Imaging Presentation
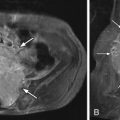
Midline sagittal T2-weighted magnetic resonance (MR) image reveals a low-lying spinal cord and decrease in height of the L4 vertebral body. The axial T2-weighted MR image obtained at the L4 level demonstrates that the low-lying spinal cord is split into two equal halves and separated by a cerebrospinal fluid (CSF) cleft. There is some anteroposterior-oriented low signal intensity in the L4 vertebral body. Coronal imaging (not pictured) revealed an L4 butterfly vertebra ( Fig. 19-1 ) .

Discussion
Diastematomyelia, also called split cord malformation , is a congenital malformation characterized by a division of the spinal cord and/or cauda equina in the sagittal plane, which is often associated with vertebral anomalies. The two hemicords are often separated by a bony fibrocartilaginous septum that is attached anteriorly to one or more vertebral bodies and posteriorly to the neural arches (posterior elements). The two hemicords usually (91%) rejoin into a single cord below the level of the division. The cleft typically occurs between T9 and S1 in 85% of cases. The cleft is exclusively in the thoracic spine in 20.6% of cases, the thoracolumbar region in 17.6%, and the lumbar in 61.8%. The conus medullaris is typically low in position. Diastematomyelia is the most frequent form of failed midline integration of the notochord and accounts for 3.8% of all closed spinal dysraphisms. Patients with diastematomyelia may be asymptomatic. When symptoms result, they can be indistinguishable from any etiology causing spinal cord tethering. Symptoms often result from tethering of the spinal cord and are secondary to associated vertebral anomalies. In children, symptoms may include foot and spinal deformities, weakness in the legs, low back pain, scoliosis, and incontinence. In adulthood, the signs and symptoms often include progressive sensory and motor problems and loss of bowel and bladder control.
The term diastematomyelia comes from the Greek diastema (cleft) and myelos (cord) and is irrespective of whether or not there is a bony or fibrous spur interposed between the two hemicords. Each hemicord gives rise to the ipsilateral dorsal and ventral nerve roots, although occasionally, one hemicord can give rise to three roots (ipsilateral ventral and dorsal roots and the contralateral ventral root), and the other hemicord gives rise to only the ipsilateral dorsal root. Either way, the four normal roots (two ventral, two dorsal) arise at each level. The anterior spinal artery forms from paired primordia at the same time that diastematomyelia occurs. If there is failure of fusion of the paired primordia into a single anterior spinal artery, there may be paired anterior spinal arteries, each supplying one of the hemichords. Diastematomyelia is different from diplomyelia, which is a true duplication of the spinal cord, producing two spinal cords, each of which contains one central canal, two dorsal horns, two ventral horns, and four segmental nerve roots at each level.
Embryologically, diastematomyelia is a failure of midline integration resulting in two paired notochords that are separated by primitive streak cells. Diastematomyelia is subcategorized into two subtypes depending on the fate of the primitive streak cells. If the streak cells develop into bone and cartilage, the two hemichords will be contained in their own dural sac separated by an osteocartilaginous spur. This type of abnormality is referred to as Pang type I. If the streak cells resorb or leave a thin fibrous band, the two hemichords will be contained in a single dural sac. This type of abnormality is referred to as Pang type II.
Diastematomyelia Type I
Type I diastematomyelia (diastematomyelia with osteocartilaginous septum) consists of two hemichords, each contained within its own dural sac and separated by a bony osteocartilaginous spur. The spur usually extends from the vertebral body to the neural arches along a midsagittal plane. Spurs can also course obliquely and may be complete or incomplete, arising from either the vertebral body or from the neural arch. The two hemichords are usually the same caliber; however, the spur can occasionally split the hemichords unequally. The spur is usually located in the thoracic and/or lumbar regions and lies at the caudal end of the cord splitting. The hemichords are in close proximity to the spur just cranial to the point where the hemichords will fuse into a single cord inferiorly. Vertebral anomalies are highly associated with type I and include bifid lamina, increased interpedicular distance, hemivertebrae, fused vertebrae, and disc space narrowing. Scoliosis is seen in 30% to 60% of patients and is usually due to the underlying bone abnormalities. Cutaneous hemangiomas, dyschromic patches, and hairy tufts often suggest an underlying split cord malformation. A hairy tuft high along the back is strongly associated with diastematomyelia type I or II. Hydromyelia is a common finding and can involve one or both hemichords and the normal cord above and below the splitting.
Diastematomyelia Type II
Type II diastematomyelia (diastematomyelia without osteocartilaginous septum) consists of two hemichords contained within a single dural sac without an intervening rigid midline septum. There are three variants of type II diastematomyelia: presence of a fibrous septum, absence of a septum, and partial cord splitting. Absence of the septum is the most common type II variant. Type II will demonstrate the same cutaneous stigmata and hydromyelia that are seen with type I. Vertebral anomalies are present but are usually milder than in type I. The most common vertebral anomaly in type II is the butterfly vertebrae. Scoliosis is usually absent. Type II is strongly associated with lipomas of the filum terminale.
Imaging Features
Plain radiographs can be an important clue as to the presence of an underlying spinal abnormality. Widening of the interpediculate distance can be identified, as can vertebral anomalies such as hemivertebra and scoliosis ( Fig. 19-2 ) . A spur, if present, can be detected with plain radiography in less than 50% of cases ( Fig. 19-3 ) . Computerized tomography (CT) readily demonstrates an osteocartilaginous spur if present ( Fig. 19-4 ) as well as vertebral anomalies ( Fig. 19-5 ) . The split spinal cord can be seen with intervening CSF density ( Fig. 19-6 ) . This is more evident with the administration of intrathecal contrast media. CT is also helpful for defining the anatomy of the spur for presurgical planning.