Diagnostic Imaging of the Chest in Intensive Care Medicine
16.1 Indications for Chest Radiography in Intensive Care Medicine
The value of daily routine chest radiography for each patient in an intensive care unit has long been a contentious issue. A recent meta-analysis did not find any advantage for daily chest radiography compared with clinically indicated chest radiography.1 Therefore, the use of daily routine chest radiography in the intensive care unit has now been abandoned.1,2,3,4,5
In its appropriateness criteria, the American College of Radiology lists the relevant indications, as illustrated in ▶Table 16.1.
16.2 Detection and Malposition of Implanted Devices
16.2.1 Tracheal Tubes
The distal end of the endotracheal tube should be positioned 4 to 6 cm above the tracheal bifurcation (▶Fig. 16.1). Movement of the head leads to downward or upward positioning of the tube by approximately 2 cm.6 Malposition of the endotracheal tube is common, but with widespread variation in the incidence reported in the literature (2-46%). Only in a minority of cases is this clinically suspected.5 Therefore, radiography is warranted to confirm correct tube position after insertion. The distal end of the tube is usually placed too low in one of the two mainstem bronchi or too high. Less often, the endotracheal tube is positioned in the esophagus. If so, the tube does not follow the tracheal contour on chest radiography.
Table 16.1 Indications for chest radiography for intensive care unit patient5 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Certain clinical situations require separate lung ventilation. This is generally the case in lung surgery. The tip of the double lumen endotracheal tube is placed in one mainstem bronchus and the tube ventilates the other lung via a side hole. Such a finding should not be misinterpreted as tube malposition.
16.2.2 Central Venous Catheters
Ideally, the tip of a central venous catheter is located just above the opening of the superior vena cava into the right atrium (▶Fig. 16.2). On chest radiography, it corresponds to a position of approximately 4 cm below the tracheal bifurcation. Too low placement in the right atrium can cause cardiac dysrhythmia and mechanical irritation of the tricuspid valve.
 Fig. 16.3 Typical malpositions of central venous catheters. Schematic diagram. (a) For right-sided placement. (b) For left-sided placement. |
Malposition is seen in around 10% of central venous catheters (▶Fig. 16.3). Puncture-related pneumothoraces are less common at a rate of up to 6%, and occur most often with the subclavian approach.6 Hence, radiography is indicated immediately after insertion. If extravascular catheter position is suspected, instillation of a few milliliters of contrast media is recommended for verification of extra- or intravascular placement. New onset pleural effusion and rapidly progressive mediastinal widening are signs of extravascular line placement. If the catheter is not seen to be positioned exactly at the right mediastinal border but is observed instead to run in the direction of the aortic arch, intra-arterial position should be suspected. This can be confirmed or excluded through blood gas analysis of a sample taken from the catheter.
16.2.3 Pulmonary Artery Catheters (Swan-Ganz Catheter)
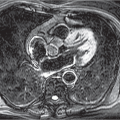
The tip of a pulmonary artery catheter is normally positioned in the right pulmonary artery (▶Fig. 16.4). Correct placement in the pulmonary artery is verified by registration of the pressure curve, thus largely precluding any relevant malpositioning. But malpositioning can be expected if a characteristic pulmonary artery pressure curve cannot be recorded during placement. Chest radiography is used for documentation of an often clinically suspected malposition and helps to correct this. Chest radiography is always indicated immediately after catheter insertion to confirm correct position and exclude pneumothorax.
Central placement of the catheter tip in the proximal pulmonary trunk can irritate the pulmonary valve because of catheter pulsation. A very peripheral catheter position, usually well into
the right lower lobe artery, corresponds to the measurement position for the pulmonary capillary wedge pressure, known as the wedge position. After measurement, the catheter is usually pulled back again into a central pulmonary artery.
the right lower lobe artery, corresponds to the measurement position for the pulmonary capillary wedge pressure, known as the wedge position. After measurement, the catheter is usually pulled back again into a central pulmonary artery.
16.2.4 Nasogastric Tubes
Nasogastric tubes usually have side holes which are several centimeters distant from the tip. Therefore, a nasogastric tube should be positioned at least 10 cm below the diaphragm to prevent reflux into the esophagus as well as aspiration (▶Fig. 16.5). Placement of the nasogastric tube tip in the esophagus is the most common malposition. There are many reasons for this:
The tube is not advanced far enough.
The tube was placed correctly initially but was then dislodged upward.
The tube is reverted in the esophagus.
The nasogastric tube may, on rare occasions, enter the tracheobronchial tree. Because of the potentially severe complications, the correct infradiaphragmatic tube position must be confirmed radiographically at least before infusing nutrient solutions.
Some nasogastric tubes are only faintly radiopaque and are difficult to detect on chest radiography, in particular in the upper abdomen. Changing the window settings or gray scale inversion may help locate the tube tip. In the worst case scenario, the nasogastric tube must be rendered visible through instillation of a few milliliters of contrast media.
16.2.5 Chest Tubes
Chest tubes are widely used in thoracic surgery and are placed under visual control; hence, malposition is not expected in this setting. Moreover, chest tube placement is a routine procedure in the intensive care unit and preclinical emergency medicine. In the latter setting, tube malposition occurs in approximately 10% of cases.7,8,9 Therefore, chest radiography is recommended for chest tubes inserted on the intensive care unit setting to exclude malposition and pneumothorax and to verify the effectiveness of the drainage function. Persistent air fistula through the chest tube suggests a tube malposition in the lung parenchyma; CT is superior to chest radiography at visualizing or excluding this condition.
16.2.6 Intra-Aortic Balloon Pump
An intra-aortic balloon pump (IABP) is implanted in patients with severe left ventricular failure to support cardiac pump function. A long balloon inserted via the femoral artery into the aorta always inflates in diastole, thus pumping blood from the aorta into the periphery. The balloon deflates again in systole. The IABP itself is usually not visualized on chest radiography; at most, only a small metallic marker is identified at the proximal tip of the balloon which should be positioned just distal
to the origin of the left subclavian artery from the aortic arch. Accordingly, the marker is projected between the middle and lower third of the aortic notch (▶Fig. 16.6). A too-high location of the balloon presents a risk of occlusion of the left subclavian artery, while in the worst case scenario too-low placement may cause intestinal ischemia due to occlusion of the origins of the large abdominal arteries.
to the origin of the left subclavian artery from the aortic arch. Accordingly, the marker is projected between the middle and lower third of the aortic notch (▶Fig. 16.6). A too-high location of the balloon presents a risk of occlusion of the left subclavian artery, while in the worst case scenario too-low placement may cause intestinal ischemia due to occlusion of the origins of the large abdominal arteries.
16.2.7 Other Implanted Devices
Artificial hearts are classified as follows in accordance with their support function:
Left ventricular assist devices (LVAD).
Right ventricular assist devices (RVAD).
Biventricular assist devices (BiVAD).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree