root (arrow). (a) Sagittal T2w image. (b) Sagittal T1w image. (c) Axial T2w image at the L5–S1 level. Fig. 12.7 Lumbar disk herniation at L3–L4. Axial CT shows a large midline disk protrusion at L3–L4. Sagittal T2w and T1w images confirm the L3–L4 herniated disk encroaching on the spinal canal. (a) Axial CT. (b) Sagittal T2w image. (c) Sagittal T1w image. Fig. 12.8 Disk herniation at L5–S1. Sagittal T2w and T1w images show a herniated disk at the lumbosacral junction. The disk space shows loss of height and decreased signal intensity. The other disk spaces appear normal. The axial T2w images show the left mediolateral disk herniation with caudal migration. The anterior indentation of the dural sac and posterior displacement of the S1 nerve root (Pfirrmann grade 2) are clearly visualized. Slight atrophy of the left paraspinal back muscles is also apparent. (a) Sagittal T2w image. (b) Sagittal T1w image. (c) Axial T2w image. (d) Axial T2w image in a different plane. Fig. 12.9 Lateral disk herniation at L3–L4. Axial T2w image shows a left lateral disk herniation at L3–L4 impinging on the L3 nerve root (arrows). There is slight narrowing of the neural foramen on the left side. Fig. 12.10 High-intensity zone at L4–L5 in a 35-year-old man with persistent low back pain after vertebral trauma. The MR images show a high-intensity zone in the midline at L4–L5, most likely representing a fresh tear of the annulus fibrosus. (a) Sagittal T2w image. (b) Axial T2w image. MRI classification of disk herniations The classification described by Pfirrmann is clinically useful in the radiologic description of disk protrusions. The spatial relationship of the disk to neural structures has particular clinical relevance. The degree of intraspinal extradural nerve root compression is classified into four grades: Grade 0 (normal): No contact between the intervertebral disk and nerve root; presence of normal epidural fat between the disk and nerve root. Grade 1 (contact): Visible contact between the disk and nerve root; normal epidural fat is not visualized. The nerve root occupies a normal position with no posterior displacement. Grade 2 (displacement): Posterior displacement of the nerve root by disk tissue (see ▶ Fig. 12.8). Grade 3 (compression): The nerve root is compressed between disk tissue and the wall of the spinal canal and is poorly delineated from disk tissue (see ▶ Fig. 12.6). Tips and Tricks Using a standard nomenclature for describing and evaluating lumbar disk problems will aid communication between the referring physician and radiologist. We emphasize that it is not uncommon to find extensive degenerative changes with disk protrusions and, in rare cases, even disk herniations in patients who are clinically asymptomatic. MRI studies in asymptomatic subjects have revealed disk protrusions in more than one-half of the participants and actual herniations in almost 30%. Only one-third of the participants had normal-appearing disks at all levels. Thus, even impressive radiologic findings may occur with no clinical correlation. The presence of absence of clinical symptoms depends on the involvement of neural structures. Nerve root compression was found to be significantly more common in symptomatic patients (83%) than in asymptomatic patients (22%). Treatment The conservative treatment of acute low back pain in the acute phase is limited to bed rest in a flat supine position or with the lower legs elevated on a cushion. Treatment is supported with analgesics and muscle relaxants. This therapy is less for immediate pain relief than to interrupt the reflex locking of affected motion segments in response to pain. When acute pain symptoms have subsided, careful remobilization can begin in the form of therapeutic exercises. Surgical treatment is indicated if conservative therapy is unsuccessful and depends on the severity of radicular dysfunction, pain, and clinical course. The development of a cauda equina syndrome or an acute loss of critical muscle functions are absolute indications for surgical intervention. Note It is important to distinguish between disk protrusions and herniations because they have different therapeutic implications. Today, open disk operations are generally performed using a microsurgical technique. The advantages of this technique are minimal tissue trauma and the precise removal of disk material encroaching on the spinal canal. Differential diagnosis Spondylolisthesis Spondylolisthesis, with an incidence of 5 to 7%, is a very rare cause of neurologic symptoms. More than one-half of patients with radiologically confirmed spondylolisthesis remain asymptomatic. Also, there is no correlation between the severity of complaints and the degree of vertebral slip. The most common form, which involves a pars defect and occurs at L5 in over 90% of cases, does not become symptomatic until early adulthood. A typical symptom is low back pain radiating to the buttock and thigh in a pseudoradicular pattern. Not infrequently, an edematous inflammatory reaction comparable to Modic 1 changes (edematous phase, ▶ Fig. 12.11) can be detected with MRI, especially in sensitive STIR sequences. Degenerative spondylolisthesis is a disease of adults and is rarely seen before age 50. Females are more commonly affected than males. The great majority of cases involve slippage of the L4 vertebra over L5 (see ▶ Fig. 12.33). This subluxation is usually mild and rarely exceeds 30%. Neurologic impairment is secondary to reactive hypertrophic changes occurring in response to the segmental instability, with thickening of the facet joints and hypertrophy of the ligamenta flava. The manifestations of an isolated lateral recess stenosis are clinically indistinguishable from those of a herniated disk. Fig. 12.11 Bilateral spondylolysis of the L3 pars interarticularis in a 14-year-old competitive gymnast with back pain. Sagittal T2w image shows increased signal intensity in the pars at L3. The sagittal and axial STIR images demonstrate bilateral edema in the L3 pars, comparable to erosive osteochondrosis or Modic 1 change. Faint enhancement is noted in the fat-suppressed axial T1w image. (a) Sagittal T2w image. (b) Sagittal STIR image. (c) Axial STIR image. (d) Axial T1w image with fat suppression. Ankylosing spondylitis Due to its frequency, its predilection for males in the third decade, and typical involvement of the sacroiliac joints, ankylosing spondylitis should sometimes be considered in the differential diagnosis of low back pain. The inflammatory joint changes lead to a diffuse, pseudoradicular pattern of pain radiating to both thighs; this is much more common than actual root compression. The correct diagnosis is suggested by the history of gradual onset, typical rest pain, morning stiffness, and frequent stiffness at night. Arachnoiditis Spinal arachnoiditis is a rare condition that may occur spontaneously but more often follows intrathecal drug administration or myelography, surgery, or spinal meningitis. The clinical presentation is highly variable and nonspecific. Relatively common symptoms are exacerbating low back pain in response to mild exertion and bilateral sciatica with a burning pain. The clinical diagnosis is confirmed by typical myelographic findings of contour irregularities, narrowing and shortening of the lumbar dural sac, nonvisualization of root sleeves, and thickened nerve roots with adhesions. Tumors Tumors are a very rare cause of lumbar radicular syndrome (1–2%) compared with disk herniations. Early detection is important, however, because the prognosis can be significantly improved by early initiation of treatment, regardless of whether the tumor is malignant or benign. The cardinal symptom is pain, an early symptom that may precede radiating radicular pain by weeks or months. Unlike the pain of a herniated disk, which usually has an acute onset, is often intermittent, and is aggravated by exercise, “tumor pain” starts insidiously and increases over time to an unremitting pain that is not relieved by rest. Primary tumors of the spinal column are rare. One tumor with a predilection for the lumbosacral region is chordoma, which usually produces neurologic symptoms due to its locally invasive growth. More common lesions are spinal metastases, which in up to 50% of cases are the initial manifestation of an underlying primary malignancy. Diffuse meningeal infiltration by a tumor can also lead to radicular complaints. Again, sensitive MRI is the imaging modality of choice. The most common intraspinal extradural masses in the lumbar spine are sequestered disk herniations or bony processes that narrow the spinal canal. The most common intradural, extramedullary tumors are neurofibromas (neurinomas) in the lumbosacral region of younger patients. Meningiomas occur predominantly in the thoracic region and predominantly affect older women. While neurinomas and meningiomas generally show homogeneous enhancement and are easily distinguished from the peripheral enhancement of intradural disk material, ependymomas may prove more difficult. These tumors also show intense enhancement but, unlike disk material, are hyperintense in T2w sequences. Epidermoids and dermoids ordinarily do not enhance.
12.2 Disk Herniations
12.2.1 Lumbar Disk Herniations











Radiology Key
Fastest Radiology Insight Engine