Diffuse Alveolar Hemorrhage
Tan-Lucien H. Mohammed, MD, FCCP
Key Facts
Terminology
Classifications based on immune status, immune complexes, histology, or presence of glomerulonephritis (pulmonary-renal syndrome)
Imaging Findings
CT patterns nonspecific; specific clinical diagnosis cannot be made
Acute hemorrhage
Lobular ground-glass opacities often admixed with dense consolidation
Edge of opacity typically ground-glass
Resolution: Over 24-48 hours develop interlobular & intralobular interstitial thickening superimposed on ground-glass opacities (“crazy-paving” pattern)
Top Differential Diagnoses
Cardiogenic Pulmonary Edema
Pulmonary Edema, Noncardiac
Pulmonary Infection: Viral or Pneumocystis
Pathology
Hemorrhage into alveolar spaces (ground-glass opacities to consolidation)
Blood removed from alveoli by macrophages (2-3 days)
Macrophages migrate into interstitium (septal thickening)
Macrophages removed by lymphatics (7-14 days)
Lung returns to normal
Repeat or chronic hemorrhage
Mild to moderate fibrosis, hemosiderosis
Clinical Issues
Hemoptysis (66%)
TERMINOLOGY
Abbreviations and Synonyms
Diffuse alveolar hemorrhage (DAH), diffuse pulmonary hemorrhage
Definitions
Pulmonary hemorrhage that originates from alveolar capillaries
Classifications based on immune status, immune complexes, histology, or presence of glomerulonephritis (pulmonary-renal syndrome)
Must rule out aspiration of blood from localized source
Sources include bronchiectasis, angiosarcoma or Kaposi sarcoma, infections (angioinvasive aspergillosis), nasal, & esophageal varices aspiration
IMAGING FINDINGS
General Features
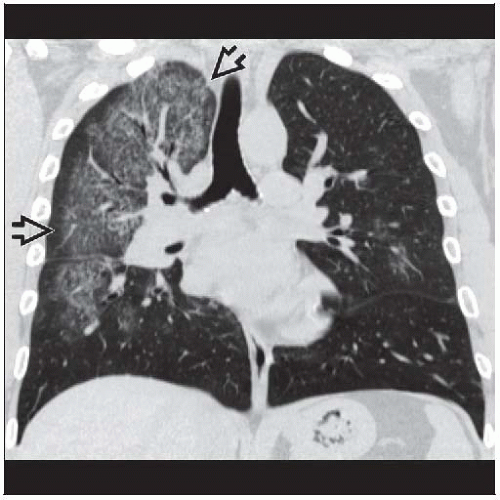
Best diagnostic clue: Acute onset of bilateral consolidation with apical sparing in anemic patient
CT Findings
CT patterns nonspecific; specific clinical diagnosis cannot be made
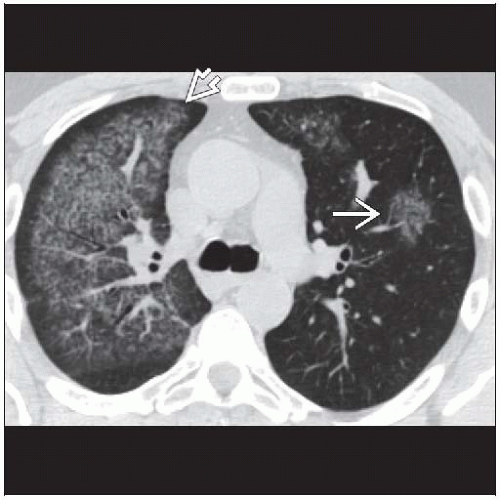
Acute hemorrhage
Lobular ground-glass opacities often admixed with dense consolidation
Edge of opacity typically ground-glass
High density from acute hemorrhage rare
Opacities tend to be gravity dependent
Prominent segmental and subsegmental bronchi (dark bronchus sign)
Spares costophrenic angles and lung periphery
Prominent septal lines suggest underlying mitral stenosis or leukemic pulmonary involvement
Pleural effusions and mediastinal adenopathy rare
Normal heart size
Resolution
Over 24-48 hours develop interlobular & intralobular interstitial thickening superimposed on ground-glass opacities (“crazy-paving” pattern)
Complete resolution from 48 hours to several days
Interlude between hemorrhages
Ill-defined 1-3 mm centrilobular nodules from intraalveolar accumulation of macrophages
Nodules diffuse, no zonal predominance
Chronic hemorrhage
Interlobular thickening with traction bronchiectasis from fibrosis
Interstitial thickening may have nodular calcification (from hemosiderosis, especially in longstanding mitral stenosis)
Radiographic Findings
May be normal; abnormal radiographic findings not specific
Acute bilateral consolidation with apical sparing
Typically perihilar distribution (“bat wing”)
Consolidation may be focal or asymmetric
Pleural effusions rare
Prominent Kerley B lines: Consider mitral stenosis
Resolution variable from 48 hours to several days
Consolidation evolves into interstitial pattern (Kerley B lines)
Radiograph returns to normal
Chronic bleeding or recurrent episodes may result in permanent reticular opacities (from fibrosis)
1st manifestation usually in airspace (consolidation or ground-glass opacities)
May begin as reticulonodular interstitial thickening, especially in bone marrow transplantation
Localized hemorrhage source
Focal abnormality (mass, cavity, atelectasis, consolidation) (60%)
MR Findings
No important role in evaluation of DAH
Intermediate signal on T1-weighted sequences and low signal on T2-weighted (iron susceptibility effect)
Pulmonary edema and pneumonia often demonstrate high signal on T2
Imaging Recommendations
Best imaging tool
Chest radiograph usually sufficient for detection
Thin-section CT: More sensitive and possibly more specific
DIFFERENTIAL DIAGNOSIS
Cardiogenic Pulmonary Edema
Cardiomegaly, bilateral gravity-dependent opacities, septal thickening, and pleural effusion
Resolves rapidly with therapy
Hemorrhage will not shift with gravity (gravitational shift test) as opposed to edema
Pulmonary Edema, Noncardiac
Septal lines less common
Favors lung periphery
Pulmonary Infection: Viral or Pneumocystis
Fever, chills, productive cough, and elevated white blood cell count common
Evolution from consolidation to reticular pattern is unusual
PATHOLOGY
General Features
General path comments
Hemorrhage in airspaces and hemosiderin-laden macrophages in airspaces and interstitium
Hemosiderin appears within 48 hours after bleeding
Etiology
Pathologic correlation
Hemorrhage into alveolar spaces (ground-glass opacities to consolidation)
Blood removed from alveoli by macrophages (2-3 days)
Macrophages migrate into interstitium (septal thickening)
Macrophages removed by lymphatics (7-14 days); lung returns to normal
Repeat or chronic hemorrhage: Mild to moderate fibrosis, hemosiderosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree