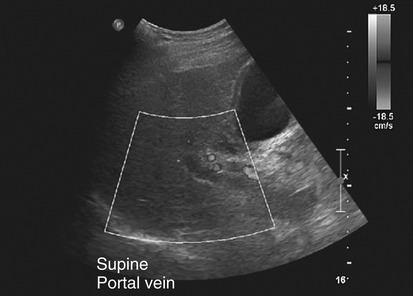
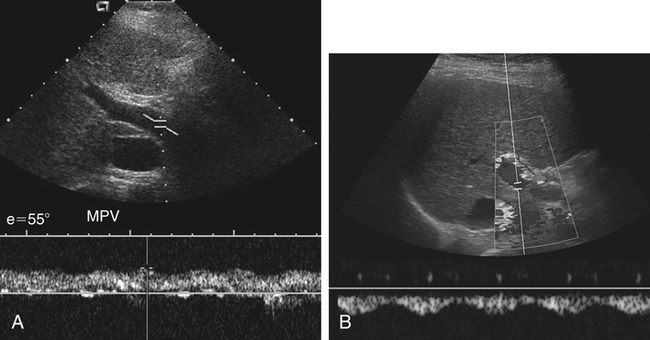
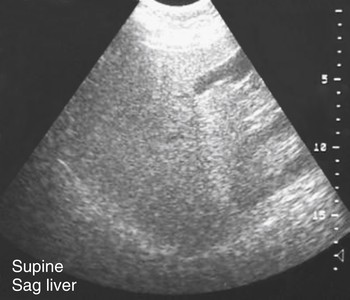
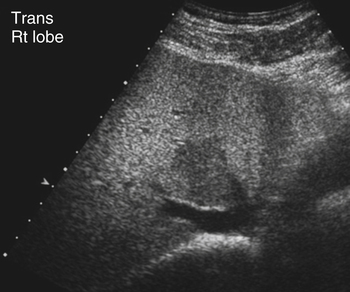
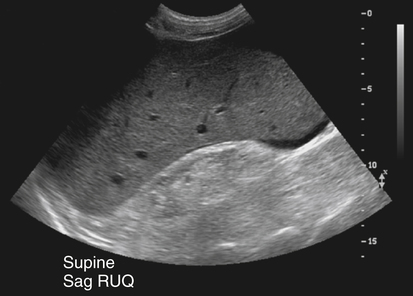
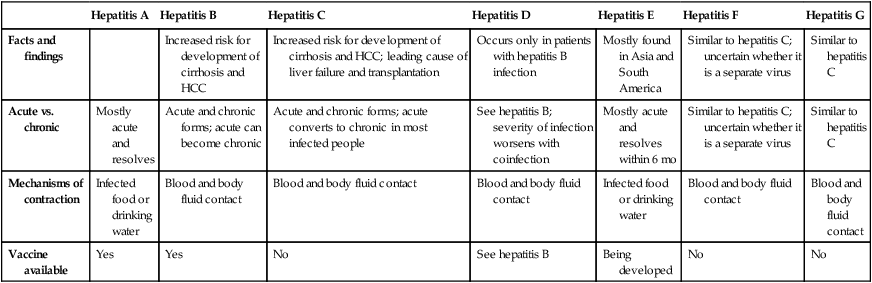
Felicia Toreno and Kathryn Kuntz • Define the processes that cause and affect diffuse liver disease. • Define and describe hepatocellular diseases and their sonographic findings. • Compare and contrast the various diffuse liver diseases and their sonographic appearances. • Understand and describe the changes in laboratory values associated with diffuse liver diseases. • Describe the changes in portal venous circulation that accompany diffuse liver diseases. • Define and describe the sonographic findings associated with conditions caused by diffuse liver diseases. Because many laboratory values are likely to be altered by a wide variety of diseases, other laboratory values in addition to liver function values should be considered in determining a definitive diagnosis. For example, increased white blood cell (WBC) levels may indicate infection or abscess in the liver. When diffuse liver disease is suspected, it is imperative that a good clinical history and laboratory values accompany a thorough assessment with sonography. Table 3-1 provides a guide to laboratory values related to diffuse liver disease. TABLE 3-1 Liver-Related Laboratory Values The liver may be enlarged especially in acute stages of hepatocellular disease. In some diseases, such as hepatitis, sonographic findings in the acute stage may be subtle and difficult to detect. The liver often becomes atrophied as pathologic changes become chronic, and the hepatocytes are replaced either by fat cells or by fibrous tissue (Fig. 3-4). Over time, replacement of the hepatocytes by fat and fibrous components leads to decreased liver function and an increase in liver enzymes. Liver cells regenerate, and this process may be accompanied by the development of regenerating liver nodules. The presence of these nodules further complicates the sonographic evaluation of the liver parenchyma and sonographic assessment of the liver for possible masses. Ascites, the accumulation of free fluid within the abdominal cavity, may develop as pressure within the liver increases, and serous fluids leak from the hepatocytes into the surrounding peritoneal cavity. This condition may be due to low levels of albumin (hypoalbuminemia) or severe portal hypertension. The increased pressure within the liver causes the fluids to leak from the liver sinuses into the hepatic lymphatics. When the pressure is high enough, some fluids leak directly into the peritoneal cavity (Fig. 3-5). The increasing pressure within the portal venous system may prevent blood from flowing in its normal direction, hepatopetal, which is toward the liver. Patients with suspected diffuse liver disease should undergo evaluation with color or spectral Doppler, which may detect hepatofugal, or reverse, blood flow in the portal-splenic circulatory system (Fig. 3-6; see Color Plate 2). These patients may develop vascular collateral channels to supply the liver with blood. Patients with impaired blood flow may undergo surgical placement of shunts or transjugular intrahepatic portosystemic shunt (TIPS) placement to help return portal blood to the systemic circulation. The appearance of diffuse fatty infiltration of the liver varies from mild to severe. The fatty replaced liver has increased echogenicity because of increased attenuation of the sound beam, as seen in Figure 3-4. As fatty replacement becomes more severe, the liver is difficult to penetrate, and the vascular structures are poorly visualized, especially the hepatic veins (Fig. 3-7). In some instances, the entire liver is not affected, and areas of the liver may be spared from fatty infiltration. These fat-spared areas appear as localized regions of decreased echogenicity within the fatty echogenic liver (Fig. 3-8). This fat sparing is often seen anterior to the gallbladder and the right portal vein, or within the left lobe. The multiple variations of hepatitis (hepatitis A to G) vary in severity and sonographic findings (Table 3-2). The most common forms of hepatitis are A, B, and C. Hepatitis A is a contagious liver disease that results from infection with the hepatitis A virus. It can range in severity from a mild illness lasting a few weeks to a severe illness lasting several months. Hepatitis A is usually spread when a person ingests fecal matter (even in microscopic amounts) from contact with objects, food, or drinks contaminated by the feces or stool of an infected person. TABLE 3-2 The liver may be enlarged and may show decreased echogenicity (Fig. 3-9), although it often appears normal in echo texture. Because of an accumulation of fluid within the hepatocytes, the walls of the gallbladder may thicken and appear prominent. Periportal cuffing, or thickening of the portal vein walls, may be noted, and the walls of the portal veins may appear more hyperechoic than normal, which is referred to as the “starry sky” appearance.
Diffuse Liver Disease
Diffuse Liver Disease
Test
Significance of Change
Alkaline phosphatase
↑ in liver disease
Ammonia
↑ in liver disease and diabetes mellitus
Bile and bilirubin
↑ during obstruction of bile ducts
Glucose
↑ in diabetes mellitus and liver disease
Hematocrit
↓ in cirrhosis of liver
Hemoglobin
↓ in cirrhosis of liver
Iron
↑ in liver disease
Lactic dehydrogenase
↑ in liver disease
Cholesterol
↑ in chronic hepatitis
↓ in acute hepatitis
Platelet count
↑ in cirrhosis of liver
Transaminase
↑ in liver disease
Urea
↑ in some liver diseases
↓ during obstruction of bile ducts
Hepatocellular Disease

Fatty Liver Disease
Sonographic Findings
Hepatitis
Hepatitis A
Hepatitis B
Hepatitis C
Hepatitis D
Hepatitis E
Hepatitis F
Hepatitis G
Facts and findings
Increased risk for development of cirrhosis and HCC
Increased risk for development of cirrhosis and HCC; leading cause of liver failure and transplantation
Occurs only in patients with hepatitis B infection
Mostly found in Asia and South America
Similar to hepatitis C; uncertain whether it is a separate virus
Similar to hepatitis C
Acute vs. chronic
Mostly acute and resolves
Acute and chronic forms; acute can become chronic
Acute and chronic forms; acute converts to chronic in most infected people
See hepatitis B; severity of infection worsens with coinfection
Mostly acute and resolves within 6 mo
Similar to hepatitis C; uncertain whether it is a separate virus
Similar to hepatitis C
Mechanisms of contraction
Infected food or drinking water
Blood and body fluid contact
Blood and body fluid contact
Blood and body fluid contact
Infected food or drinking water
Blood and body fluid contact
Blood and body fluid contact
Vaccine available
Yes
Yes
No
See hepatitis B
Being developed
No
No
Sonographic Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Diffuse Liver Disease