Diseases of the Joints
Lee F. Rogers
L. F. Rogers: Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, North Carolina 27157.
The ends of apposing bones, as portrayed on a roentgenogram, are separated by a space commonly referred to as the joint space. This space is occupied by articular cartilage and a small amount of synovial fluid, both of which have the same radiodensity and are therefore indistinguishable from each other. Loss of articular cartilage is manifested radiographically as a decrease in the width of the joint space. The joint capsule of the normal joint is of the same density as the surrounding soft tissue and is usually difficult to visualize. However, when the joint is distended by fluid, its outer limits may be seen if there is sufficient fat in the periarticular tissues to offer contrast (see Figs. 3-15, 3-16A, and 3-18). This is particularly true of the peripheral joints: the interphalangeal (IP) and metacarpophalangeal (MCP) joints of the hand, the ankle, the wrist, the elbow, and the suprapatellar bursa of the knee. However, it is difficult to identify distention of the major proximal joints—the shoulder, hip, and axial skeleton. Periarticular edema or hemorrhage tends to obliterate the fat and tissue planes. Close observation of periarticular soft tissues often permits the detection of early signs of inflammatory disease in the joint or adjacent structures.
Radiographs are used in diseases of the joints to confirm the clinical diagnosis of joint disease, determine the type of joint disease, and evaluate the extent of clinically known disease.9 The radiographic findings may be either consistent or inconsistent with the clinical diagnosis. If inconsistent, an alternative diagnosis should be made on the basis of the radiographic appearance of the disease process. On other occasions, joint disease is observed on a radiograph obtained for some other reason (e.g., peripheral trauma); on a chest radiograph demonstrating changes in the spine or pectoral girdle; or on radiographs of the abdomen and pelvis revealing abnormalities of the spine, sacroiliac joints, or hips. In these situations, the joint disease should be categorized and included in the radiographic report.
There are four principal radiographic signs of joint abnormalities or joint disease: (1) abnormalities of the apposing margins of both bones at a joint, (2) change in the width of the joint space (usually narrowing but occasionally widening because of an increase in synovial fluid), (3) malalignment of the joint (subluxation or dislocation with the joint margins no longer in apposition), and (4) periarticular swelling caused by distention of the joint capsule. The most common findings are narrowing of the joint space and abnormalities of the apposing articular margins of bone.
Each joint disease has a more or less specific pattern of radiographic abnormalities. This pattern is based on the radiographic characteristics at each individual joint, the distribution of joint involvement, and the presence or absence of other ancillary radiographic findings.13 When the characteristic pattern is coupled with the clinical history, physical findings, and laboratory examinations, the correct diagnosis can be established with reasonable certainty.
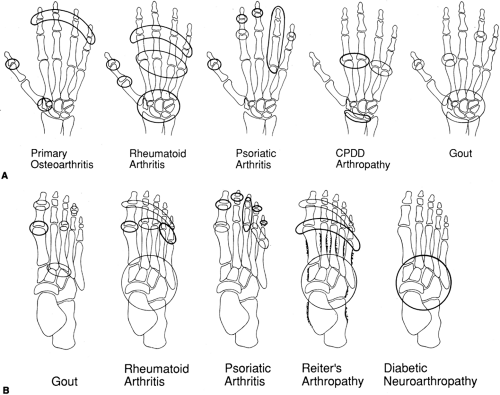
The distribution of joint involvement is extremely important. At the beginning of a diagnostic evaluation, it should be determined whether the process is limited to one joint (monoarticular) or involves multiple joints (polyarticular). Each joint disease has a characteristic distribution of joint involvement (Fig. 3-1); it is more likely to involve certain joints than others, and to involve those joints either symmetrically (simultaneous involvement of similar joints of both extremities) or asymmetrically (involvement of a joint on one side without simultaneous involvement of the corresponding joint on the opposite side).
The specific radiographic characteristics of importance in establishing or confirming the diagnosis often are the following: (1) whether the joint space narrowing is symmetrical or asymmetrical; (2) whether soft-tissue swelling is present and whether it is symmetrical (indicating a joint effusion) or asymmetrical (indicating a periarticular mass); and the presence or absence of (3) periarticular osteoporosis, (4) periarticular erosions, and (5) spur formation.
Ancillary radiographic findings include the presence or absence of periosteal reaction of bones in the vicinity of the
involved joint and the character of calcification or ossification of ligamentous attachments or tendinous attachments about the joint. Such calcifications and ossifications are referred to as entheses, and their diffuse presence in the skeletal system is known as an enthesopathy. Finally, the presence or absence of calcification within the joint cartilage (chondrocalcinosis) is to be noted. This finding is characteristic of certain joint disorders.
involved joint and the character of calcification or ossification of ligamentous attachments or tendinous attachments about the joint. Such calcifications and ossifications are referred to as entheses, and their diffuse presence in the skeletal system is known as an enthesopathy. Finally, the presence or absence of calcification within the joint cartilage (chondrocalcinosis) is to be noted. This finding is characteristic of certain joint disorders.
The clinical findings of importance are the age and sex of the patient, a history of previous trauma, the clinical appearance of the joint or joints involved, the presence or absence of associated diseases (particularly skin disease, uveitis, urethritis, and diarrhea), and identifiable tophaceous deposits. Laboratory values of importance are the erythrocyte sedimentation rate; the presence or absence of serum rheumatoid factor; the leukocyte count; and the serum levels of calcium, phosphorus, alkaline phosphatase, and uric acid. The radiographic diagnosis is aided greatly by knowledge of the clinical and laboratory findings, and the opposite is equally true: the radiographic diagnosis of joint disease may be severely handicapped in the absence of knowledge of the results of clinical and laboratory examinations.
Joint diseases are classified in Table 3-1.
INFECTIOUS ARTHRITIS
Acute and Chronic Pyogenic Arthritis of the Peripheral Joints
The source of infection resulting in pyogenic arthritis may be hematogenous, from other infections of the skin, respiratory tract, or urinary system; it may be a direct extension from a focus of adjacent osteomyelitis; or it may be a consequence of bacterial contamination resulting from surgical procedures or open injuries of the joint. The course of the disease varies considerably. In some cases, it is relatively
mild and subsides without residua. In others, a purulent infection ensues, causing pyoarthrosis with rapid destruction of joint surfaces. In still others, the disease follows a comparatively indolent and chronic course from the outset.
mild and subsides without residua. In others, a purulent infection ensues, causing pyoarthrosis with rapid destruction of joint surfaces. In still others, the disease follows a comparatively indolent and chronic course from the outset.
In children, infection more commonly involves the major peripheral joints, and the source of infection is very likely to be an infection of the skin, upper respiratory tract, or lungs. In adults, the source is more likely to be trauma or surgery secondary to vascular disease, particularly in the feet of diabetic patients. Bacterial spondylitis is more common in adults than in children; it is often associated with a urinary tract infection or occurs after catheterization or other manipulative procedures of the bladder and urethra.
Unusual sites of pyogenic infection occur in intravenous drug abusers, including the sternoclavicular and sacroiliac joints, and infections are often caused by gram-negative organisms. Septic arthritis may also complicate intra-articular injection of steroids.
Roentgenographic Observations
The radiographic findings described here occur in an untreated or inadequately treated infection of virulence.13 With present-day therapeutic measures, most cases of acute pyogenic joint infection can be brought under control before appreciable damage occurs within the joint.
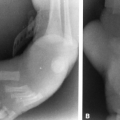
Soft-Tissue Swelling
In the first few days of infection, the only roentgenographic changes are those of soft-tissue swelling and distention of the joint capsule by fluid (Fig. 3-2). This causes an increase in soft-tissue density about the joint (Fig. 3-3). Periarticular edema tends to obliterate the tissue planes around the joint and often extends into the subcutaneous fat. In the absence of trauma, such findings, particularly in a febrile child with pain or tenderness in the area, strongly suggest the diagnosis of septic arthritis. Soft-tissue changes of this type are not specific, of course, and at this stage of the disease needle aspiration should be performed promptly to establish the diagnosis or rule out the possibility of infectious arthritis. The diagnosis of infectious arthritis should not await the appearance of radiographic changes.
Joint-Space Narrowing
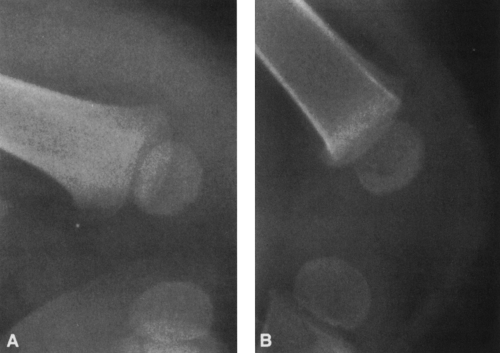
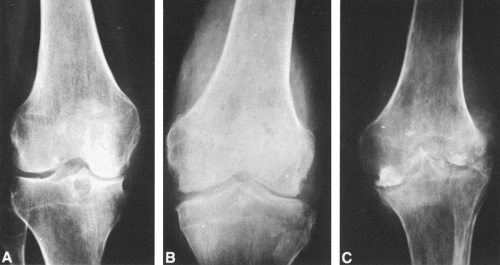
Purulent organisms excrete proteolytic enzymes that destroy articular cartilage (Fig. 3-4), resulting in a decrease in the width of the joint space. In a virulent infection, this may become evident 7 to 10 days after the onset of disease. If the infection is untreated or inadequately treated, the narrowing progresses rapidly and the joint space may disappear completely within several weeks. Early in the course of acute infection, the bones about the joint maintain normal density; however, if the infection becomes subacute or chronic, osteoporosis becomes evident. Joint narrowing and destruction in the absence of osteoporosis are indicative of a highly virulent infection.
Bone Destruction
Bone destruction is manifested by irregularity of the subchondral bone at the apposing margins of the joint (see Figs. 3-3 and 3-4B).
The destruction may be focal initially, but it eventually extends across the entire joint surface. Because bone destruction does not occur for 8 to 10 days, this sign is of no value in the early diagnosis of joint infection.
The destruction may be focal initially, but it eventually extends across the entire joint surface. Because bone destruction does not occur for 8 to 10 days, this sign is of no value in the early diagnosis of joint infection.
Ankylosis
If the articular cartilages are completely destroyed, bony ankylosis usually follows. Eventually, bone trabeculae form across the ends of the bones, and in time all evidence of the joint may disappear.
If antibiotic treatment is ineffective or is discontinued too soon, the acute infection may be transformed into a chronic indolent process with a slowly progressive course extending over months. In this case, there is a gradual decrease in the joint space, the articular ends of the bone become roughened, and sequestra may form. As the infection subsides, the bones gradually regain density and bony ankylosis may occur. If the infection continues, fibrous or bony ankylosis may occur, resulting in little or no joint motion (Fig. 3-4C).
Neonatal Infections
Septic arthritis frequently occurs as a complication of neonatal osteomyelitis. Such infections occur in premature and full-term infants who have undergone catheterization of umbilical vessels. In the neonate, the blood supply of the epiphysis is contiguous with that of the metaphysis, and extension of an infectious process into the joint is therefore very likely (Fig. 3-5). Multiple sites of infection are the rule, and septic arthritis is common. The hip is involved in 45% of cases, the knee in 35%; remaining sites are the shoulder, elbow, and ankle. If the hip is involved, the joint distention may be sufficient to result in a dislocation accompanied by a large surrounding soft-tissue mass (Fig. 3-6).
Neonatal osteomyelitis also may occur in those who have not had umbilical catheterization. Under these circumstances, the signs are often vague and there is only a single focus of disease.
TUBERCULOSIS OF THE PERIPHERAL JOINTS
Tuberculosis of the joints is a chronic indolent infection having an insidious onset and a slowly progressive course. It usually affects a single joint (monoarticular). The joint disease may result from hematogenous dissemination to the synovial membrane, or it may be secondary to a tuberculous abscess in the neighboring bone. The latter is common in childhood. Pathologically, tuberculosis usually begins as a synovitis. Proliferation of inflammatory granulation tissue, known as pannus, begins at the perichondrium and spreads over the joint surfaces. It interferes with nutrition of the
cartilage, resulting in degeneration and destruction. In weight-bearing joints, and to a lesser degree in non-weight-bearing joints, there is a tendency for preservation of the joint cartilages at sites of maximum weight-bearing or close apposition of cartilage. This is in contrast to pyogenic infections, in which the joint exudate contains proteolytic enzymes that rapidly destroy the entire cartilaginous joint surface.
cartilage, resulting in degeneration and destruction. In weight-bearing joints, and to a lesser degree in non-weight-bearing joints, there is a tendency for preservation of the joint cartilages at sites of maximum weight-bearing or close apposition of cartilage. This is in contrast to pyogenic infections, in which the joint exudate contains proteolytic enzymes that rapidly destroy the entire cartilaginous joint surface.
Roentgenographic Observations
Tuberculous Arthritis
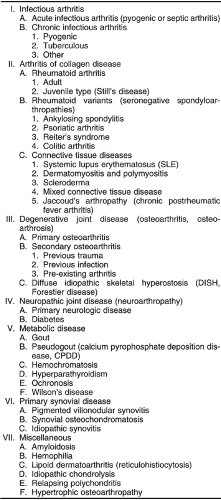
The earliest evidence of tuberculous arthritis of a peripheral joint is a joint effusion. In time, often after several months, the bones adjacent to the joint become osteoporotic. The osteoporosis is often severe and probably is caused by a combination of hyperemia and disuse (Fig. 3-7). Eventually, destruction of articular cartilage is manifested by narrowing of the joint and erosion of bone. In the weight-bearing joints, there is a tendency for preservation of cartilage at the point of maximum weight-bearing (Fig. 3-8). The earliest evidence of bone destruction is the appearance of erosions at the margins of the joint. These marginal defects are sharply circumscribed and closely resemble erosions seen in rheumatoid arthritis. Marginal erosions gradually extend across the joint surface. With further progression, gross disorganization of the joint may occur. The articular cartilage disappears, ragged destruction of the articular ends of the bone occurs, and separation of dead fragments (sequestra) is noted (Fig. 3-8C). Very little reactive sclerosis is observed in untreated tuberculosis.
Caries sicca is a relatively uncommon form of tuberculosis that is characterized by a chronic and indolent course and an absence of joint effusion. Except for the lack of fluid and associated swelling of soft tissues, the roentgenographic findings in this type of disease differ little from those described previously. This type occurs most frequently in the shoulder.
Unilateral abnormalities of the sacroiliac joint should suggest the possibility of tuberculosis. Bacterial infections of
this joint are also encountered in drug abusers. The radiographic findings are destruction of the joint margins with some degree of reactive sclerosis.
this joint are also encountered in drug abusers. The radiographic findings are destruction of the joint margins with some degree of reactive sclerosis.
In tuberculosis there is little tendency for spontaneous healing, and bony ankylosis seldom develops without surgical intervention.
The differential diagnosis of tuberculous arthritis includes principally acute and chronic pyogenic arthritis and rheumatoid arthritis. In acute pyogenic arthritis, there is early destruction of joint space and an absence of osteoporosis. In chronic pyogenic arthritis, the findings are very similar. Bony ankylosis is much more likely in a pyogenic infection than in tuberculosis. In a given joint, the differentiation between tuberculosis and rheumatoid arthritis may be difficult. However, the polyarticular nature and distribution of rheumatoid arthritis should distinguish it from tuberculosis, which is almost always monoarticular.
Fungal Infections
Joint involvement is rare in fungal infections. However, blastomycosis, histoplasmosis, actinomycosis, coccidioidomycosis, and cryptococcosis joint infections are occasionally observed. They are similar in appearance to tuberculosis. Diagnosis must be based on recovery of the causative organism.
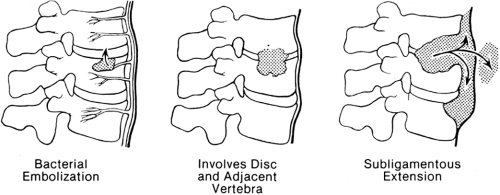
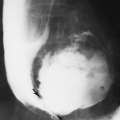
INFECTIOUS SPONDYLITIS
Infections of the spine are initiated by hematogenous spread of organisms. These may be of arterial or paravertebral venous plexus origin. The latter is very likely to be the source of infections of the spine that are associated with infections of the urinary tract or occur after urinary tract manipulations. The bacteria lodge beneath the end-plate of a vertebra, usually anteriorly, and quickly extend into the adjacent intervertebral disc and then into the inferior end-plate of the adjacent vertebral body (Fig. 3-9).13 From here, the infection may extend out of the vertebra and along the spine, beneath the paravertebral ligament, forming soft-tissue masses and abscesses.
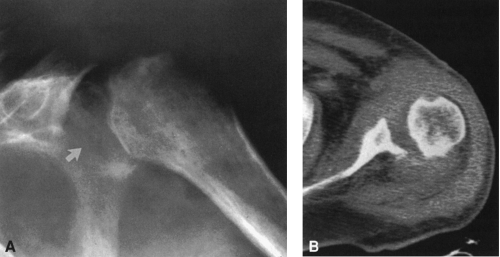
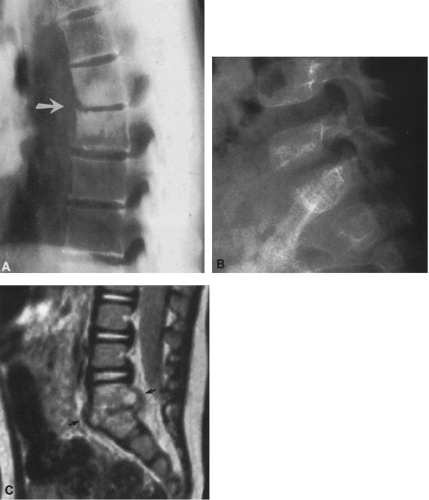
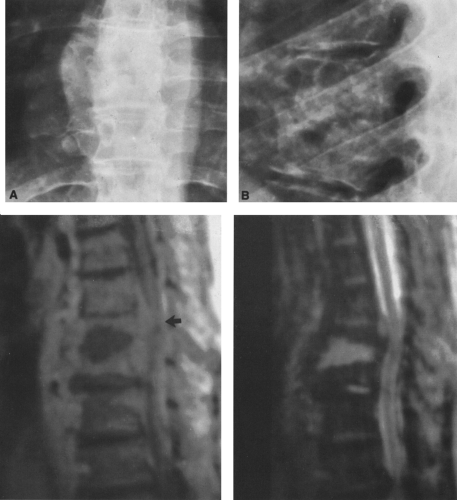
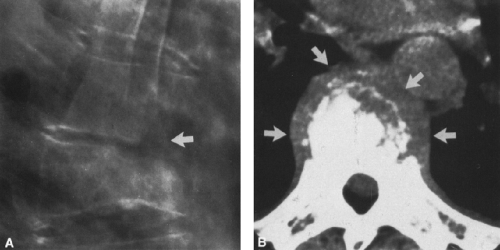
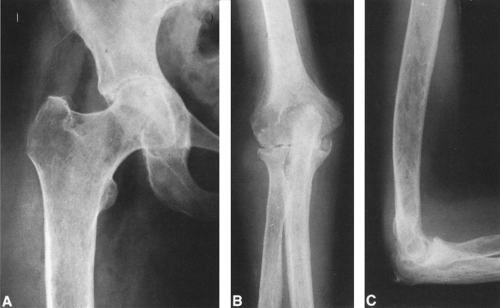
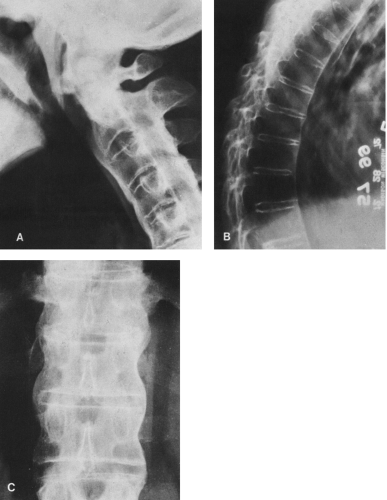
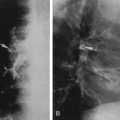
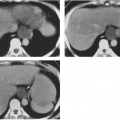
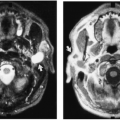
The radiographic findings indicative of infectious spondylitis are (1) narrowing of the disc space, (2) erosion and destruction of adjacent vertebral end-plates, and (3) a paravertebral soft-tissue mass (Figs. 3-10 and 3-11). In the cervical spine, the soft-tissue mass is identified on the lateral radiograph as an enlargement of the retropharyngeal soft tissues and, in the thoracic spine, it is a paravertebral soft-tissue mass that is best seen on the anteroposterior radiograph of the chest or thoracic spine (Fig. 3-11A). The soft-tissue mass associated with infection of the lumbar vertebral bodies is usually very difficult to see on the anteroposterior radiographs of the lumbar spine. In all locations, both the paraspinous soft-tissue mass and the degree of vertebral body destruction are readily identified by computed tomography (CT) (Fig. 3-12). In questionable cases, polytomography is the best method of evaluation because it clearly demonstrates the end-plates of the adjacent vertebral bodies. Magnetic resonance imaging (MRI) demonstrates all of the findings quite satisfactorily, including any encroachment upon or compression of the spinal cord (Figs. 3-10 and 3-11). Rarely, an infectious process is limited to the vertebral body or posterior bony elements and appears as a focus of destruction. In general, the posterior elements are not involved by the infectious process.
Pyogenic Spondylitis
Infectious spondylitis caused by pyogenic organisms has a tendency to be confined to one interspace, and the paraspinous soft-tissue masses are not as large as those seen with tuberculosis (see Figs. 3-11 and 3-12). The earliest roentgenographic sign is a decrease in the height of the disc space. CT or polytomography may be necessary to confirm destruction of the adjacent end-plates. The infections tend to be subacute, and the destructive focus often has a sclerotic margin.
Juvenile Spondyloarthritis
Calcification of one or more intervertebral discs in childhood is a rare disorder. Afflicted children are usually between
2 and 11 years old, with a predominance of boys. Patients usually complain of pain, with limitation of motion, muscle spasm, tenderness, and torticollis. Roentgenograms show calcification in one or more intervertebral discs, usually in the cervical area. The disease tends to be self-limited, and the calcifications gradually disappear over a period of several months. Although this condition has been regarded as an infection by some observers, there is evidence to indicate that some cases are of traumatic origin. Calcification of the disc in adult patients is usually found in the thoracic spine; it is a common condition and appears to be a degenerative change related to the aging process.
2 and 11 years old, with a predominance of boys. Patients usually complain of pain, with limitation of motion, muscle spasm, tenderness, and torticollis. Roentgenograms show calcification in one or more intervertebral discs, usually in the cervical area. The disease tends to be self-limited, and the calcifications gradually disappear over a period of several months. Although this condition has been regarded as an infection by some observers, there is evidence to indicate that some cases are of traumatic origin. Calcification of the disc in adult patients is usually found in the thoracic spine; it is a common condition and appears to be a degenerative change related to the aging process.
Tuberculous Spondylitis
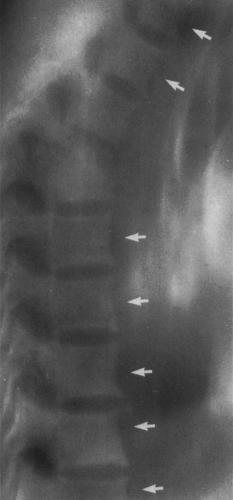
Tuberculous spondylitis has a greater tendency than infectious spondylitis to spread along the spine (Fig. 3-13; see Fig. 3-11). The spread occurs beneath the paraspinous ligaments, both above and below the initial site of infection. This spread forms an elongated paravertebral soft-tissue mass. Radiographically, the soft-tissue mass may be accompanied by irregular erosions or smooth, saucerized defects or scalloping of the anterior borders of several adjacent vertebral bodies. On other occasions, there is minimal radiographic evidence of disc disease but extensive paravertebral soft-tissue masses are present, there is little or no vertebral collapse, and the intervertebral discs appear to be preserved. In long-standing cases, calcification may occur in the paravertebral abscesses. These calcified or partially calcified abscesses remain throughout life. With quiescence and healing of the disease, the bones regain a more normal density and bony ankylosis may occur across the involved disc. In very old cases of tuberculous spondylitis, several contiguous vertebrae may have been destroyed to such an extent that their individual outlines are no longer recognizable and all evidence of the intervening disc spaces has disappeared. The resultant angled deformity of the spine is known as a gibbus, from the Latin word for “hump.”
Fungal Spondylitis
Involvement of the spine occasionally occurs in actinomycosis, blastomycosis, and coccidioidomycosis. Most lesions resemble those of tuberculosis. Coccidioidomycosis has a tendency to involve bony protuberances and may present as isolated destructive foci in the posterior elements.
RHEUMATOID ARTHRITIS
Rheumatoid arthritis affects adults between the ages of 20 and 60 years, with the highest incidence between the ages of 40 and 50 years. Females are affected much more frequently than males. The clinical course of the disease varies. In most cases, it begins insidiously and then either runs a protracted and progressive course or undergoes remissions of variable length. Usually, the disease eventually leads to a variable degree of deformity of the affected joints. In the typical case, the disease begins in the peripheral joints, usually the proximal interphalangeal (PIP) and MCP joints
of the hand and the carpal joints of the wrist. There is a tendency for symmetrical involvement of the joints on the right and left sides; this tendency is stronger in women than men. As the disease progresses, it affects more proximal joints, advancing toward the trunk in all extremities until finally almost every joint in the body is involved. The disease may become arrested at any stage.
of the hand and the carpal joints of the wrist. There is a tendency for symmetrical involvement of the joints on the right and left sides; this tendency is stronger in women than men. As the disease progresses, it affects more proximal joints, advancing toward the trunk in all extremities until finally almost every joint in the body is involved. The disease may become arrested at any stage.
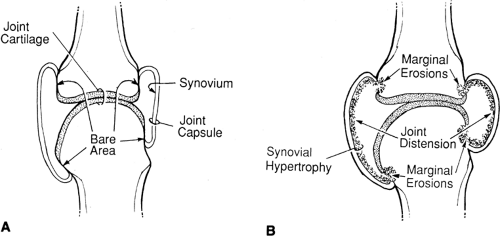
Pathologically, rheumatoid arthritis begins as synovitis. In the early stages there is edema and inflammation of the synovium and the subsynovial tissues. Joint effusion accompanies the synovial changes. If the disease advances, the synovium becomes greatly thickened, with enlargement of the synovial villi. This is followed by proliferation of fibrovascular connective tissue known as pannus. Pannus is responsible for the characteristic marginal erosions that first occur in the so-called bare areas between the peripheral edge of the joint cartilage and the insertion of the joint capsule (Fig. 3-14). Ultimately, pannus grows over the surface of the articular cartilage, interfering with normal nutrition, which results in cartilage degeneration, and destroying foci of underlying articular bone. In advanced cases the joint becomes filled with pannus, articular cartilage disappears, and fibrous ankylosis results, frequently followed by bony ankylosis. As these changes are occurring in the joint, the adjacent bone undergoes osteoporosis and muscles atrophy from disuse.
Roentgenographic Observations
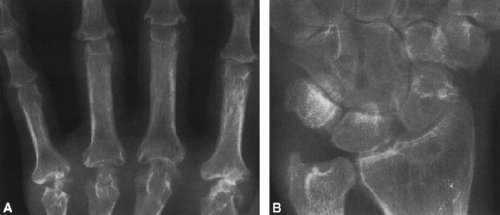
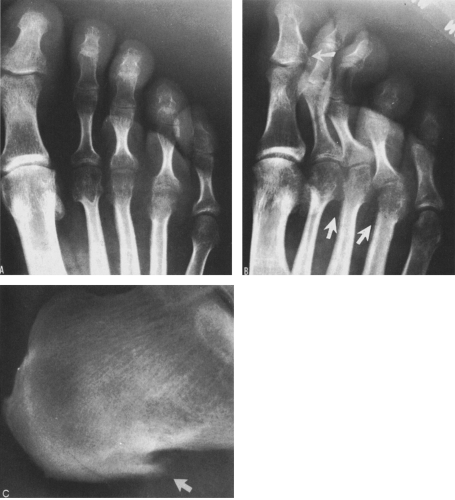
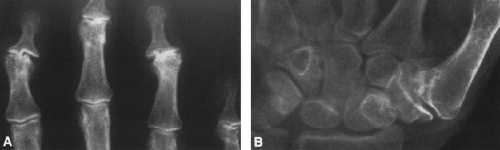
Radiographic findings vary with each stage of the disease. The initial manifestations are soft-tissue swelling, symmetrical narrowing of the joints, periarticular osteoporosis, and marginal erosions (Fig. 3-15). Radiographic manifestations of the disease are present in 66% of patients 3 to 6 months after the onset of disease and in 85% of those affected for 1 year. The distribution of joint involvement is characteristic. The disease begins in the PIP, MCP, and carpal joints (see Fig. 3-1A) with a more or less symmetrical distribution in the right and left extremities. In some cases the joints of the hand and wrist are equally affected, but in others the destructive process may be much more severe in the hand than in the carpus (Fig. 3-16). In still others, it may be more severe in the carpus than in the hand, even extensive in the carpus and yet minimal in the MCP and IP joints (Fig. 3-17). In the foot (see Fig. 3-1B), the metatarsophalangeal (MTP) joints, particularly the fourth and fifth, are often involved in the initial stage of the disease process. In fact, characteristic
changes of erosion may be present in the heads of the fourth or fifth metatarsal when the radiographic changes of the hand are minimal or nondiagnostic (Fig. 3-18). Therefore, it is important to examine not only the hands but also the feet in the initial evaluation of a patient with rheumatoid arthritis.
changes of erosion may be present in the heads of the fourth or fifth metatarsal when the radiographic changes of the hand are minimal or nondiagnostic (Fig. 3-18). Therefore, it is important to examine not only the hands but also the feet in the initial evaluation of a patient with rheumatoid arthritis.
Soft-Tissue Swelling
The earliest roentgenographic evidence of the disease is periarticular soft-tissue swelling, which characteristically is symmetrical and fusiform (see Fig. 3-15). This swelling is easily identified in the PIP joints and to a lesser extent in the MCP and MTP joints. Joint distention can also be identified in the knee, ankle, and wrist. The joint effusion is caused by the synovitis.
Periarticular Osteoporosis
Local demineralization of bone occurs adjacent to the involved joint. In the metacarpals and phalanges, this involves the base and heads of the bone but spares the diaphysis (see Fig. 3-15). In the wrist, all the carpal bones are involved, as are the distal margins of the radius and ulna and the bases of the metacarpals. The bones in the affected area are more radiolucent because of loss of bone mineral. In early cases, this finding is often rather striking because of the symmetry of the process.
In advanced disease, generalized osteoporosis develops, involving all portions of the skeleton. This is caused in part by the disease process and in part by disuse and may be compounded by the use of steroids.
Symmetrical Joint Space Narrowing
Narrowing of the joint space results from degeneration of the articular cartilages as pannus spreads across the joint surfaces (see Fig. 3-15). Typically this diminution in the joint is uniform and the joint space is symmetrically narrowed, in contrast to the asymmetrical narrowing that is characteristic of osteoarthritis. The narrowing may progress gradually until the ends of the bones practically impinge on one another.
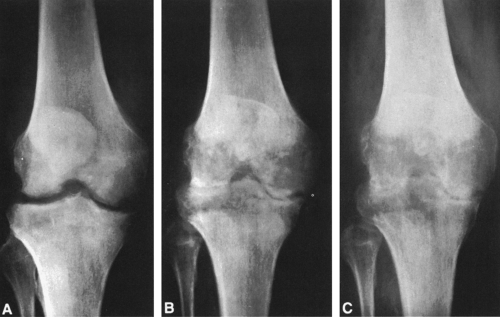
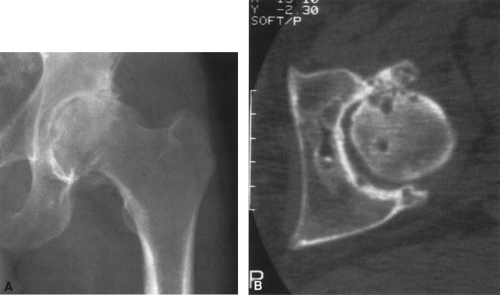
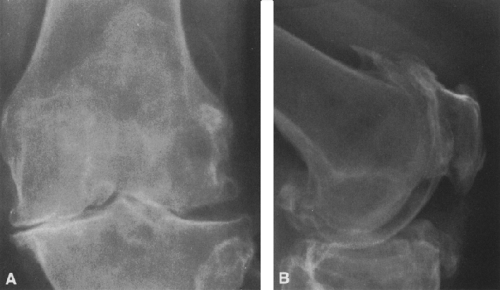
In the hip, thinning of the central aspect of the joint space causes displacement of the femoral head in an axial direction—that is, it moves upward and inward (Fig. 3-19). The joint space characteristically is symmetrically narrowed. The acetabulum may become deepened, eventually leading to characteristic changes of protrusio acetabuli (Otto pelvis) (Fig. 3-19). Rheumatoid arthritis of the knee characteristically involves all compartments–medial, lateral, and patellofemoral. When the knee is involved, there is an even or symmetrical narrowing of the joint space in all compartments, particularly medial and lateral.
Joint-space narrowing also occurs in osteoarthritis, but it differs in some ways (see Figs. 3-34, 3-35, and 3-36). In osteoarthritis the joint-space narrowing is characteristically asymmetrical. In the hip the narrowing is more marked superiorly, and in the knee it commonly is limited to the medial compartment. These and other findings such as the absence of osteoporosis and the presence of subchondral sclerosis of bone, subchondral cyst, and marginal spur formation should facilitate the differentiation between rheumatoid arthritis and osteoarthritis.
 FIG. 3-22. Juvenile rheumatoid arthritis. The lateral radiograph of the knee demonstrates soft-tissue swelling with joint effusion without evidence of bone destruction (compare with Fig. 3-2). At this stage, the correct diagnosis is dependent on joint aspiration. |
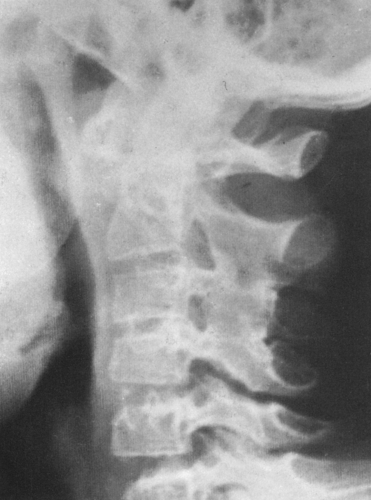 FIG. 3-24. Still’s disease of the cervical spine. Note the ankylosing of the apophyseal joints at C2-C3 and C3-C4. |
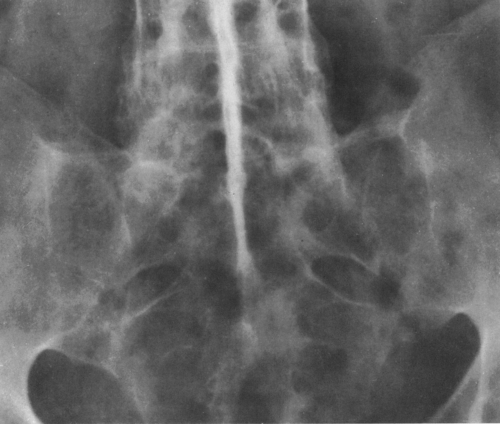 FIG. 3-25. Ankylosing spondylitis. There is complete bony ankylosis of the sacroiliac joints and calcification and ossification of the interspinous ligaments in the lower lumbar spine. |
 FIG. 3-29. Psoriatic arthritis. There is a mutilating destruction of the metatarsophalangeal joints and ankylosis of the proximal interphalangeal joints. |
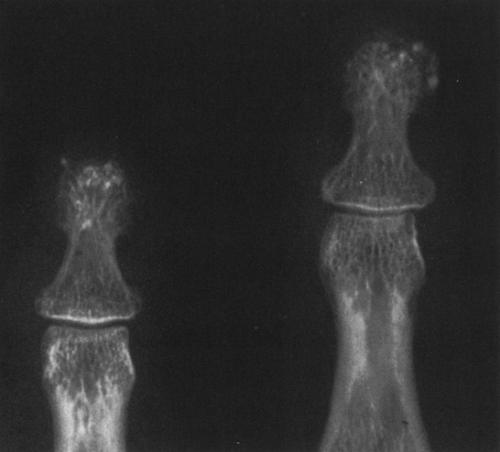 FIG. 3-33. Scleroderma. There is minimal tapering of the distal soft tissues and punctate soft-tissue calcifications, changes characteristic of scleroderma. |
Marginal Erosions
After a variable interval, bony erosions occur as a result of the development of granulation tissue (pannus) at the peripheral margin of the joint cartilage (see Figs. 3-15, 3-16, 3-17, and 3-18




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree