From a radiographic standpoint, it is most useful to classify amyloidosis on the basis of the abnormalities it produces. In general, pulmonary amyloidosis is classified
into three types: (1) diffuse or alveolar septal amyloidosis, (2) localized nodular amyloidosis, and (3) tracheobronchial amyloidosis.
Diffuse (Alveolar Septal) Amyloidosis
Symptoms of respiratory insufficiency are common with diffuse or alveolar septal amyloidosis, and may be related to diffuse lung disease or associated cardiac involvement. This form of amyloidosis is most often related to primary systemic amyloidosis (systemic AL). Diffuse lung involvement is much less common and may be incidental with AA amyloidosis or senile amyloidosis. Occasionally, diffuse alveolar septal amyloidosis reflects localized rather than systemic disease.
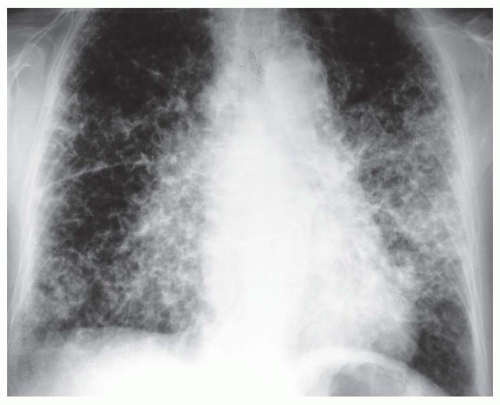
The lung may be diffusely involved in the absence of a radiographic abnormality. If radiographs are abnormal, a reticular or reticulonodular pattern typically is seen, usually bilateral and diffuse or with a basal and subpleural predominance (
Figs. 21-1 and
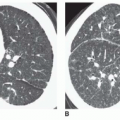
21-2A). Focal or patchy areas of consolidation also may be seen. The abnormal areas can calcify or, rarely, show frank ossification. Less often, a small nodular pattern mimicking sarcoidosis or miliary tuberculosis may be seen.
Hilar or mediastinal lymph node enlargement may be seen in patients with AL, either as an isolated finding or in association with interstitial disease. Cardiac infiltration with heart failure may result in pulmonary edema or pleural effusion.
On HRCT, the most common pulmonary manifestations of diffuse parenchymal amyloidosis consist of multiple small nodules, usually ranging from 2 to 4 mm in diameter (see
Fig. 21-2B and C), interlobular septal thickening, fine reticular opacities, focal consolidation, foci of calcification within nodules or areas of consolidation (
Fig. 21-3), and traction bronchiectasis. A subpleural and basal predominance may be seen.
Progression of the diffuse parenchymal disease typically occurs with time, with an increase in the reticular opacities, septal thickening, the size and number of nodules, the extent of consolidation, and the size and number of calci-fications.
As on chest radiographs, other findings seen on CT include lymphadenopathy, lymph node calcification (
Fig. 21-4), and pleural effusion. Lymph node enlargement occurs in up to 75% of cases.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access