Fig. 18.1
(a, b) PA and axillary plain radiographs demonstrate arthritis of the acromioclavicular joint with narrowing of the joint space, osteophyte formation on both the acromion and distal clavicle, sclerosis and subchondral cystic change
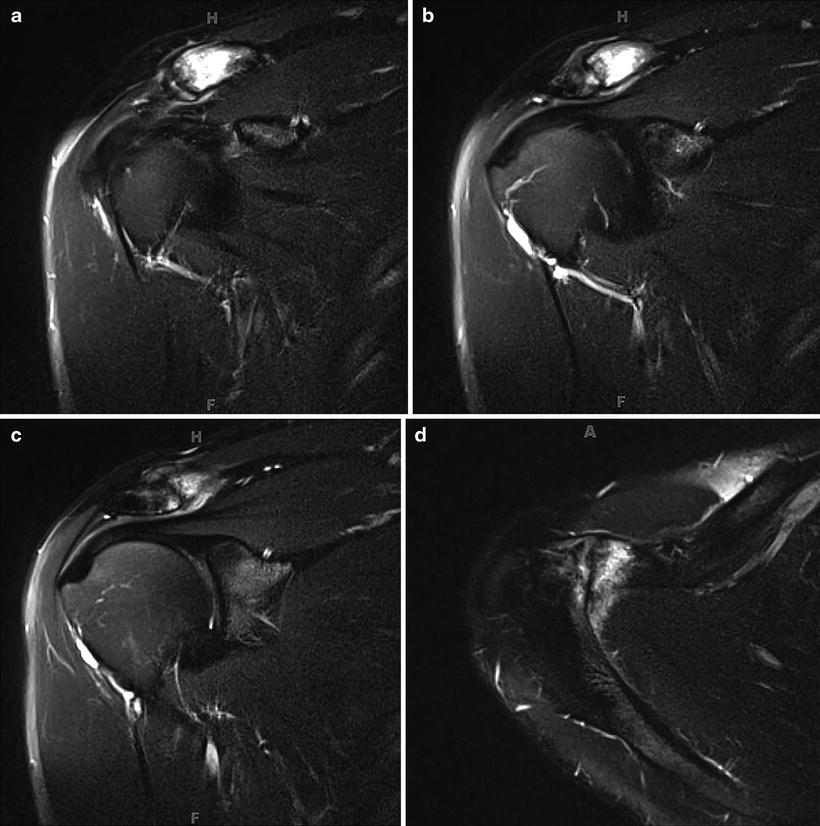
Fig. 18.2
a–c show a series of coronal MRI images, and d shows an axillary MRI image. These T2 MRI slices show edema in the distal clavicle and acromion as well as confirm degenerative changes seen on plain radiographs
The findings of AC joint arthritis on plain radiographs and MRI were consistent with the patient’s clinical presentation, with symptoms suggesting AC joint pathology and pain relived with AC joint injection. No other structures had pathology identified on the MRI. Specifically, the rotator cuff, biceps tendon, labrum, and articular cartilage of the glenohumeral joint were all intact. At this point, conservative management had not adequately controlled his symptoms, and the risks and benefits of operative intervention were discussed with the patient. He elected to proceed with arthroscopic distal clavicle excision.
Arthroscopy
Anesthesia was interscalene block plus local infiltration.
The patient was placed into the beach chair position. Arthroscopy was limited to only the AC joint, as no other shoulder pathology was suspected.
The plane of the AC joint was identified using a 1.5 inch 22-guage needle. A posterior viewing portal was then made directly posterior to the AC joint and a size 2.7 mm arthroscope was inserted into the AC joint. An anterior portal was then made and a 4.0 mm shaver was introduced into the AC joint.
There was a significant amount of degenerated intra-articular meniscus, which was debrided with a shaver and an ablator. A burr was then used to remove bone from the lateral end of the clavicle until there was a 1 cm gap between the remaining clavicle and the acromion. In this case, approximately 8 mm of bone from the distal clavicle was resected to achieve a 1 cm gap between the remaining bone ends.
Arthroscopic findings correlated well with the findings on X-ray and MRI: AC joint arthritis.
Discussion
Radiographic changes of AC joint arthritis are a common finding and frequently deemed incidental when the patient does not have clinical evidence of symptoms attributable to the AC joint. When AC joint arthritis is symptomatic, this is frequently confirmed with plain radiographs, and an MRI may not be needed.
AC joint arthritis may be addressed with arthroscopic distal clavicle excision. This may be done through an isolated arthroscopy of the AC joint, as in the case above, or as a component of a subacromial arthroscopy. postoperative PA and axillary plain radiographs are shown in Fig. 18.3a, b, and the arthroscopy images are shown in Fig. 18.4a–e.
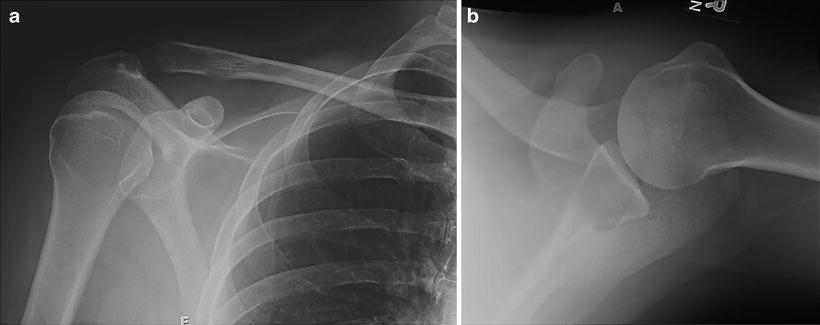
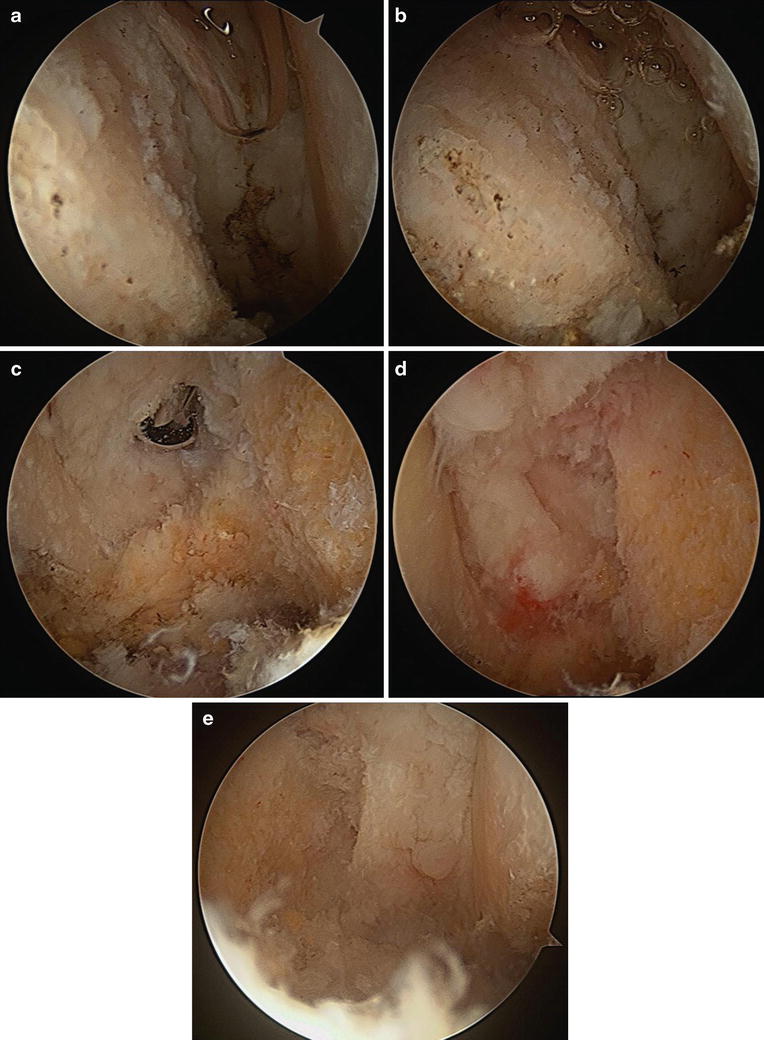
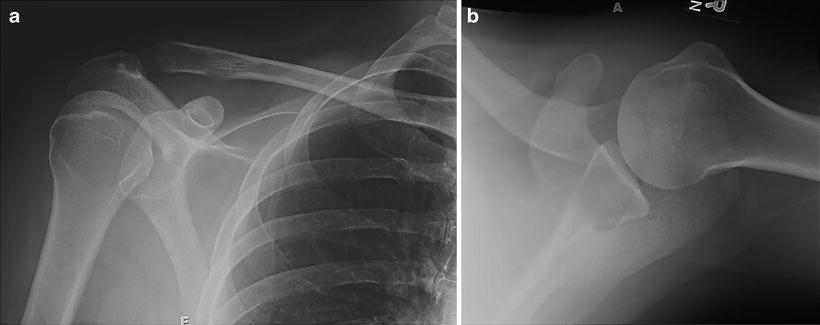
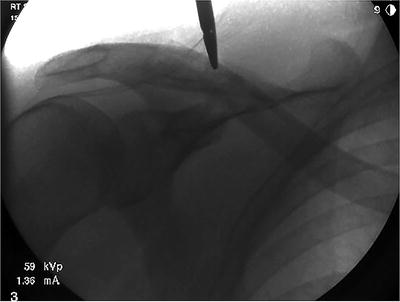
Fig. 18.3
(a, b) Postoperative PA and axillary radiographs demonstrate increased distance between the acromion and distal clavicle
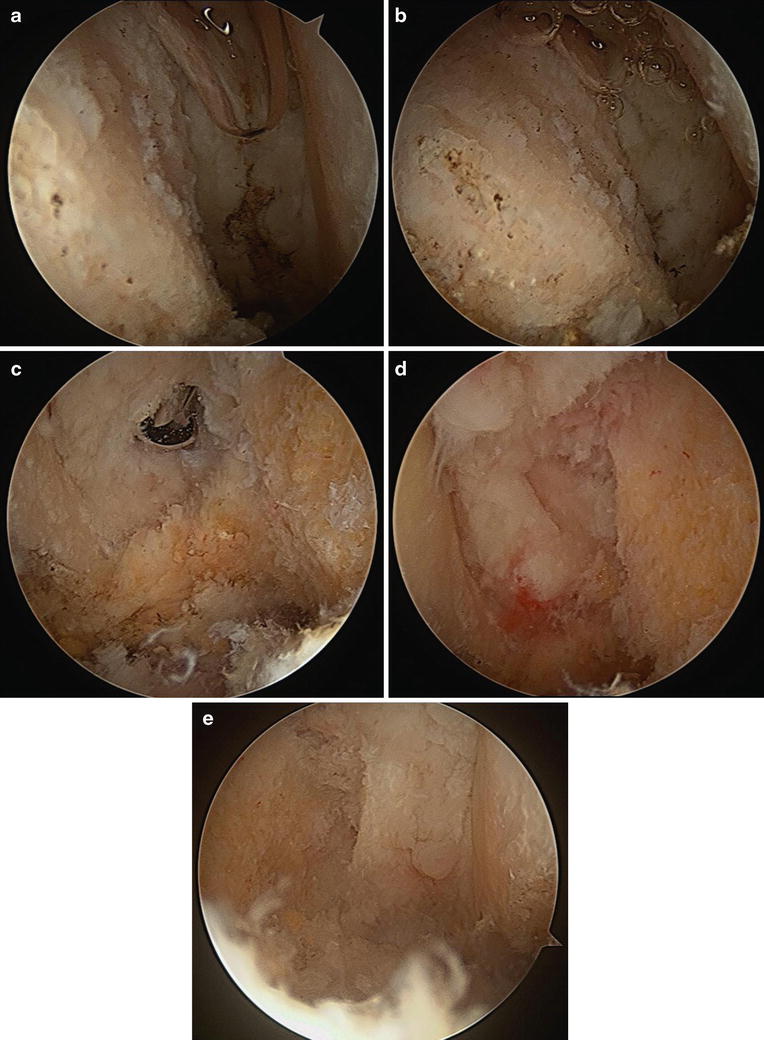
Fig. 18.4
(a–e) Images from the arthroscopy. a and b show the arthritic acromioclavicular joint from the posterior portal prior to any resection. c is viewed from the anterior portal, and a shaver is seen entering the AC joint from the posterior portal. d and e show the space created in the AC joint after the distal clavicle is resected; d is viewed from the anterior portal and e from the posterior portal
Case 2: AC Joint Separation
History/Exam
A 25-year-old man presented to the orthopedic clinic 2 months after a fall directly onto his right shoulder. He had gone to an urgent care on the day of his injury and was diagnosed with a type III AC separation. Subsequently, he wore a sling intermittently and was seen by an orthopedist and a physical therapist. Two months later, he presented to our clinic with continued pain localized to his right AC joint. Symptoms were exacerbated by certain arm motions, such as elevating his arm above his head, lifting items with this arm, and rolling onto this shoulder while sleeping.
On physical examination, the patient had a prominence over the AC joint consistent with type V AC separation. Additionally, he was tender to palpation over the AC joint. His shoulder range of motion was full and equal to the contralateral side. He was neurovascularly intact in the extremity and without symptoms in his contralateral shoulder. The remainder of his exam was unremarkable.
Imaging
Three views of the right shoulder were taken at the urgent care facility including a PA, a scapular Y, and an axillary X-ray (Fig. 18.5a–c). They demonstrate inferior displacement of the acromion relative to the distal clavicle; the coracoclavicular distance has increased greater than 100 %. The glenohumeral joint is located. The radiographic impression is a type V AC separation.
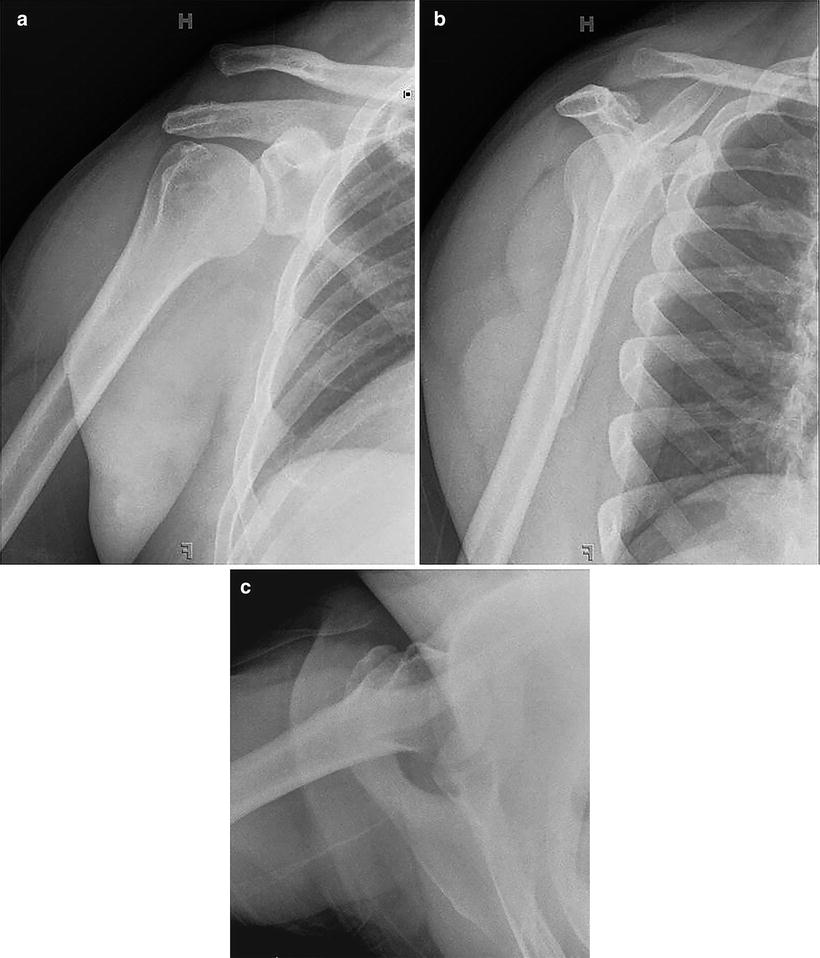
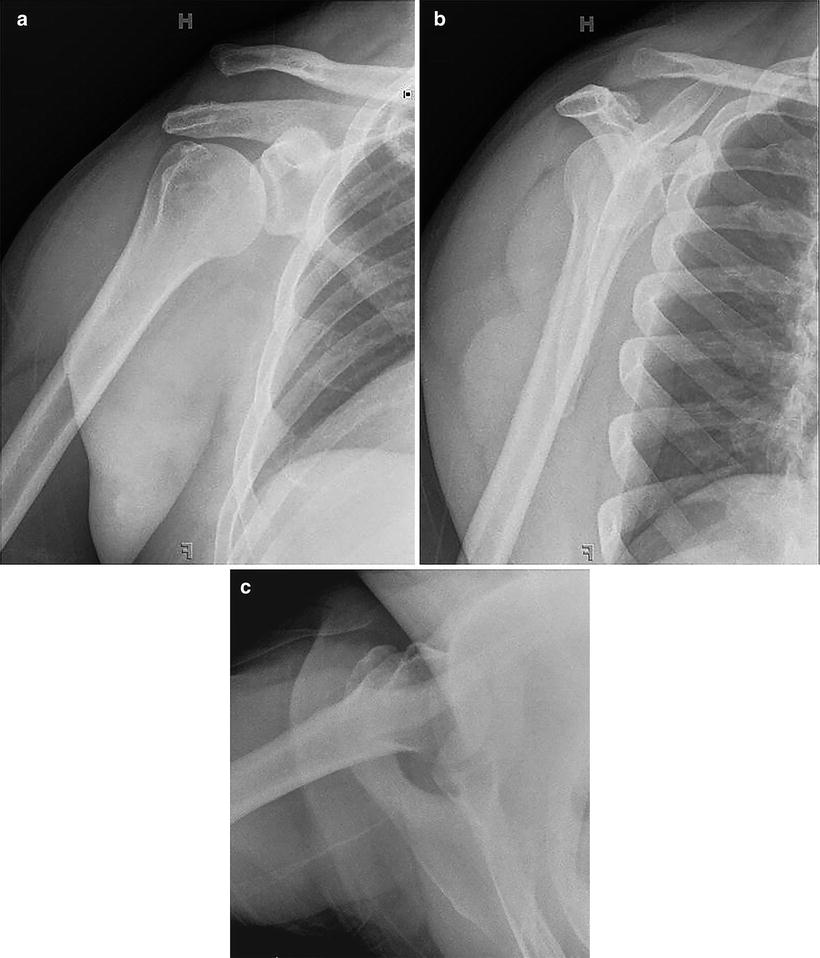
Fig. 18.5
a–c demonstrate PA, scapular Y, and axillary plain radiographs of a right shoulder with a type V AC separation
The findings of AC joint separation on plain radiographs were consistent with the patient’s clinical presentation. At this point, continued conservative management was recommended. It was discussed with the patient that many people with this injury do not require surgery. We discussed the high success rate of nonoperative treatment and that delayed reconstruction was no less successful than acute repair.
One month later, he returned to the clinic, noting no improvement in his symptoms. At this time, the risks and benefits of operative intervention were discussed with the patient. He elected to proceed with arthroscopically assisted coracoclavicular ligament reconstruction.
Arthroscopy
Anesthesia was an interscalene nerve block. The patient was placed into a well-padded beach chair position. Standard anterior and posterior arthroscopy portals were made, and a diagnostic arthroscopy of the glenohumeral joint was completed.
The arthroscope was then moved into the subacromial space and a lateral portal was created. The subacromial space was debrided using a radiofrequency device exposing the coracoacromial ligament. An anterolateral portal was then created and the arthroscope moved into the lateral portal. The radiofrequency device was then used through the anterolateral portal to clear bursal tissue from around the coracoid exposing the superior, lateral, and inferior portions of the coracoid. Care was taken to maintain the working surface of the device against the coracoid and to avoid proceeding medial or distal on the coracoid, in order to avoid neurovascular injury.
A 3 cm incision was made over the distal clavicle 2–3 cm medial to the distal end of the clavicle. A suture shuttling device was introduced anterior to the clavicle through the clavicular incision. It was visualized through the arthroscope on the medial side of the coracoid and passed inferior to the coracoid. The loop was retrieved with a looped suture grasper, and No. 5 nonabsorbable suture was shuttled around the coracoid. On the clavicle, a 6 mm hole was drilled approximately 1.5 cm medial to the AC joint, followed by a second hole drilled 2 cm medial to the first. The suture shuttling device was passed through each clavicular tunnel and used to shuttle one end of the No. 5 nonabsorbable suture through each clavicular tunnel.
One end of the No. 5 nonabsorbable suture was tied to the suture placed through a semitendinosus allograft as well as to one end of a core suture with a braided exterior. Both the core suture and the suture attached to the graft were then passed through one tunnel, around the coracoid, and through the second tunnel. Tension on the suture attached to the graft then allowed the graft to be advanced around the coracoid and into position. The AC joint was manually reduced, and the core suture was clamped over the bony bridge between the clavicle tunnels for provisional fixation. Fluoroscopy was used to verify that acceptable reduction was obtained and then maintained with longitudinal traction on the arm and the core suture was tied. This intraoperative image is seen in Fig. 18.6. Tension was then applied to both limbs of the graft and interference screws were advanced, while manual reduction was again used to keep the AC joint reduced during final fixation. Repeat fluoroscopic exam was similar to the previous images, and the wounds were closed.