Case presentation
A 4-year-old female presents with the parents noting that the child has been “not walking right” and “wobbly” for the past 3 weeks. She sustained a head injury 1 month prior to her current presentation but there was no reported loss of consciousness at that time and the fall was off a chair, onto a hardwood floor, less than 2 feet. At the time, she did not appear injured and had been at her baseline until the onset of current symptoms. There has been no reported fever, recent illness, emesis, neck pain, back pain, or incontinence. The family has noted that her “eyes look funny” and she appears to “have trouble focusing her vision.” She also has been drooling (new for this child) and seems to have difficulty speaking, which is also new for the child as she has been developmentally appropriate.
Physical examination reveals age-appropriate vital signs and the child is in no overall distress. She is normocephalic and there are no signs of trauma. Pupils are round and equally reactive to light and there is no photophobia. The child has bilateral ptosis and she appears to have difficulty focusing her vision on objects. She has equal tone and strength throughout, but when she ambulates, she is ataxic and has dysmetria. She is drooling and is difficult to understand when she speaks.
Imaging considerations
Imaging is often employed in patients with general neurologic complaints, such as severe headache, and focal neurologic findings (such as ataxia or abnormal neurologic examination), or if there are symptoms that raise suspicion for an intracranial process, such as emesis, vision changes, or concerning historical findings (such as awakening in the middle of the night with headache, first morning emesis, or persistent/worsening headache). Imaging options include computed tomography (CT) and magnetic resonance imaging (MRI); which modality is employed depends largely on history, physical examination, and institutional resources.
While the use of neuroimaging has become commonplace for the evaluation of a variety of symptoms in pediatric patient populations, including concussion, , first-time seizures, , headache, , and dizziness, , neuroimaging may not be indicated in all patients. Several studies looking at acute and subacute ataxia in pediatric patients found conditions that required intervention in approximately 13% of patients imaged. , Of note, the clinical features most predictive of imaging abnormalities were the age of the child (older children had more significant intracranial pathology), the duration of symptoms (more than 3 days was significant), and the presence of additional neurological signs on examination, such as cranial nerve deficits or hemiparesis. , Cranial nerve deficits are associated with a variety of intracranial pathologies, including demyelinating disease and tumors; more than 80% of children with space-occupying tumors will have signs of increased intracranial pressure, in addition to ataxia. , Therefore it is a constellation of symptoms and examination findings that leads the clinician to suspect an intracranial process, rather than individual symptoms alone.
Plain radiography
This modality has no role in the evaluation of pediatric patients with focal neurologic findings.
Computed tomography
CT is often used as a first-line imaging modality to detect intracranial pathology. This modality is readily available in most urgent and emergent settings and sedation is not required. If an intracranial mass is suspected, a non—contrast study can be utilized.
Magnetic resonance imaging
MRI is the preferred method to visualize intracranial pathology, including brain tumors, and is often obtained following the detection of a brain mass on CT. In cases with a high index of suspicion, MRI is appropriate as an initial imaging test or after a CT with unrevealing or nonspecific findings. Conventional MRI techniques can provide anatomic information regarding dimensions and location of a brain tumor; advanced MRI imaging techniques, such as diffusion-weighted imaging, functional MRI, and diffusion tensor imaging, can be utilized to provide physiologic information regarding hemodynamics and cellularity. Barriers to MRI use include the time necessary to complete a study and lack of immediate availability in many cases. In young children, sedation is often required to complete the study.
Imaging findings
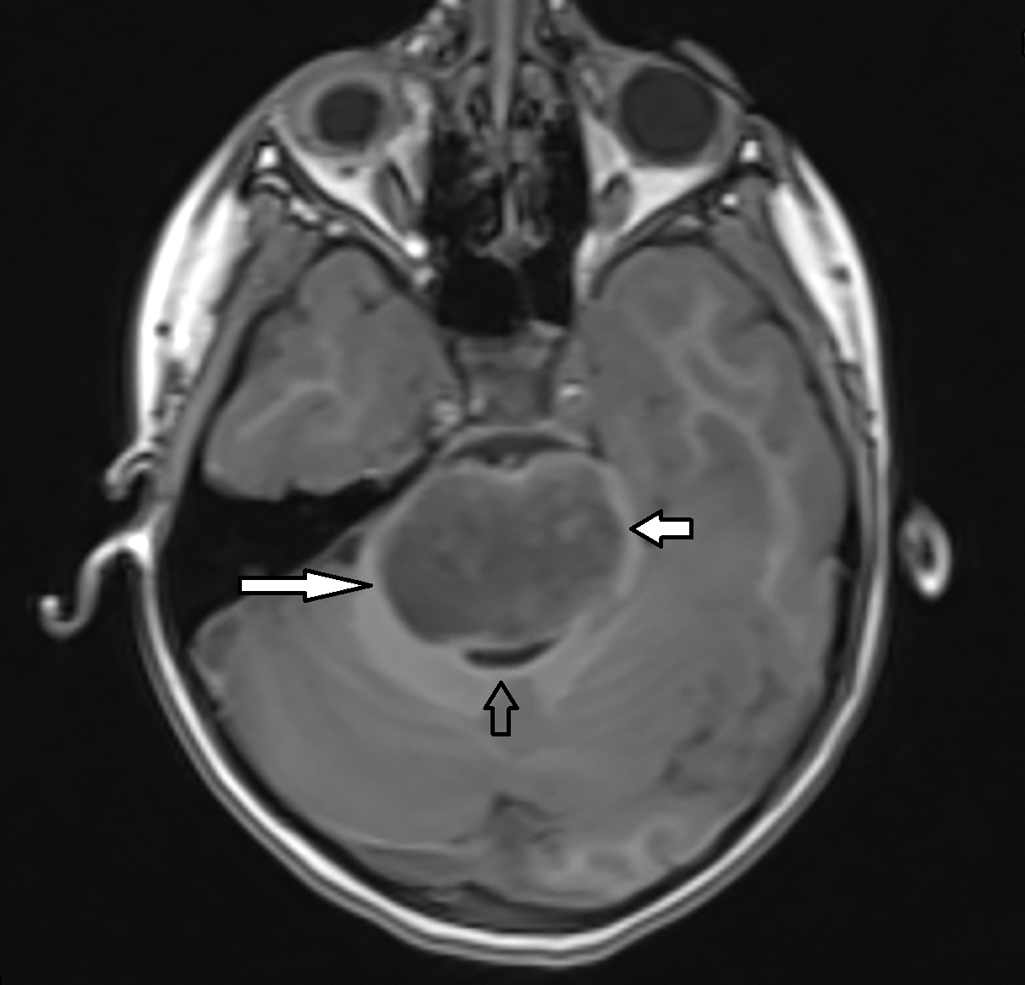
The child’s history and physical examination were concerning for an intracranial process, especially a space-occupying lesion. A non—contrast CT scan was obtained and selected images are provided. There is diffuse enlargement and low attenuation throughout the brainstem, but particularly in the pontine region, and there is compression and effacement of the fourth ventricle but no hydrocephalus; these findings are concerning for a brainstem glioma ( Fig. 29.1 ).
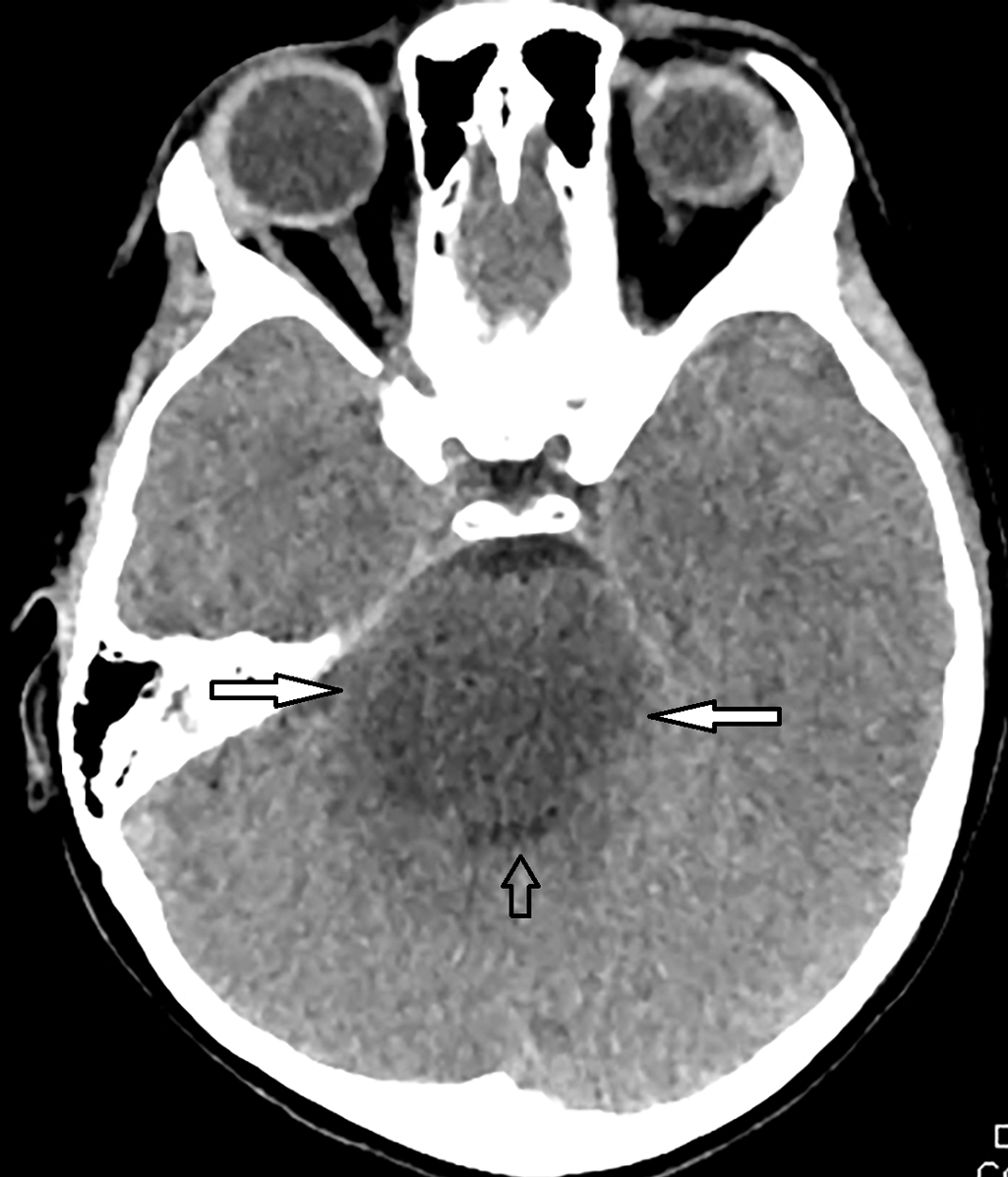
In light of these imaging findings, the child underwent MRI of the brain and spine with and without intravenous (IV) contrast. Selected images are provided. Sedation was required to complete the study. This study demonstrated a large T2 hyperintense pontine mass without enhancement or hemorrhage, with some exophytic extension around the basilar artery, and compression of the fourth ventricle without hydrocephalus ( Figs. 29.2 and 29.3 ). There is no cerebrospinal fluid dissemination of the tumor.