Introduction
The foot can be divided into three compartments according to the bony anatomy: the forefoot (comprising the metatarsals and phalanges, the midfoot (the cuneiforms, cuboid and navicular) and the hindfoot (calcaneus and talus).
Midfoot pain and metatarsalgia are common clinical complaints. The aetiology of the symptoms is often difficult to establish clinically and imaging therefore plays an important role in the evaluation of patients. Although radiographs give a good overview of bony anatomy and allow the evaluation of bony lesions, they may be unhelpful in the assessment of soft tissue lesions and early bony abnormalities. With its superficial soft tissue structures, the midfoot and forefoot are ideally suited to evaluation with ultrasound.
This chapter covers the wide range of pathology that may give rise to midfoot and forefoot symptoms, including trauma, masses, synovitis, infection and tendinopathy.
Technical Aspects
High-frequency linear array probes (7.5 MHz or higher) should be used. Focal zones should be centred at the level of interest. Important artifacts to be aware of are anisotropy and beam edge artifact. Anisotropy occurs in structures that have fibres running in a single direction, such as tendons and ligaments. When the angle of insonation is not perpendicular to the structure there may be a dramatic drop-off in echogenicity, which may simulate an abnormality. Technology such as beam steering and compound imaging may help to minimize this artifact. Beam edge artifact occurs at the edge of tendons with loss of signal and distal acoustic shadowing that may obscure adjacent structures.
A copious layer of jelly is very helpful when evaluating superficial structures, particularly if skin contact cannot easily be achieved across the length of the probe. An interposed layer of gel can also help to minimize skin pressure and avoid compression of vessels when examining superficial structures with Doppler. Extended field of view imaging is useful in giving an overview of the anatomy and improves image presentation when demonstrating abnormalities to colleagues.
Doppler imaging has a crucial role in musculoskeletal ultrasound, allowing a real-time evaluation of regional blood flow, which may be altered in a variety of pathological conditions, including inflammation, infection and tumours. Doppler imaging also has an increasingly important role in the follow-up imaging, to assess therapeutic response. In general, power Doppler is preferred over colour Doppler for musculoskeletal ultrasound, as the former is subject to less background noise, is not affected by aliasing and is independent of the angle of insonation.
Trauma
Foreign Body
Foreign bodies are commonly found in the sole of the foot and may present as localized masses. Often the patient will recall a penetrating injury.
Imaging
Foreign bodies appear as hyperechoic fragments, usually with a linear configuration. Glass or metal often results in posterior acoustic shadowing but organic material such as splinters may not demonstrate this finding. Abscesses surrounding foreign bodies appear as heterogeneous, ill-defined, low-echogenicity collections with peripheral increased vascularity on Doppler.
Granuloma formation may occur around foreign bodies with a hypoechoic halo surrounding the foreign body.


Stress Fracture
Plain radiographs may be normal for several weeks before a periosteal reaction or fracture line appears in patients with stress fracture. The gold standard for the early detection of stress fractures is considered to be MRI. Ultrasound, however, does have a role. Moreover, the recognition of stress fractures on ultrasound is important, as this is a relatively frequent unexpected finding in patients presenting with metatarsalgia. The middle and distal portions of the second and third metatarsal shafts are most commonly affected.
Imaging
On ultrasound an acute stress fracture appears as a focal area of cortical disruption with associated hypoechoic haematoma and periosteal elevation. There is usually increased Doppler signal around the periosteal lesion. If a suspected stress fracture is seen it is prudent to obtain plain radiographs to confirm the lesion and act as a baseline ( Fig. 28.3 ).

Plantar Plate Injury
Plantar plate injury or insufficiency may be the result of wearing high-heeled shoes, hypermobility, acute hyperextension trauma or overuse. Although overall the second metatarsophalangeal joint (MTPJ) is most commonly involved, turf toe describes an acute hyperextension injury of the first MTPJ with rupture of the plantar plate. This condition is usually associated with playing sports on a hard surface such as artificial turf. The injury typically occurs at the distal insertion of the plantar plate. Running and push-off are usually compromised. In the long term, the injury may result in hallux rigidus and hallux valgus.
Anatomy and Imaging
The plantar plate is a fibrocartilaginous supporting structure that connects the base of the proximal phalanx to the metatarsal neck, blending in with the sesamoids and tendons of the flexor hallucis brevis. Its function is to resist hyperextension of the MTPJ.
| The plantar plate is best visualized in the longitudinal plane, and appears as a low-echogenicity band, curving over the metatarsal head to insert into the proximal phalanx. |


Most plantar plate injuries can be managed nonsurgically with insoles and strapping, with severe injuries requiring long-term immobilization in a boot or cast. If conservative treatment is unsuccessful, surgery is considered.
Sesamoiditis
The term ‘sesamoiditis’ covers a spectrum of pathological conditions, including stress fractures, osteochondritis, chondromalacia and avascular necrosis of the sesamoid bones of the first hallux. Sesamoiditis is usually caused by repeated forefoot loading such as dancing and running. The onset may be acute or develop insidiously. Patients complain of pain beneath the first MTPJ, with restricted movement of the joint. The medial sesamoid is most affected and it is usually bipartite.
Imaging
The hallux sesamoids are embedded within the medial and lateral slips of the flexor hallucis brevis tendon at the level of the first metatarsal head. A thick intersesamoid ligament connects the sesamoids, which in turn are attached to the base of the proximal phalanx by the sesamoid-phalangeal ligament. The anatomical arrangement forms part of a gliding mechanism that reduces friction and protects the tendon. A primary function of the hallux sesamoids is to absorb the weight-bearing force of the medial forefoot.
Plain radiographs should be obtained to assess for sclerosis or fragmentation of the sesamoids. In nearly all cases of sesamoiditis, the sesamoid bone is bi- or multipartite. On MRI there may be bony fragmentation with bone oedema on fluid-sensitive sequences. If there is avascular necrosis the affected sesamoid is of low signal on all sequences. Ultrasound may show fragmentation of the sesamoids, and in some cases there may be associated tendinopathy of the flexor hallucis longus tendon. Bipartite sesamoids can be difficult to differentiate from sesamoid fractures and most may even be fractures. Acute fractures have sharp, uncorticated margins, but this cannot usually be appreciated on ultrasound ( Fig. 28.6 ).

Patients are usually managed by offloading the sesamoid by activity modification and orthotics. Ultrasound-guided injection of steroid between the sesamoid and the metatarsal may also decrease pain. Surgery may alter the biomechanics of the forefoot and cause hallux valgus or claw toe deformity, and so should be undertaken with caution.
Freiberg’s Infraction
Freiberg’s infraction is characterized by collapse of the second or third metatarsal head, which is thought to be related to repetitive trauma, resulting in microfractures and avascular necrosis. It occurs more commonly in females and typically affects adolescents. The disease is more common when the first metatarsal is shorter than the second.
Imaging
On radiographs there is initially sclerosis of the metatarsal head, followed by collapse and irregularity. On ultrasound the metatarsal head is flattened and irregular. There is often synovitis at the MTPJ, which may be associated with increased vascularity on Doppler ( Fig. 28.7 ).

With most cases of Freiberg’s infraction off-loading the metatarsal head may be sufficient. If synovitis is a major feature, steroid injection may give long-term pain relief. Surgery can be helpful in patients with on-going pain.
Masses
Ultrasound is often the first imaging modality used in the evaluation of soft-tissue masses. It allows a quick and effective means of confirming the presence of a lesion, and provides valuable information on the site, size, morphology and anatomical relations. Ultrasound can readily determine the cystic nature of ganglia, synovial cysts and bursitis. The location of the lesion in the foot can help narrow the diagnosis. For example, lesions between the metatarsal heads are almost invariably Morton’s neuromas or bursae.
The differential for lesions in the sole of the foot includes plantar fibromatosis, fat necrosis, epidermoid inclusion cyst and foreign body granuloma.
Morton’s Neuroma
In 1876 Thomas Morton described ‘a peculiar and painful affection of the fourth metatarsophalangeal articulation’ which subsequently became known as a Morton’s neuroma. Morton’s neuroma is not a true neuroma, but instead represents perineural fibrosis and neural hypertrophy of the interdigital nerve as it passes between the heads of the metatarsals. The 2/3 interspace is most commonly affected, followed by the 3/4 interspace. The female-to-male ratio for Morton’s neuroma is around 5 : 1, which is thought to relate to footwear. Patients typically present with pain and paraesthesia, with burning or tingling sensations in the affected toes. The symptoms may be intermittent with episodes related to activity. Often patients describe the sensation of a pebble in the shoe. With lateral compression of the forefoot the pain is reproduced and there may be a palpable and audible Moulder’s click.
Imaging
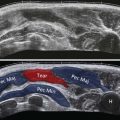
The patient should be positioned supine on the couch with their foot in the neutral position. As described in Chapter 23 , evaluation for Morton’s neuroma is best performed with the probe in the sagittal plane positioned either on the dorsum or plantar aspect of the forefoot. The forefoot is held steady with one hand while the probe is passed slowly across the MTPJ into the intermetatarsal space, and then across to the next MTPJ. When the probe is directly over the intermetatarsal space…
| … it can be very helpful to press a finger into the dorsal aspect of the space to try to elicit symptoms and also improve the conspicuity of a suspected Morton’s neuroma. |
Typically, a Morton’s neuroma appears as a round or ovoid hypoechoic nodule, in the sagittal plane on the plantar aspect of the intermetatarsal ligament. They can be of varying size, often 1 cm in diameter or greater. The significance of smaller lesions is uncertain. Careful evaluation may reveal the intermetatarsal nerve entering the nodule. Occasionally, a bilobed configuration may be present with a component extending dorsally. A Morton’s neuroma is usually slightly compressible, whereas a highly compressible lesion suggests an associated intermetatarsal bursa. However, a clear distinction between these two entities is difficult and often they coexist. This has led to the more generally used descriptive term ‘Morton’s neuroma and intermetatarsal bursal complex’ or, more simply, Morton’s bursa complex. In the transverse plane a Morton’s neuroma can be visualized as a mushrooming lesion arising on the plantar aspect between the heads of the metatarsals, particularly on lateral compression of the forefoot (Moulder’s manoeuvre). In some patients a palpable click occurs, although …
| … Moulder’s click has been shown to be a very nonspecific sign with clicks occurring with or without an accompanying neuroma or the click occurring in one interspace and the neuroma in another. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree