Diseases of the Chest Wall and Diaphragm
Janet E. Kuhlman
John H. Juhl
J. E. Kuhlman and J. H. Juhl: Department of Radiology, University of Wisconsin Medical School, Madison, Wisconsin 53792-3252.
The chest wall and diaphragm are affected by a wide variety of conditions, including infectious and inflammatory diseases and primary and secondary malignancies. Diagnosis and characterization of chest wall masses by conventional chest radiography is limited, and cross-sectional imaging with computed tomography (CT) or magnetic resonance imaging (MRI), or both, is frequently needed. Chest wall invasion by lung cancer, recurrent breast cancer, or lymphoma is a common clinical question that may be difficult to answer with conventional radiographs. Other practical issues involving the chest wall include determining the cause of brachial plexopathy and delineating the extent of infections and inflammatory diseases. This chapter also reviews the anatomy of the diaphragm and the pathologic conditions that affect it, such as diaphragmatic hernias and processes that transgress the diaphragm.
OVERVIEW OF THE CHEST WALL
Chest wall disease is often first detected with plain films of the chest.52 Initial evaluation may identify rib and bone anomalies as well as underlying lung pathology that may be associated with a chest wall lesion.52 Plain-film findings of an extrapulmonary chest wall mass include the incomplete border sign. The chest wall mass loses its sharp outline where it interfaces with the soft tissues of the chest wall, but keeps its sharp outline where it is silhouetted by the lung. Extrapulmonary chest wall masses tend to have smooth, tapered borders and to displace both the parietal and visceral pleura inward. Plain-film evaluation of most chest wall conditions is limited and must be supplemented by further cross-sectional imaging with CT or MRI. Often, CT and MRI play complementary roles in the evaluation of chest wall processes.10,27,52 The advantages of MRI in evaluating chest wall conditions include direct multiplanar capabilities, improved soft-tissue contrast characterization, and flow-sensitive pulse sequences that allow the detection of blood flow without the use of catheters or intravenous contrast agents.10,27,48,52 CT evaluation of chest wall disease, on the other hand, provides images with higher spatial resolution and depicts cortical bone erosion better than MRI does.10,27,52 Spiral CT datasets can also be obtained during a single breath hold, allowing the generation of multiplanar and three-dimensional images to evaluate the extent and severity of disease.
Computed Tomographic Techniques for Evaluating Chest Wall Disease
Newer CT techniques such as spiral/helical scanning allow faster imaging of the chest wall during a single breath hold and can be used to generate multiplanar reconstructions that are free of respiratory motion artifact. Helical scanning protocols vary depending on the manufacturer, but for a routine evaluation, typical scanning parameters are a slice thickness of 7 mm, a table speed of 9.8 mm/second (pitch of 1.4), and a reconstruction interval of 7 mm. Additional scans with thin collimation (1 to 3 mm) can be done as needed, and these may be particularly critical for evaluation of apical masses for chest wall invasion. The use of an intravenous contrast agent is essential for the evaluation of most chest wall problems to delineate the extent of chest wall disease and to opacify important vascular structures. It is most effectively administered by a power injector, with 100 to 150 mL of iodinated contrast material (300 mg iodine per milliliter) injected at a rate of 2–3 mL/second.17,20
Magnetic Resonance Imaging Techniques for Evaluating Chest Wall Disease
No standard MRI technique for evaluating chest wall disease exists. Each examination should be tailored to the clinical question in order to choose the appropriate pulse sequences,
imaging planes, slice thickness, field of view, and imaging coil.10,17,18,19,20,27 Many chest wall problems can be evaluated by traditional spin-echo sequences with the use of the body coil. However, newer surface, transmit-receive, and phased-array coils are available that provide images with higher signal-to-noise ratios and achieve higher spatial resolution. Torso and flexible coil configurations that wrap around the chest are excellent choices for many chest wall problems. Most examinations begin with large field-of-view images to survey the extent of the problem. These views are then supplemented with smaller field-of-view images in multiple planes. Frequently used pulse sequences include T1-weighted spin-echo sequences; T2-weighted spin-echo or fast spin-echo images; short T1 inversion recovery (STIR) sequences; and gradient-recalled acquisition in the steady state (GRASS) images for vascular assessment. Fast spin-echo sequences can often be substituted for the longer traditional spin-echo T2-weighted sequences, and magnetic resonance angiography techniques can be very useful in displaying the vascular supply of chest wall masses. Imaging planes (axial, coronal, sagittal, and oblique) are selected to best display the pathology and relevant anatomy. Slice thickness and interslice gap are adjusted to cover the region of interest. Cardiac gating along with respiratory compensation techniques are routinely used for chest imaging to minimize image artifacts. Gadolinium intravenous contrast enhancement may be helpful in differentiating recurrent tumor from scarring in the chest wall. 17,20
imaging planes, slice thickness, field of view, and imaging coil.10,17,18,19,20,27 Many chest wall problems can be evaluated by traditional spin-echo sequences with the use of the body coil. However, newer surface, transmit-receive, and phased-array coils are available that provide images with higher signal-to-noise ratios and achieve higher spatial resolution. Torso and flexible coil configurations that wrap around the chest are excellent choices for many chest wall problems. Most examinations begin with large field-of-view images to survey the extent of the problem. These views are then supplemented with smaller field-of-view images in multiple planes. Frequently used pulse sequences include T1-weighted spin-echo sequences; T2-weighted spin-echo or fast spin-echo images; short T1 inversion recovery (STIR) sequences; and gradient-recalled acquisition in the steady state (GRASS) images for vascular assessment. Fast spin-echo sequences can often be substituted for the longer traditional spin-echo T2-weighted sequences, and magnetic resonance angiography techniques can be very useful in displaying the vascular supply of chest wall masses. Imaging planes (axial, coronal, sagittal, and oblique) are selected to best display the pathology and relevant anatomy. Slice thickness and interslice gap are adjusted to cover the region of interest. Cardiac gating along with respiratory compensation techniques are routinely used for chest imaging to minimize image artifacts. Gadolinium intravenous contrast enhancement may be helpful in differentiating recurrent tumor from scarring in the chest wall. 17,20
Chest Wall Masses
The extrapleural space and the chest wall are composed of fat and soft tissues, including nerves, blood vessels, lymphatics, muscle, bone, cartilage, and fibrous connective tissue. Chest wall masses can arise from any of these component tissues.10,27,35,37 Typically, masses that are extrapleural displace both the parietal and visceral pleura as they expand into the thorax and create a lesion that forms obtuse angles with the chest wall on the chest radiograph and CT scans.10,27,35,37 Associated bony changes in the adjacent ribs are common because most chest wall masses arise in or near ribs, and this is the best plain-film finding of chest wall disease.
Lipomas
The most common chest wall mass is a benign lipoma52 (Figs. 34-1 and 34-2). Lipomas may be located in the subcutaneous fat or within the chest wall muscles, or they may insinuate through the ribs to become subpleural or intrathoracic masses. A more extensive growth of lipomatous tissue is called infiltrating lipomatosis. Often an intrathoracic lipoma can be suggested based on the plain-film appearance of a pedunculated intrathoracic mass which appears almost like a breast, with relatively more lucent radiographic density than the rest of the soft tissues of the chest. CT scanning readily confirms the fatty nature of the mass; CT attenuation of the mass is usually in the range of −100 to −160 Hounsfield units. Lipomas are also easily recognized on MRI by their signal intensity, which parallels that of subcutaneous fat on all pulse sequences: high signal on T1, high signal on proton-density, lower signal on more heavily weighted T2, low signal on STIR, and low signal on fat-saturation sequences. Chemical shift artifact should also be present at the interface of the fatty mass and surrounding water-containing soft tissues. Distinguishing between a benign lipoma and a liposarcoma, particularly a low-grade liposarcoma, is often difficult or impossible based solely on imaging characteristics. In general, however, benign lipomas are homogenous
in texture and signal characteristics, with little or no internal soft-tissue components. High-grade liposarcomas are more heterogeneous in their tissue composition and usually contain soft-tissue elements as well as fat. The pleochmorphic type of liposarcoma may contain little or no fat and may demonstrate only soft-tissue characteristics on CT and MRI.17,18,19,20
in texture and signal characteristics, with little or no internal soft-tissue components. High-grade liposarcomas are more heterogeneous in their tissue composition and usually contain soft-tissue elements as well as fat. The pleochmorphic type of liposarcoma may contain little or no fat and may demonstrate only soft-tissue characteristics on CT and MRI.17,18,19,20
Neurogenic Tumors
Neural tumors that cause chest wall masses may arise from the peripheral nerves of the chest wall, the intercostal nerves of the thoracic cage, the thoracic spine nerve roots, or the paraspinal ganglion of the sympathetic chain10,41 (Figs. 34-3 and 34-4). Neurofibromas, schwannomas (neurilemmomas), and neurofibrosarcomas arise from nerve roots. Neuroblastomas, ganglioneuromas, and ganglioneuroblastomas originate from sympathetic ganglia.11
 FIG. 34-3. Apical neurofibromas arising from the first intercostal nerves bilaterally. (From ref. 20, with permission.) |
 FIG. 34-4. Magnetic resonance image of plexiform neurofibroma infiltrating the chest wall (A) and left upper extremity (B). Neurogenic tumors are hyperintense on T2-weighted images. Neurofibromas also demonstrate a characteristic target sign, with a low-signal-intensity center within the bright tumor mass (arrow). (From ref. 20, with permission.) |
Depending on the type of nerve affected, the plain-film findings of neurogenic tumors may include rib erosions, rib notching, and rib sclerosis for those tumors arising from intercostal nerves.10,41 Neurofibromas can even mimic Pancoast tumors when they arise from the first or second intercostal nerves in the apex of the thoracic cage.41 Patients with neurofibromatosis often have more extensive involvement of the chest wall by plexiform neurofibromas that infiltrate widely. Malignant degeneration occurs in approximately 15% of patients with neurofibromatosis.10,41
Both CT and MRI are used to image neurogenic tumors, but in many cases MRI is the preferred modality to evaluate
the extent of chest wall involvement. The intramuscular extent of neurofibromas is more difficult to delineate with CT because of limited soft-tissue contrast. On the other hand, neurofibromas and other neurogenic tumors demonstrate very high signal intensity on T2-weighted images, which increases their conspicuity with respect to other soft tissues and muscle of the chest wall.10 MRI is also better able to demonstrate the intraspinal extent of neurogenic tumors without the need for myelography. CT more readily identifies small calcifications within neurogenic tumors and better delineates bone destruction. Marrow involvement by malignant neurogenic tumors is detected more accurately with MRI.10 Neurofibromas often demonstrate a typical feature on T2-weighted MRI images that has been called the “target sign”—a high-signal tumor mass with a central focus of low signal intensity10 (see Fig. 34-4). Pathologically, the low-signal target is probably caused by tightly packed collagen and Schwann cells within the center of neurofibromas, while the peripheral area of the tumor is composed of higher-signal myxoid tissue.
the extent of chest wall involvement. The intramuscular extent of neurofibromas is more difficult to delineate with CT because of limited soft-tissue contrast. On the other hand, neurofibromas and other neurogenic tumors demonstrate very high signal intensity on T2-weighted images, which increases their conspicuity with respect to other soft tissues and muscle of the chest wall.10 MRI is also better able to demonstrate the intraspinal extent of neurogenic tumors without the need for myelography. CT more readily identifies small calcifications within neurogenic tumors and better delineates bone destruction. Marrow involvement by malignant neurogenic tumors is detected more accurately with MRI.10 Neurofibromas often demonstrate a typical feature on T2-weighted MRI images that has been called the “target sign”—a high-signal tumor mass with a central focus of low signal intensity10 (see Fig. 34-4). Pathologically, the low-signal target is probably caused by tightly packed collagen and Schwann cells within the center of neurofibromas, while the peripheral area of the tumor is composed of higher-signal myxoid tissue.
Hemangiomas
Hemangiomas are uncommon lesions affecting the chest wall, but they may form in the skin, subcutaneous tissues, muscles, ribs, or synovium of joints.8,23,30 A spectrum of vascular malformations can occur, including cavernous hemangiomas and venous, arteriovenous, capillary, and mixed malformations (Fig. 34-5). Calcified phleboliths are occasionally identified in larger hemangiomas on chest radiographs.8,23,30 CT with intravenous contrast demonstrates an enhancing mass or serpiginous vessels, phleboliths, and underlying bone remodeling. 8,23,30 MRI often more accurately delineates the extent of soft-tissue hemangiomas, because these lesions typically demonstrate areas of very high signal intensity on T2-weighted images.8,10 The bright signal on T2 is thought to be caused by slow-flowing or stagnant blood within dilated vascular channels. Depending on their type and morphology, hemangiomas may demonstrate a mixture of MRI signals owing to the combination of vascular elements, fat, and connective tissues within the mass, as well as the presence of old blood, hemosiderin, and thrombus.8 A characteristic MRI feature of superficial hemangiomas is the presence of low-signal curvilinear structures on T1-weighted images that demonstrate high signal on T2-weighted images. Intramuscular lesions are frequently associated with muscle atrophy.8,17,20 Larger-vessel arteriovenous malformations show flow void in larger feeding vessels on T1-weighted images and high signal caused by fast flow on GRASS or gradient-flow-sensitive sequences (Fig. 34-5).
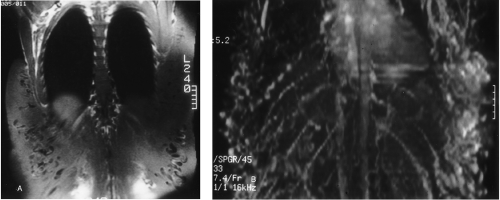 FIG. 34-5. Magnetic resonance image of chest wall arteriovenous malformation. Coronal T1-weighted (A) and magnetic resonance angiography (B) sequences demonstrate the extensive nature of the vascular malformation with numerous feeding vessels. (From ref. 17, with permission.) |
Lymphangiomas
Lymphangiomas are congenital malformations of the lymphatic system in which lymphatic saccules become sequestered from the rest of the lymphatic network38,46,53 (Fig. 34-6). Most commonly they appear as a neck mass in the infant, but lymphangiomas may extend from the neck into the supraclavicular fossa, the axilla, the chest wall, and the mediastinum.17,18,19,20,38,46,53 Their infiltrative nature and propensity for recurrence make lymphangiomas difficult to resect, and careful preoperative planning is critical to successful removal.38,46,53 Cystic hygromas are a localized form of lymphangioma, usually identified in early childhood, in which the lymphatic channels dilate in a multiloculated, cystic mass.38,46,53
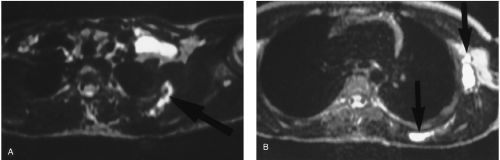 FIG. 34-6. A and B: Magnetic resonance image of chest wall lymphangioma. These infiltrative cystic lymph saccules demonstrate high signal intensity on T2-weighted images. (From ref. 20, with permission.) |
The plain-film findings of chest wall lymphangiomas are limited, and cross-sectional evaluation with CT or MRI, or both, is required for further delineation. Lymphangiomas appear as well-defined cystic masses on CT, with homogenous CT attenuation in the range of water.38,46,53 Intravenous contrast is very beneficial in helping to define the margins of lymphangiomas from surrounding soft tissues and muscles. MRI exquisitely displays the extent of chest wall lymphangiomas because the dilated, fluid-containing structures demonstrate high signal intensity on T2-weighted images.38,46,53 T2-weighted sequences with fat suppression and STIR sequences highlight the water content of lymphangiomas and are excellent for delineating the full extent of these lesions. Internal septations within lymphangiomas are frequently identified both on CT and MRI.17,18,19,20,38,46,53
Vessel-related Pathology
Extrapleural masses in the apex of the thoracic cage may be caused by aneurysms, false aneurysms, or perivascular hematomas of the subclavian artery or veins. These are frequently the result of complications of central line placements17,18,19,20,53 (Fig. 34-7). Blunt chest trauma may result in chest wall hematomas of considerable size. Even cardiopulmonary resuscitation may cause chest wall hematomas, particularly in patients with underlying bleeding dyscrasias. Chest wall veins become excessively dilated when they serve as collateral drainage pathways around an intrathoracic site of obstruction, such as an obstructed or thrombosed superior vena cava.
 FIG. 34-7. Postoperative chest wall hematoma around an axillary graft. High density within the fluid collection represents clotted blood. (From ref. 17, with permission.) |
Malignancies of Chest Wall Soft Tissues
Breast cancer is the most common neoplasm to arise in the soft tissues of the chest wall.52 Mammography is currently the mainstay of breast cancer screening; however, gadolinium-enhanced MRI has shown some promise as an adjunct to mammography for distinguishing types of breast masses and for identifying multifocal breast cancers. The ultimate role of MRI in evaluating breast cancer has yet to be established. CT is used extensively to stage more advanced breast cancers, and both CT and MRI have important roles in the evaluation of local chest wall recurrences.5,44,45,52 Less common soft-tissue tumors of the chest wall include soft-tissue sarcomas and desmoid tumors.
Chest Wall Masses That Arise in Ribs and Cause Rib Destruction
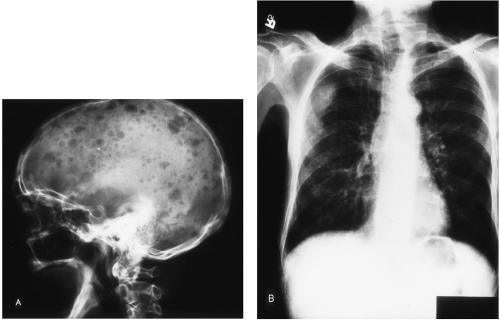
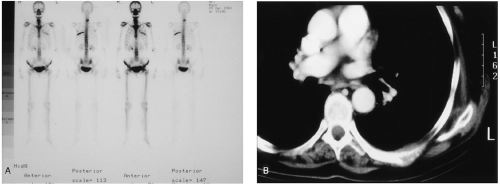
Chest wall masses that arise within a rib and cause rib destruction are often first detected on chest radiographs. In the adult, the most common causes of this finding are metastases or multiple myeloma41 (Figs. 34-8, 34-9, and 34-10). The same differential diagnosis is also true for masses arising in the sternum that cause bone destruction48A (Fig. 34-11). In adults, the ribs and sternum are skeletal locations with remaining red marrow, making them susceptible to hematogenous metastases from cancers of the breast, lung, kidney, and thyroid. 52 In the child, Ewing’s sarcoma and metastatic neuroblastoma are the most common cause of destructive rib masses.
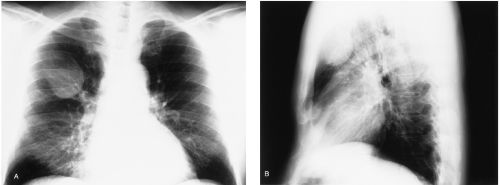
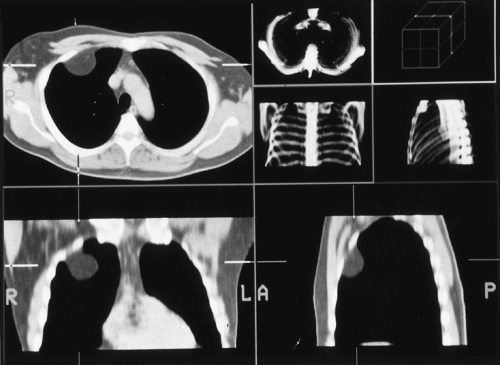
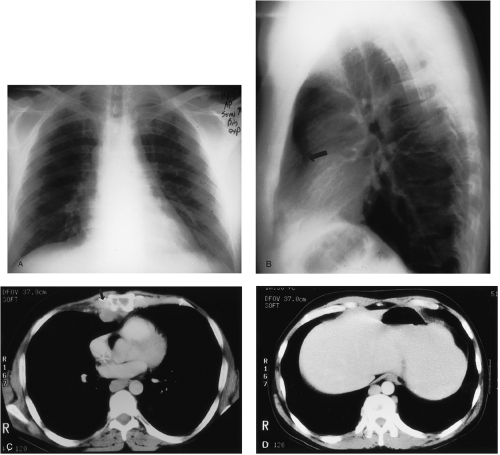
 FIG. 34-8. Multiple extrapulmonary chest wall masses with rib destruction caused by rib metastases from hepatoma. (From ref. 20, with permission.) |
A variety of primary malignant and benign tumors also arise in the bone or cartilage of ribs, but compared with metastases these are uncommon lesions. Such tumors include chondrosarcomas, osteosarcomas, fibrosarcomas, round cell tumors, giant cell tumors, osteochondromas, enchondromas, aneurysmal bone cysts, and hemangiomas.41,52 Non-neoplastic disorders also produce rib masses and rib destruction, as in conditions such as fibrous dysplasia, eosinophilic granuloma, radiation osteitis, brown tumors in hyperparathyroidism, or rib erosion caused by an expanding thoracic aneurysm41 (Figs. 34-12, 34-13, and 34-14). Healing rib fractures are a common cause of a palpable rib mass or a lesion mimicking a pulmonary nodule on plain films. In patients with chronic renal failure and secondary hyperparathyroidism, metastatic calcifications in the soft tissues of the chest wall can simulate pulmonary nodules or bone tumors. Examination beyond the chest radiograph usually requires CT and sometimes MRI. In general, cortical bone destruction is more accurately detected with CT, because of its better spatial resolution. Infiltration of the bone marrow and the soft-tissue extent of chest wall masses are more accurately displayed with MRI.
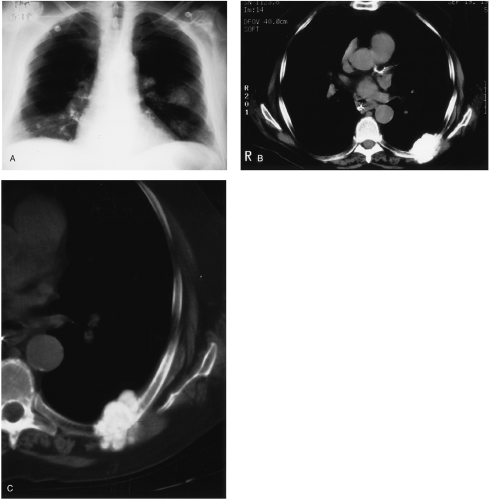
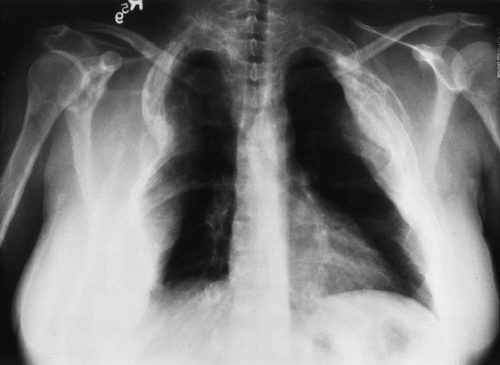 FIG. 34-14. Polyostotic fibrous dysplasia producing multiple chest wall masses as a result of expansile rib enlargement. (From ref. 20, with permission.) |
Chest Wall Invasion by Tumor
Lung Cancer and the Pancoast Syndrome
The Pancoast syndrome is a clinical triad of ipsilateral arm pain, wasting of the muscles of the hand, and Horner’s eye findings (exophthalmos, ptosis, miosis, and anhiydrosis). 9,10,27,32,34,52,56 It is caused by any tumor in the superior sulcus that invades the chest wall to involve the brachial plexus in the supraclavicular fossa and the sympathetic stellate ganglion in the upper mediastinum and lower neck.9,32,34,56
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree