1. What names have been given to this entity?
2. What is the significance of the type of fracture depicted in this child’s distal tibia?
3. What radiographic findings are the most specific for this entity?
4. What type of force is likely responsible for the distal tibial fracture depicted?
5. Which age group is at greatest risk for this entity?
Non-accidental trauma 2209
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

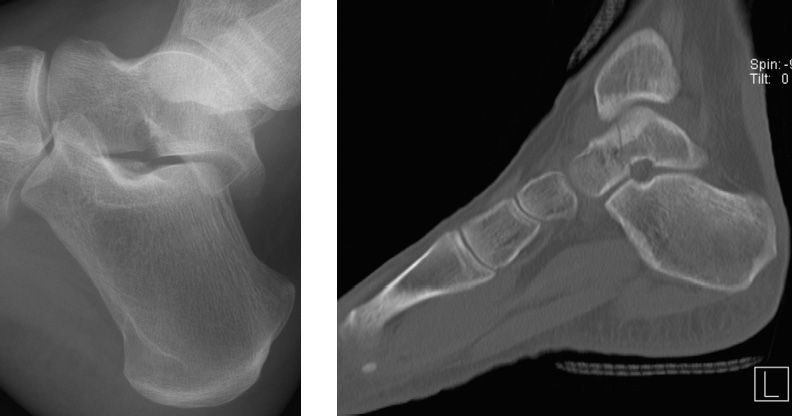
Radiograph demonstrates a fracture of the distal tibial metaphysis (arrows). The fracture has a “bucket-handle” appearance when imaged en face.

The fracture appears to involve the “corners” of the metaphysis (arrows) on the lateral projection.

Cortical stepoff of the distal radial metaphysis (arrow) consistent with fracture.

Healing fracture of the left clavicle (arrow).

Lateral skull radiograph in a different patient (a 17-day-old girl) demonstrates a depressed skull fracture (arrow).
Answers
1. Non-accidental trauma and non-accidental injury are terms used today to describe what has previously been called child abuse, battered child syndrome, or shaken baby syndrome.
2. The radiographs depict a metaphyseal fracture. Metaphyseal fractures (also called classic metaphyseal lesions or bucket-handle fractures) are considered highly specific for non-accidental trauma.
3. Metaphyseal fractures and rib fractures are considered very specific for non-accidental trauma.
4. The metaphyseal fracture is thought to result from shear force caused by to-and-fro shaking of the extremities, as when an adult shakes an infant. A series of microfractures develops into a fracture line in the subepiphyseal region parallel to the physis.
5. Younger children are at higher risk. Children younger than one year of age accounted for 46% of fatalities caused by abuse or neglect, and children younger than age four years accounted for 81%.
Suggested Readings
Dwek JR. The radiographic approach to child abuse. Clin Orthop Relat Res. 2011;469(3):776–789.
Lonergan GJ, Baker AM, Morey MK, Boos SC. From the archives of the AFIP. Child abuse: radiologic-pathologic correlation. Radiographics. 2003;23(4):811–845.
Motor vehicle accident
1. What are the imaging findings?
2. What is the mechanism of injury?
3. What injuries to the cervical spine are unstable?
4. In what injury is the hamburger sign seen?
5. What percentage of patients with bilateral injury have neurological compromise?
Jumped facet 2357
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

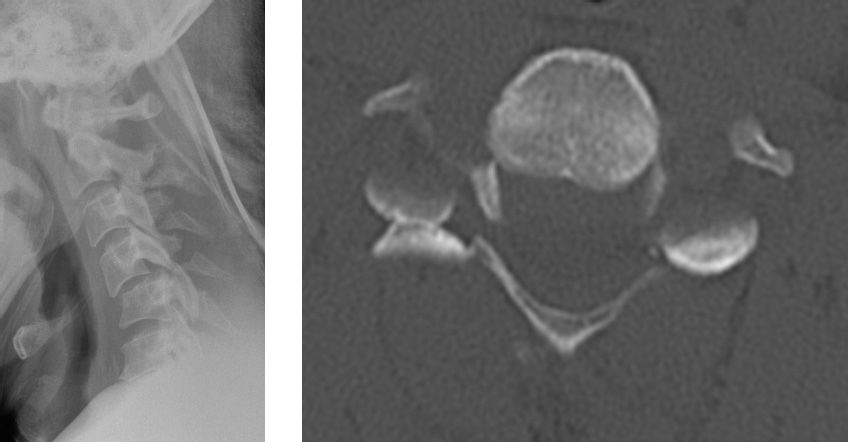
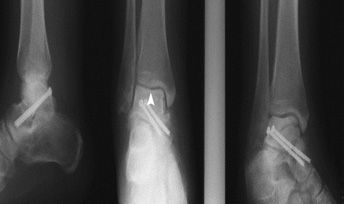
Anterolisthesis of C4 on C5, with a jumped facet (arrowhead) and multiple spinous process fractures.
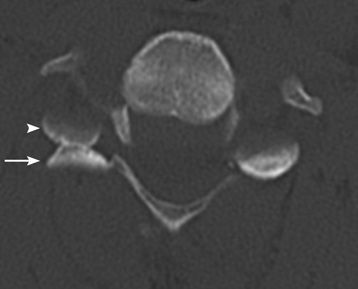
Right “hamburger” sign demonstrated. Arrowhead points to the inferior facet of the C4 vertebra, and the arrow points to the superior facet of C5.
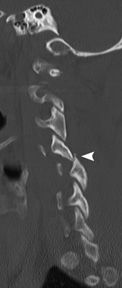
Jumped facet with an associated fracture (arrowhead).

Uncovered disc with bulging, minimal cord edema and no cord transection. Ligamentous injury (arrowheads).

Perched facet on the left side.
Answers
1. There is a hyperflexion injury with a jumped facet, anterolisthesis of C4 on C5 and multiple spinous process fractures. The “hamburger” and “naked facet” signs are the same and are demonstrated here.
2. The mechanism for this injury is hyperflexion. A rotary component to the injury is contributory.
3. Flexion teardrop, Jefferson and Hangman fractures, type 2 dens fractures, and bilateral locked facets are unstable fractures. A unilateral locked facet with a fractured facet is also unstable. In addition, hyperextension dislocation is unstable.
4. A “hamburger” sign is seen in a jumped facet. On axial CT, the normal appearance of the facets is said to resemble a hamburger, with the superior articular facet of the vertebra below forming the top bun and the inferior facet of the vertebra above forming the bottom bun, and the space between the “meat.” With a jumped facet, the bottom “bun” now lies anterior to the top “bun.” This is known as the hamburger or naked facet sign.
5. Of patients with bilateral jumped facets, 75% have neurological compromise. The listhesis that occurs results in severe canal and foraminal stenosis, with cord compression or transection in severe cases.
Suggested Readings
Kornberg M. The computed tomographic appearance of a unilateral jumped cervical facet (the “false” facet joint sign). Spine (Phila PA 1976). 1986;11(10):1038–1040.
Sekula RF, Daffner RH, Quigley MR, et al. Exclusion of cervical spine instability in patients with blunt trauma with normal multidetector CT (MDCT) and radiography. Br J Neurosurg. 2008;22(5):669–674.
History of a motor vehicle accident
1. What are the imaging findings?
2. What other significant injuries would you be looking for?
3. What vessels provide the major arterial supply to the talar dome?
4. What is the Hawkins sign?
5. What is the significance of a positive Hawkins sign?
Talar neck fracture: Hawkins type 1 1462
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

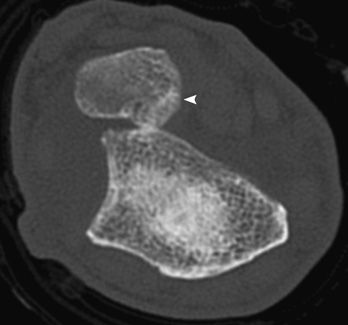
Minimally displaced talar neck fracture (arrowhead) and ankle effusion are seen.
Same patient (Hawkins type 3) postsurgical screw fixation shows anatomic alignment of the fracture but with sclerosis of the talar dome (arrowhead), which is consistent with avascular necrosis.

Nondisplaced fracture of the talar neck is seen.

Radiographs 6 weeks later shows subchondral talar dome lucency, which is a positive Hawkins sign.

Another patient with Hawkins type 3 fracture, including a displaced talar neck fracture and associated subtalar and ankle joint subluxation.
Answers
1. There is a minimally displaced talar neck fracture with a small ankle effusion.
2. Dislocation/subluxation of the subtalar, tibiotalar, or talonavicular joints and significant fracture displacement.
3. The artery of the tarsal canal, which is a branch of the posterior tibial artery, is the major blood supply to the talar dome. The artery of the tarsal sinus, which is a branch of the peroneal artery, is the secondary blood supply.
4. Subchondral lucency in the talar dome occurring six to eight weeks after injury is called a Hawkins sign.
5. A positive Hawkins sign indicates a low risk for avascular necrosis of the talar dome. The band-like lucency that is seen in the dome is a result of preserved vascular perfusion, resulting in bone resorption.
Suggested Readings
Donnelly EF. The Hawkins sign. Radiology. 1999;210(1): 195-196.
Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am. 1970;52(5):991–1002.
Fall from a tree

1. What are the imaging findings?
2. What is the accepted name for this injury?
3. What is the typical mechanism of injury?
4. What is a crisscross injury?
5. Are these injuries stable or unstable, and how are they treated?
Essex-Lopresti fracture–dislocation 2318
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma
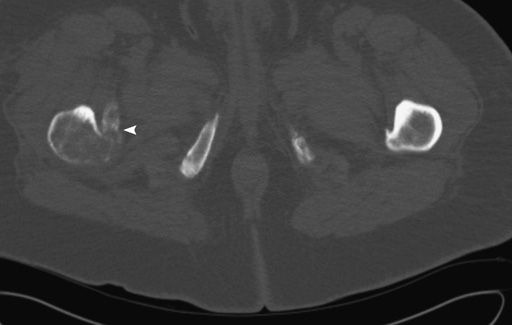
Volar dislocation of the distal ulna (arrowhead) at the DRUJ is well appreciated on CT.

Treated with excision of the radial head and placement of a radial head prosthesis.

DRUJ dislocation was reduced and pinned.
Answers
1. There is a comminuted displaced radial head fracture, with volar dislocation of the ulna at the distal radio-ulnar joint (DRUJ).
2. The combination of a comminuted displaced radial head fracture and DRUJ dislocation is called an Essex-Lopresti fracture–dislocation.
3. Essex-Lopresti injuries are usually the result of a high velocity fall on the outstretched hand such as in parachuting, skiing, and falls from a height. Longitudinal migration of the radius occurs in the classic injury, with interosseous membrane disruption. Hyperpronation results in a dorsal dislocation of the distal ulna, hypersupination in a volar dislocation—these are the other variants.
4. The rare crisscross injury is a dislocation of the radial head at the elbow, and of the ulna at the DRUJ. The radial head dislocation is usually volar with a volar distal ulna dislocation.
5. The injury to the interosseous membrane that occurs in an Essex-Lopresti fracture–dislocation renders the injury unstable. Management is usually surgical: reduction of the radial head fracture and/or excision and prosthetic replacement of the radial head, with reduction and pinning of the DRUJ.
Suggested Readings
Jungbluth P, Frangen TM, Arens S, Muhr G, Kälicke T. The undiagnosed Essex-Lopresti injury. J Bone Joint Surg Br. 2006;88(12):1629–1633.
Lendemans S, Taeger G, Nast-Kolb D. Dislocation fractures of the forearm. Galeazzi, Monteggia, and Essex-Lopresti injuries [in German]. Unfallchirurg. 2008;111(12): 1005–1014; quiz 1015–1016.
Patient fell while cleaning her garage

1. What are the radiograph findings?
2. What is the mechanism of injury?
3. The distal radius fracture is almost always located above what structure?
4. What is the treatment for this injury in an adult?
5. What is the injury pattern in an Essex-Lopresti injury of the forearm?
Galeazzi fracture–dislocation 1396
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

There is a displaced angulated fracture of the distal radius, with ulnar dislocation. An associated displaced ulnar styloid process fracture is seen (arrowhead).

The fracture is treated with open reduction and internal fixation. The dislocation has been reduced.

The radial height has been restored.
Answers
1. Displaced fracture of the distal radius, with dorsal dislocation of the distal ulna. This is a Galeazzi fracture–dislocation.
2. The typical mechanism is a fall on the outstretched hand while pronated. Direct trauma can sometimes result in this pattern.
3. The distal radius fracture is almost always located above the pronator quadratus muscle.
4. The management for a Galeazzi fracture–dislocation is open reduction and internal fixation in an adult. In a child, closed reduction and casting is performed.
5. An Essex-Lopresti forearm injury is a fracture of the radial head, accompanied by a dislocation of the distal ulna at the distal radioulnar joint. The interosseous membrane is injured.
Suggested Readings
Atesok KI, Jupiter JB, Weiss AP. Galeazzi fracture. J Am Acad Orthop Surg. 2011;19(10):623–633.
Carlsen BT, Dennison DG, Moran SL. Acute dislocations of the distal radioulnar joint and distal ulna fractures. Hand Clin. 2010;26(4):503–516.
Fall

1. What are the radiograph findings?
2. What is the mechanism of injury?
3. What can be included in the differential, and what is the most likely diagnosis?
4. What are the different forms of this injury, and what is the most common form?
5. What are the major complications of this injury pattern?
Monteggia fracture–dislocation 1395
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

Companion case: proximal ulna fracture with a posteriorly directed fracture apex and posterior dislocation and fracture of the radial head. This a reverse Monteggia fracture (Bado type 2).

Another patient treated with rigid fixation of the ulna fracture and excision of the radial head.
Answers
1. Angulated fracture of the proximal ulna with anterior and radial dislocation of the radial head, consistent with a Monteggia fracture dislocation.
2. A fall on the outstretched hand in hyperpronation and direct trauma to the back of the elbow are the proposed mechanisms.
3. Essex-Lopresti injury, Galeazzi fracture–dislocation, and elbow dislocation are included in the differentials. A Monteggia fracture–dislocation is the diagnosis.
4. Bado described four forms, with type 1 being the most common.
• Type 1: Fracture of the proximal ulna diaphysis with anterior radial head dislocation.
• Type 2: Fracture of the proximal ulna diaphysis with posterior or posterolateral dislocation of the radial head.
• Type 3: Fracture of the proximal ulna metaphysis with lateral or anterolateral radial head dislocation.
• Type 4: Fracture of the proximal radius and ulna at the same level with anterior radial head dislocation. This is least common.
5. Complications include injury to the radial, median, and ulnar nerves, fracture nonunion and heterotopic ossification.
Suggested Readings
Beutel BG. Monteggia fractures in pediatric and adult populations. Orthopedics. 2012;35(2):138–144.
Sferopoulos NK. Monteggia type IV equivalent injury. Open Orthop J. 2011;5(5):198–200.
Acute right hip pain with no history of significant trauma

1. What are the radiological findings?
2. What are the usual etiologies for this appearance?
3. What are the next appropriate steps?
4. What is the main risk when this appearance is seen?
5. What is the management?
Lesser trochanter avulsion: metastatic disease 1363
Case ranking/difficulty: ![]()
![]() Category: Bone tumors and marrow abnormalities
Category: Bone tumors and marrow abnormalities

There is avulsion of the lesser trochanter (arrow). Focal osteolysis of the proximal femur with cortical thinning is noted (arrowhead).
Osteolytic lesion with cortical destruction and lesser trochanter avulsion (arrowhead).
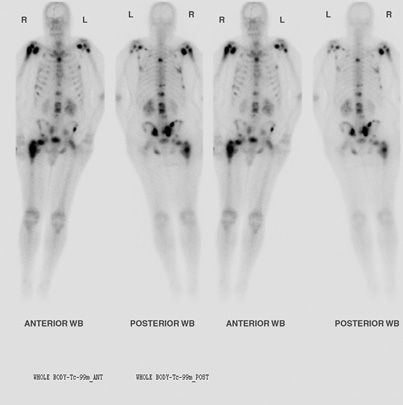
Diffuse metastatic foci are demonstrated.
Answers
1. There is an avulsion fracture of the lesser trochanter, with an osteolytic lesion in the proximal femur. There is cortical thinning.
2. In a patient older than age 40 years, lesser trochanter avulsion with minor or no trauma is highly suspicious for metastasis or primary bone tumor. In an adolescent, this may occur after strenuous hip flexion and is not pathologic.
3. Because this fracture is highly suspicious for underlying neoplasm, correlation for a history of neoplasm is warranted. If there is none, then further investigation with a bone scan is needed to evaluate for additional lesions. CT or MRI is indicated to assess the local extent of the lesion, and to determine the risk for pathologic fracture.
4. The main risk is an additional pathological fracture of the proximal femur.
5. Because of the high risk for pathologic fracture, prophylactic fixation of the femur is usually indicated.
Suggested Readings
Khoury JG, Brandser EA, Found EM, Buckwalter JA. Non-traumatic lesser trochanter avulsion: a report of three cases. Iowa Orthop J. 1998;18(18):150–154.
Phillips CD, Pope TL, Jones JE, Keats TE, MacMillan RH. Nontraumatic avulsion of the lesser trochanter: a pathognomonic sign of metastatic disease? Skeletal Radiol. 1988;17(2):106–110.
History of a chronic disease, and sudden heel pain with no trauma
1. What are the pertinent radiograph findings?
2. What is the diagnosis?
3. What are predisposing factors for this entity?
4. What is the average time between the mean age of diabetes onset and the development of this fracture?
5. What is the definitive treatment?
Calcaneal insufficiency avulsion fracture 1532
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

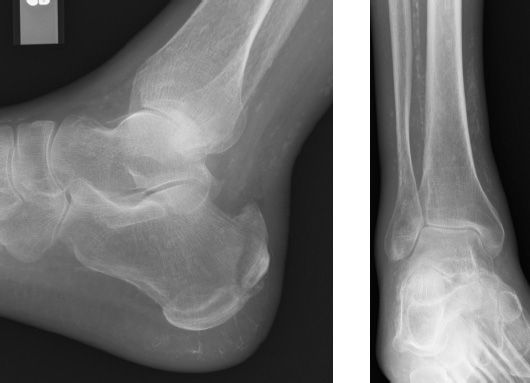
There is an acute, vertically oriented, and mildly displaced fracture of the posterior superior calcaneus. There is extensive vascular calcification.

Radiograph taken three months later shows further displacement of the fracture.

Lateral film of the contralateral side shows no fracture.
Answers
1. Vertically oriented, mildly displaced fracture of the posterior superior calcaneus, with vascular calcifications indicating the patient’s diabetic status.
2. The diagnosis is a calcaneal insufficiency avulsion fracture (CIAF).
3. Diabetes mellitus, neuropathic foot, vascular insufficiency, soft-tissue infection, and osteoporosis are all contributory.
4. Average time from diabetes diagnosis to calcaneal avulsion fracture is 20 years.
5. Nondisplaced fractures can be treated conservatively and with good diabetes control, but the general tendency for this fracture to be displaced usually means surgical fixation is required.
Suggested Readings
Arni D, Lambert V, Delmi M, Bianchi S. Insufficiency fracture of the calcaneum: Sonographic findings. J Clin Ultrasound. 2009;37(7):424–427.
Kathol MH, el-Khoury GY, Moore TE, Marsh JL. Calcaneal insufficiency avulsion fractures in patients with diabetes mellitus. Radiology. 1991;180(3):725–729.
History of anterior knee pain after running

1. Which age group is commonly affected in this condition?
2. What is the proposed mechanism?
3. What are the typical radiological findings?
4. What is the significance of this injury?
5. What is the next most appropriate study?
Patella sleeve avulsion fracture 1345
Case ranking/difficulty: ![]()
![]() Category: Trauma
Category: Trauma

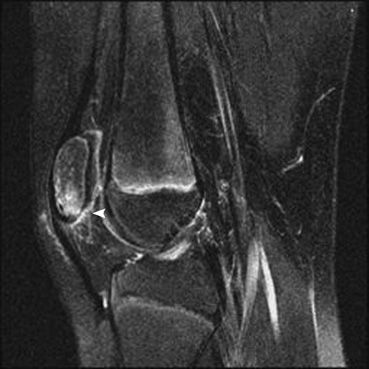
There is an avulsion fracture from the patella lower pole (arrow). Mild soft-tissue swelling is seen. Anterior patella density is an ossification center (arrowhead).

Another patient with a patella sleeve avulsion. (Courtesy of Children’s Hospital of Philadelphia.)
Osteochondral fracture well appreciated. The cartilaginous injury is minimal in this older patient. (Courtesy of Children’s Hospital of Philadelphia.)
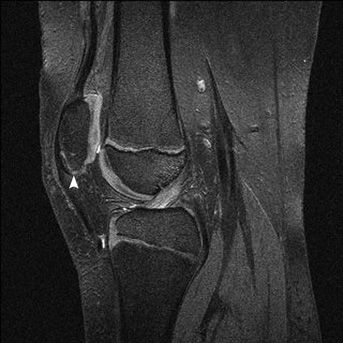
Osteochondral fracture. (Courtesy of Children’s Hospital of Philadelphia.)
Answers
1. Patella sleeve avulsions are most common in the 8- to 12-years age group.
2. Patella sleeve avulsion results from a forced quadriceps contraction on a flexed knee. Sinding-Larsen-Johansson syndrome is an osteochondrosis of the lower pole of the patella affecting individuals aged 10 to 14 years.
3. Plain film radiographic findings of a patella sleeve avulsion include an avulsion fracture at the patella, soft-tissue swelling and joint effusion. Patella alta could be seen in some cases, if the patella tendon and its associated osseous fragment are completely avulsed.
4. The significance of a patella sleeve avulsion is that the cartilaginous and soft-tissue involvement is often disproportionate to the bony avulsion. Therefore, MRI is often necessary to assess the extensor mechanism and patella cartilage.
5. An MRI is often necessary to assess the extensor mechanism and patella cartilage, which may be injured in excess of the perceived osseous injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree