Introduction
Due to the superficial location of many of the structures that contribute to medial sided symptoms, ultrasound plays an important role in their assessment. Abnormalities of the medial tendons predominate, but disorders of the neurovascular structures, ligaments and even bones need to be considered. The technique for examining the medial ankle has already been discussed. Important points include the dominant role that axial images play in the assessment of tendon disease and this is particularly important in the medial ankle where the tendons follow a curved course around the medial malleolus. Each of the conditions that can contribute to medial side of symptoms will be discussed in turn.
Tibialis Posterior Tendon
The tibialis posterior tendon (TPT) is the most powerful inverter of the foot and helps to stabilize the medial longitudinal arch. TPT dysfunction is one of the commonest causes of medial sided ankle pain and is particularly prevalent in the middle-aged and older population. The cause of tendinopathy is multifactorial. Intrinsic factors combine with extrinsic and abnormal biomechanics to lead to tendon degeneration. Intrinsic factors include strain on the tendon as it passes a curved course around the medial malleolus. A zone of hypovascularity is said to occur in the watershed area between the proximal portion of the tendon supplied by the posterior tibial artery and the distal portion of the tendon supplied by a combination of the posterior tibial and dorsalis pedis arteries. Other areas of relative hypovascularity occur as the tendon sheath does not extend the full length to its insertion and there is no associated mesotendon. The combination of these anatomical features may predispose to tendon degeneration in this location. Other intrinsic factors include systemic disease, particularly diabetes, renal disease and rheumatoid arthritis, hypertension and use of steroids. Histologically, tendinosis is associated with replacement of the normal collagenous architecture with mucinous material that lacks structure or fibre organization. There is a decrease in the ratio of type 1 to type 3 collagen, and a reactive vascular ingrowth. This maladaptive repair is associated with tendon dysfunction.
Tendinopathy of the TPT is most common in middle-aged females who complain progressively of pain followed by flat foot deformity. Classically patients describe difficulty with walking on uneven ground, climbing and descending stairs. Clinically, tenderness is found on the medial aspect of the ankle along the line of the tendon. With advancing disease, the patient is unable to carry out a single heel raise.
The action of tibialis posterior in plantar flexing and everting is to maintain congruity at the talonavicular and calcaneocuboid joints during walking. Failure of this mechanism leads to flexion stresses of the midfoot and ultimately failure.
The TPT maintains the longitudinal arch of the foot and consequently its failure leads to flat foot deformity followed by sequential failure of the spring ligament and ligaments of the sinus tarsi.
Degenerate TPT tears usually occur at the level of the medial malleolus, whereas tears in athletes are usually at the navicular insertion.
Clinical and Radiological Staging
Both clinical and imaging staging has been described. The lower grades include the presence of pain without structural abnormality. This progresses through tendon degeneration to complete rupture when flat foot deformity is obvious. The clinical classification describes progressive dysfunction from stage I paratenonopathy, tenosynovitis and tendon degeneration with normal tendon length, through stage II with tendon elongation leading to correctable flat foot deformity, stage III with rigid flat foot deformity and finally stage IV with secondary medial ligament failure leading to valgus deformity. The imaging findings reflect clinical progression though is often normal in the early stages. Positive findings can be divided into those that involve the tendon sheath called tenosynovitis, and changes within the tendon itself.
Tenosynovitis
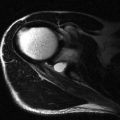
A small quantity of fluid is frequently found in the normal tendon sheath, particularly in the submalleolar region. A useful rule of thumb is that the cross-sectional area of fluid should not exceed that of the adjacent tendon. In the earliest stages, findings may be limited to excess fluid within the tendon sheath ( Fig. 27.1 ).
| Distension often begins in the immediate submalleolar area as this is where the sheath has room to expand ( Fig. 27.2 ). |





Hypertrophic, Atrophic and Calcific Tendinopathy
The earliest ultrasound changes of tendinopathy are focal areas of decreased reflectivity within the tendon.
| Under normal circumstances, blood vessels should not be found within a tendon apart from perhaps an occasional vessel close to the nutrient artery. |
Signal changes within the tendon should be carefully sought as their detection indicates progression to a more significant form of the disease.
These early abnormalities predominate in the submalleolar region and may be associated with other findings. There is a fibrous pulley enthesis on the posterior aspect of the medial malleolus where the TPT passes around it. Involvement of the enthesis may lead to bony hypertrophy and the formation of a spur on the posterior aspect of the medial malleolus ( Fig. 27.6 ). This may be visible on plain films and is a useful plain film clue to the underlying tendon disorder. It is also clearly visible on MR imaging, particularly in the axial plane.

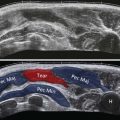
As the tendon begins to further elongate and as the arch of the foot drops, the tendon becomes further stretched. In some cases, there is a decrease in the cross-sectional area of the tendon that now appears of equal size to or smaller than the adjacent flexor digitorum tendon. The appearance of atrophic tendinopathy, as it is called ( Fig. 27.7 ), has been likened to a fraying rope. As the individual strands begin to dissociate, they slide apart, reducing the tendon cross-sectional area in the most involved segment ( Fig. 27.8 ). As has previously been outlined …
… the TPT is normally at least twice the size of flexor digitorum. Loss of this ratio is termed atrophic tendinopathy or type 2 partial tear.


Other forms of tendinopathy include acute calcific ( Fig. 27.9 ) and insertional tendinopathy. Fibrosing tenosynovitis is uncommon in the TPT, although it has been described. Calcification in the tendon sheath leading to acute calcific tenosynovitis is rare. A few flecks of calcification within the tendon, particularly at tendon insertions, should not be regarded as significant and calcification of this type is frequently asymptomatic. As with the supraspinatus tendon, occasionally acute calcific tendinopathy presents very acutely. The skin is red, the subcutaneous tissues are swollen and the tendon is very tender to touch. Calcium may be seen as a conglomerate within the tendon that can be associated with an increase in Doppler signal.