Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
20.1.1 Anatomy (Fig. ) []
20.1.2 Histology (Fig. ) []
20.2.1 Metaplasia []
20.2.3 Salpingitis
20.2.5 Tubal Infertility
20.3.3 Leiomyoma and Adenomyoma
20.3.6 Teratoma
20.4.1 Carcinoma In Situ
20.4.2 Invasive Adenocarcinoma
20.4.4 Metastatic Tumors
20.4.5 Lymphomas
Abstract
The tube is situated in the upper part of the broad ligament.
20.1 Anatomy and Histology
20.1.1 Anatomy (Fig. 20.1) [1]
Fig. 20.1
(a) Ovary (1), Tube (2), Uterus (3), Mesosalpinx (4), Mesometrium (5). (b) Mesosalpinx (1), Mesovarium (2), Mesometrium (3). (c) Tube: Intramural (1), isthmus (2), ampulla (3), infundibulum, fimbriae (4), and ovarian fimbria (5) Ovarian ligament (6), Tuboovarian ligament (7), Lomboovarian ligament (8), Mesosalpinx (9), Mesometrium (10). (d) Mesonephric duct remnants (1) (From Testut [1])
20.1.1.1 Location
The tube is situated in the upper part of the broad ligament.
The broad ligament comprises:
The mesosalpinx
The mesovarium
The mesometrium
The mesosalpinx is a fold of peritoneum attached:
Above to the uterine tube
Below and posteriorly to the mesovarium
Laterally to the suspensory ligament of the ovary
Medially to the ovarian ligament
20.1.1.2 Description
The tube comprises four different parts from medial to lateral:
The intramural part (1 cm length): It lies within the wall of the uterus. It opens into the uterine cavity, near the cornu, through the uterine os.
The isthmus (2 cm length): It forms its medial third. Its lumen is narrow.
The ampulla (6 cm length).
The infundibulum (1 cm length): Its circumference is prolonged into a variable number of finger-like processes, the fimbriae. One of these, the ovarian fimbria, is longer than the others (2–3 cm). It goes from the posterior part of the infundibulum, follows the upper border of the tubo-ovarian ligament.
20.1.2 Histology (Fig. 20.2) [2]
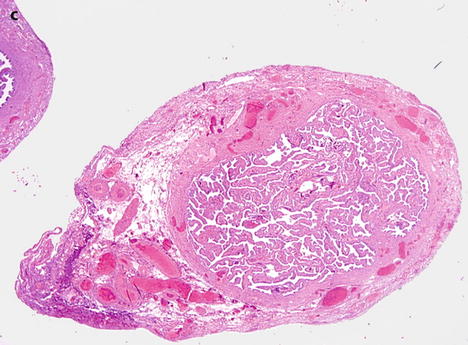
Fig. 20.2
(a) Longitudinal section of the tube showing: A thin proximal portion of the tube (intramural and isthmus), and a much larger distal part (ampulla and fimbriae). An increase of the number and height of the folds or plicae from the proximal part to the distal part. (b) Transverse section of the tube through the isthmus shows the three layers of the wall: (1) the mucosa with its epithelium and its lamina propria, (2) the muscularis with its thicker inner circular layer (thick black arrow) and its thinner outer longitudinal layer (gray arrow), (3) the serosa (thin black arrow). (c) Transverse section through the ampulla illustrates the significant increase of the number of plicae in this portion of the tube (Fig. 20.2a, b from Testut [1])
20.1.2.1 Mucosa
The mucosal layer consists of a luminal epithelial lining and a scanty lamina propria.
(a)
The epithelium is composed of:
Columnar secretory cells (55–65 %).
Ciliated cells (20–30 %).
Intercalary or peg cells: Columnar cells occupied by a thin dark staining nuclei.
Scattered lymphocytes may be seen located above the basement membrane.
(b)
The lamina propria contains spindly or angular cells and vessels.
The mucosa increases in its gross structural complexity as the lumen enlarges from the uterine to the ovarian end.
The interstitial and intramural portions each contain about five or six blunt plicae or folds. In the isthmus, the plicae increase in height to more nearly occupy the larger lumen. A dozen or more plicae, some with secondary folds, are present.
In the ampulla, the plicae are frond-like and delicate, and both secondary and tertiary branches are visualized.
20.1.2.2 Muscularis
The muscularis has two layers, mainly an inner circular layer that has a variable thickness, being about 0.5 mm in the isthmus and 0.1 mm in the ampulla, and an outer longitudinal layer.
At the uterine end, beginning in the intramural tube and extending laterally about 2 cm, there is in addition an inner longitudinal layer.
20.1.2.3 Serosa
The serosa is lined by flattened mesothelial cells. Beneath the mesothelium, there is a small amount of collagen and blood vessels.
20.2 Non-Tumoral Tubal Lesions
(a)
Metaplasia
(b)
Endometriosis (see Chap. 17.1.10) and endosalpingiosis (see Chap. 17.2.4)
(d)
Salpingitis isthmica nodosa
(e)
Tubal infertility
20.2.1 Metaplasia [2]
The metaplastic cells are squamous, transitional, or mucinous resembling the endocervical epithelium. Mucinous metaplasia may be associated with Peutz-Jeghers syndrome or chronic inflammation.
20.2.4 Salpingitis Isthmica Nodosa [2]
20.2.4.1 Definition
One or more outpouchings or diverticula of the epithelium, surrounded by nodular hyperplasia of the muscularis, are located in the isthmic portion of the tube (Table 20.1).
Table 20.1
Clinical and imaging findings in salpingitis isthmica nodosa
–30 years |
–Isthmic portion of the tube |
–Often bilateral |
–Nodules of 1–2 cm in diameter centered by a diverticulum |
–Serosa smooth |
–Complications: infertility, ectopic pregnancy, and exceptionally rupture |
20.2.4.2 Etiology
The etiology is unknown. Salpingitis or adenomyosis-like process has been suggested.
20.2.4.3 Clinical and Imaging Findings
They are reported in Table 20.1.
At hysterosalpingography, the pattern of diverticles of the isthmic portion is very characteristic (Fig. 20.3).
Get Clinical Tree app for offline access
Fig. 20.3
Hysterosalpingography (a) displays multiple diverticles on the isthmic portion of the right fallopian tube (arrow




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree