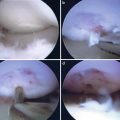
Fig. 20.1
Clinical photo of supine positioning of the arm in suspension for elbow arthroscopy
Prone
The prone position is an additional method of positioning. The greatest benefit of the prone positioning is the excellent access to the posterior compartment of the elbow. Direct visualization of the ulnohumeral joint from posterior is helpful for debridement of excess bone in cases of posterior impingement. The face and chest are padded and supported by a foam airway/head positioner and padded chest rolls. The nonoperative extremity is positioned in 90° of shoulder abduction and external rotation with the elbow in 90° of flexion. Often a special arm holder is used to optimize positioning of the operative arm. A non-sterile arm tourniquet is applied, and the arm is place in 90° of shoulder abduction and neutral rotation. The arm is supported at the mid-humeral level by a padded arm holder attached to the operating table allowing for flexion and extension of the arm during arthroscopy (Fig. 20.2a, b).


Fig. 20.2
(a, b) Author’s preferred setup for elbow arthroscopy in prone position with arm holder under mid-humerus giving plenty of room for range of motion during procedure
In the prone position, several advantages are realized. The elbow is easily manipulated from flexion to full extension. The posterior compartment of the elbow is easily accessible for numerous procedures directed by posterior pathology. Open procedures are easily performed if necessary. If the surgeon chooses to perform an open procedure, no change in positioning is needed for posterior procedures. Medial or lateral procedures can be carried out in the prone position by internally or externally rotating the shoulder and supporting the arm on a padded arm board (Figs. 20.3 and 20.4). Drawbacks of the prone position primarily relate to patient positioning, ventilation, and anesthetic options. It is imperative to support the head and face with foam padding to secure the airway, and chest rolls are needed to facilitate ventilation. Regional anesthesia is poorly tolerated and may not provide adequate anesthesia thus necessitating conversion to general anesthesia. In such cases, repositioning is necessary to establish an airway.
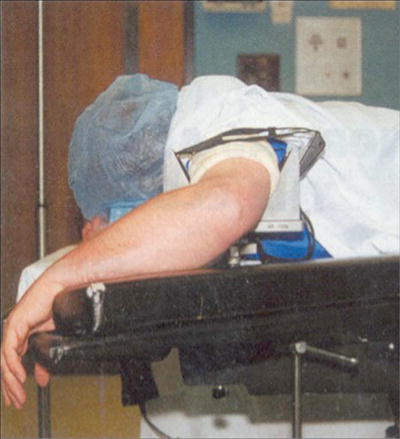

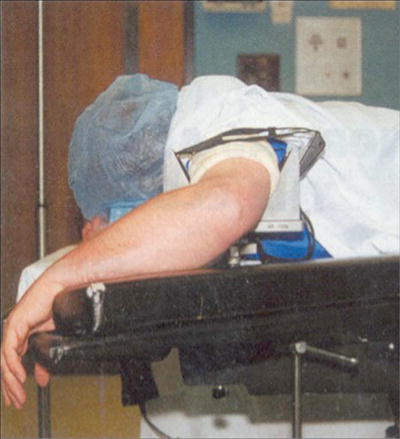
Fig. 20.3
Clinical photo shown demonstrating the ability to externally rotate the shoulder and support the forearm on the arm board in prone position for an open lateral approach to the elbow

Fig. 20.4
Clinical photo demonstrating the ability to internally rotate the shoulder and rest the forearm on an arm board to gain access to the medial elbow for an open procedure
Lateral Decubitus
The aim of this position is to take advantage of the benefits of both the supine and prone position while avoiding the major pitfalls inherent to each setup. A beanbag is used to place the patient in the lateral decubitus position. An axillary roll is appropriately placed. The operative extremity is positioned over an arm holder or over a padded bolster with the shoulder internally rotated and flexed to 90°. The elbow is maintained in 90° of flexion (Fig. 20.5).


Fig. 20.5
Lateral positioning of the arm in elbow arthroscopy (used with permission from Baker CL, Grant LJ. Arthroscopy of the elbow. Am J Sports Med. 1999;27:251–64)
The elbow is maintained in the prone position thus affording the advantages of the prone position. Patient positioning is simplified with respect to prone positioning, and airway maintenance is easily monitored with adequate exposure for the anesthesiologist. Disadvantages include the need for a padded bolster and the potential inconvenience of repositioning should a need for an open procedure arise.
Portal Placement
A thorough understanding of the bony and neurovascular anatomy around the elbow is necessary prior to proceeding with elbow arthroscopy. After adequate positioning, prepping, and draping, the landmarks about the elbow should be palpated and marked with a sterile marker. The medial and lateral epicondyles, the olecranon, and radial head should be marked. Care should also be taken to palpate the ulnar nerve in its groove. It should be noted if the nerve is subluxed or subluxable prior to portal placement as this could lead to injury of the nerve. Its course should be marked with the sterile marker as well. It should also be noted that all positions for elbow arthroscopy allow for flexion of the elbow at 90°. This is vital because flexion moves the neurovascular structures anteriorly further from the joint and provides more space for portal placement [26].
Proximal Anteromedial Portal (Figs. 20.6 and 20.7)
Fig. 20.6
The medial elbow with anteromedial and proximal anteromedial portals shown. The ulnar, median, and medial antebrachial nerves are all in close proximity to these portals as described above. Note that the proximal anteromedial portal is at increased distance from the median nerve as compared to the anteromedial portal (used with permission from Cole BJ, Sekiya JK. Surgical techniques of the shoulder, elbow, and knee in sports medicine. Philadelphia: Elsevier Saunders; 2008)

Fig. 20.7
Operative view of the medial elbow. P posterior portal, PAM proximal anteromedial portal, UN ulnar nerve, ME medial epicondyle (used with permission from Baker CL, Grant LJ. Arthroscopy of the elbow. Am J Sports Med. 1999;27:251–64)
The proximal anteromedial portal is made 2 cm proximal to the medial epicondyle and 1–2 cm anterior to the intermuscular septum. A nick in the skin is made, and the blunt tip trocar is advanced to the anterior surface of the humerus. The trocar is kept in contact with the anterior cortex and then slid distally to the elbow joint. This technique keeps the trocar posterior to the brachialis muscle therefore protecting the median nerve and brachial artery. Blunt dissection stays anterior to the medial intermuscular septum and thus anterior to the ulnar nerve. Structures at risk during creation of this portal are the medial antebrachial cutaneous, median, and ulnar nerves. The medial antebrachial cutaneous nerve is at risk as it courses approximately 2.3 mm from the portal site. The median nerve is at risk as the trocar is advanced distally between the humerus and brachialis muscle. The average distance from the median nerve to the trocar tip is 12.4–22 mm [22, 27].
Relative contraindications to the creation of this portal include ulnar nerve subluxation or previous ulnar nerve transposition [22, 27, 28]. In the case of prior ulnar nerve transposition, this portal can be utilized if care is taken to identify the course of the nerve with dissection prior to trocar placement. In the absence of ulnar nerve subluxation or history of transposition, the ulnar nerve is located between 12 and 23.7 mm from the portal site and is hence not at risk so long as the trocar entry site is placed anterior to the intermuscular septum [22, 27].
This portal is easily reproducible and provides visualization of the entire anterior compartment from the medial to the lateral gutter. As such, it serves well as the initial portal in elbow arthroscopy.
Anteromedial Portal (Figs. 20.6 and 20.7)
This portal is placed 1–2 cm anterior and 2 cm distal to the medial epicondyle [29]. A nick in the skin is made, and the blunt tip trocar is advanced through the flexor mass aiming for the radial head taking care to stay between the humerus and the brachialis. With the trocar anterior to the medial epicondyle and the ulnar nerve in its normal anatomic position, the ulnar nerve should not be at risk. The greatest risk is to the medial antebrachial cutaneous which passes 1–2 mm from the portal site [22]. Risk of injury can be minimized by incising skin only and using the blunt trocar for the subcutaneous dissection [25, 27]. The median nerve travels approximately 7–14 mm away from the portal site and is at less risk of injury if the surgeon maintains dissection posterior to brachialis [22, 30]. The standard anteromedial portal is therefore almost twice as close to the median nerve as the proximal anteromedial portal determined by the difference between the anatomical measurements mentioned above, 7–14 mm away from the portal in standard anteromedial portal versus 12–23.7 mm away from the portal in the proximal anteromedial portal. The proximal anteromedial portal presents a safer alternative to standard anteromedial portal therefore minimizing the risk of a devastating median nerve injury.
Proximal Anterolateral Portal (Fig. 20.8)
Fig. 20.8
Lateral view of the elbow with anterolateral and proximal anterolateral portals shown. Note that the proximal anterolateral portal is at increased distance from the radial nerve as compared to the anterolateral portal (used with permission from Cole BJ, Sekiya JK. Surgical techniques of the shoulder, elbow, and knee in sports medicine. Philadelphia: Elsevier Saunders; 2008)
The proximal anterolateral portal in addition to the proximal anteromedial portal can also be used as a starting portal [9, 31, 32]. It is established 2 cm proximal and 2 cm anterior to the lateral epicondyle. This portal was developed as an alternative to the standard anterolateral portal, due to the portal providing greater safe distance from the radial nerve [22, 31]. Anatomic studies with the elbow in 90° of flexion and distended with fluid at the time of proximal anterolateral portal creation reveal a safe distance between 9.9 and 14.2 mm between the trocar and radial nerve [22, 31]. This distance is markedly decreased to 4.9–9.1 mm when the standard anterolateral portal is created [22, 31]. The lateral antebrachial cutaneous nerve passes 6 mm from this portal site [22].
As the trocar is advanced distally, toward the elbow joint, the brachioradialis and brachialis muscle are pierced prior to entering the lateral joint capsule. With the arthroscope placed into the cannula, the anterior capsule, lateral gutter, radial head, capitellum, coronoid, and anterolateral aspect of the ulnohumeral articulation can be visualized. It is believed by some authors that the proximal anterolateral portal provides improved visualization of the lateral aspect of the joint [31].
Anterolateral Portal (Fig. 20.8)
The anterolateral portal was originally described as being made 1 cm anterior and 3 cm distal to the lateral epicondyle [18]. As the blunt trocar is introduced, it passes through the extensor carpi radialis brevis muscle before traversing the lateral joint capsule. This portal position is limited in its capabilities with respect to the lateral joint. However, it permits visualization of the anteromedial aspect of the joint including the trochlea, coronoid fossa, coronoid process, and medial aspect of the radial head [31]. Care must be taken not to place the portal distal to the radial head, as the posterior interosseous nerve courses 1–1.5 cm from the radial head around the radial neck. Furthermore, care should be taken not to make the portal distal to the radial head as this can endanger the radial nerve. The radial nerve passes 5–9 mm from this portal site [22, 27, 28].
An inside-out technique allows the arthroscope in the anteromedial or proximal anteromedial portal to be advanced over the radial head and pressed firmly against the joint capsule lateral to the radial head. The camera is exchanged in the cannula for a switching stick which is advanced through the extensor carpi radialis brevis until it tents the skin. Incision is made over the switching stick, and cannula is inserted over the switching stick. This portal provides good access to the radial head and allows visualization of the annular ligament.
Direct Lateral Portal (Figs. 20.9, 20.10, and 20.11)
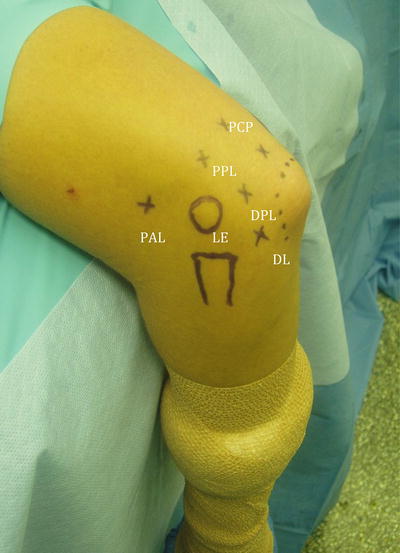
Fig. 20.9
Operative view of the lateral elbow. PCP proximal central posterior portal, PPL proximal posterolateral portal, DPL distal posterolateral portal, DL direct lateral portal, PAL proximal anterolateral portal, LE lateral epicondyle
Fig. 20.10
Schematic of lateral view of the elbow with the direct lateral portal shown which is located in the soft spot marked by the lateral epicondyle, radial head, and tip of the olecranon (used with permission from Cole BJ, Sekiya JK. Surgical techniques of the shoulder, elbow, and knee in sports medicine. Philadelphia: Elsevier Saunders; 2008)

Fig. 20.11
Operative view of the lateral elbow. Instrument pointing to the lateral soft spot and location of the direct lateral portal (used with permission from Baker CL, Grant LJ. Arthroscopy of the elbow. Am J Sports Med. 1999;27:251–64)
Also known as the soft spot portal, this portal is often used for the initial insufflation of the joint with an 18-gauge needle. It is found in the soft spot in the triangle marked by the lateral epicondyle, radial head, and tip of the olecranon. This portal is fairly safe with regard to neurologic structures with the sole risk being injury to the posterior antebrachial cutaneous nerve which courses approximately 7 mm away [33]. The biggest risks of this portal are the risk of fluid extravasation into the soft tissues and postoperative portal drainage [22, 23, 28].
When establishing this portal, the trocar is advanced through the anconeus muscle, and entry to the lateral elbow joint is attained through the posterior elbow capsule. Visualization of the radioulnar joint and inferior aspect of the radial head and capitellum can be achieved through this portal site. In addition, this portal provides a safe entry site for instrumentation of the radiocapitellar joint and lateral gutter. Due to the risk of soft tissue extravasation, it is advisable to delay making this portal until near the end of the operation.
Posterior Portals (Figs. 20.12 and 20.13)
Fig. 20.12
Schematic of the posterior elbow with the distal central posterior portal (named in this figure as straight posterior) and distal posterolateral portal shown (used with permission from Cole BJ, Sekiya JK. Surgical techniques of the shoulder, elbow, and knee in sports medicine. Philadelphia: Elsevier Saunders; 2008)

Fig. 20.13




Operative image of the posterior of the elbow showing portals including proximal and distal straight posterior portals and the proximal and distal posterolateral portals. PCP proximal central posterior portal, DCP distal central posterior portal, PPL proximal posterolateral portal, DPL distal posterolateral portal, DL direct lateral portal, PAL proximal anterolateral portal, LE lateral epicondyle, UN ulnar nerve
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree