Introduction
Commoner causes of groin discomfort in the general population include inguinal hernias and muscle strains in the lower abdominal wall and upper thigh. Muscular strains in this group of patients often do not present to a primary care physician and certainly further management in the form of imaging is not necessary. The majority of symptomatic inguinal hernias can also be diagnosed clinically but there is a role for imaging in equivocal cases as there are well-recognized limitations to clinical assessment. The clinical role of ultrasound in the assessment of patients with groin pain has greatly increased in the last 10 years and this technique is now commonly used for the diagnosis of clinically indeterminate hernias and for the assessment of postoperative patients with groin pain.
The situation in the professional athlete is more controversial, with a number of aetiologies for chronic groin pain described. Especially in the case of osteitis pubis, adductor dysfunction and prehernia complex (or sportsman’s hernia), research has been relatively anecdotal, describing a number of differing pathologies and treatments. Although there are a large number of pathologies that can cause groin pain, including infection, neuralgia or tumour, this section will concentrate on inguinofemoral hernias and muscular strain, highlighting the strengths and limitations of ultrasound.
Normal Anatomy
Anatomically the groin contains the soft tissues of the inguinofemoral region between the anterior superior iliac spine and the symphysis pubis involving the upper thigh and inferior abdominal wall. Soft tissue structures include the skin, superficial fat and fascia, musculature (abdominal and upper thigh), extraperitoneal (preperitoneal) fat and peritoneum.
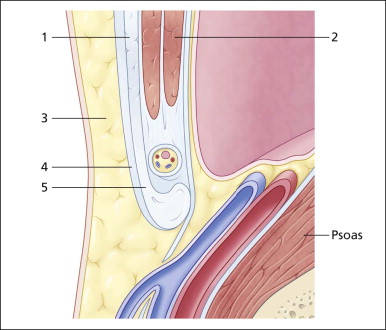
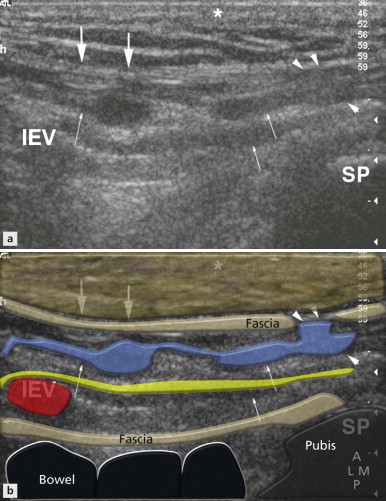
The inguinal canal allows the passage of vessels, nerves, lymphatics and the spermatic cord (round ligament in females) from within the abdomen to the external genitalia. The posterior wall of the canal is formed by the muscle, aponeurosis and fascia of transversus abdominis and also part of the internal oblique. The anterior canal wall is formed from the fascia of the external oblique muscle ( Fig. 17.1 ). The deep (internal) inguinal ring is a defect within the transversus abdominis fascia that allows the contents of the inguinal canal to leave the abdomen and enter the canal proper. The canal then extends obliquely, medially and inferiorly towards the pubic crest where the superficial (external) inguinal ring, a defect in the external oblique fascia, allows the contents to leave the canal ( Fig. 17.2 ). Superficial to the canal is subcutaneous fat and skin, whereas the iliopsoas muscle lies deep to it on its medial aspect and the external iliac vessels pass on the lateral aspect as they enter the thigh. The peritoneum and small bowel lie posterosuperiorly ( Figs 17.1 and 17.2 ).
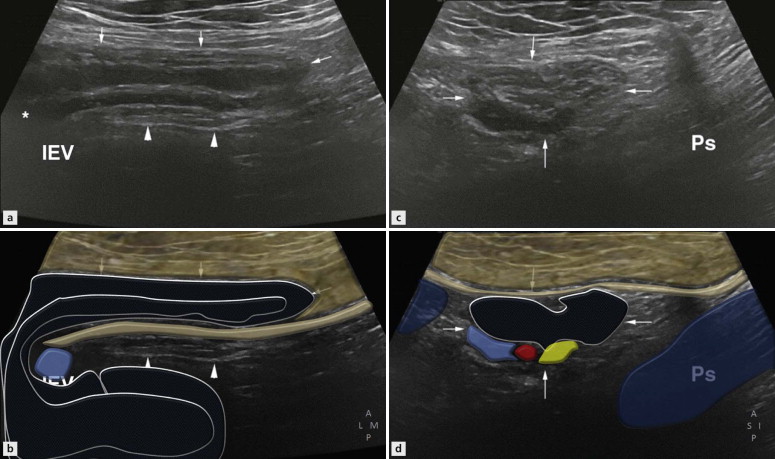
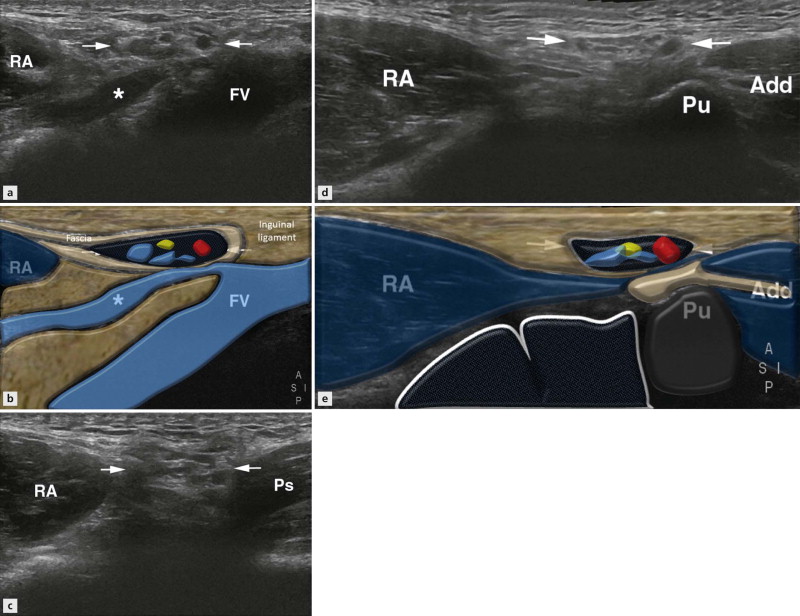
Important landmarks include the inferior epigastric vessels (IEVs), which arise from the external iliac vessels and course superiorly deep to rectus abdominis ( Figs 17.3 to 17.5 ). Just after their origin from the external iliac vessels they lie immediately medial to the deep inguinal ring. Therefore if a hernia arises lateral to these vessels, it is indirect (passing through the internal ring), but if it arises medial to the vessels it is a direct hernia (bulging through the posterior wall).
Examination Technique and Normal Ultrasound Appearances
It is important to identify the deep inguinal ring when assessing for inguinal hernias. The canal can be initially identified in the long or short axis. Both methods are outlined below and whichever you choose is a personal preference as merely rotating the probe through 90° will obtain the other view.
Long Axis View
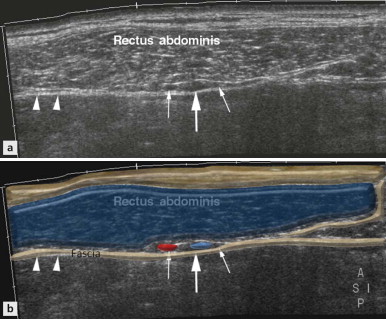
There are two main methods for visualizing the epigastric vessels, the landmark for assessing the deep ring on dynamic examination. The first method is to scan the rectus abdominis muscle transversely and identify the inferior epigastric vessels (IEVs) within the rectus sheath on its deep aspect ( Fig. 17.3 ). By continuous scanning in the transverse plane the vessels can be followed inferiorly as they sweep to join the external iliac vessels. However, in obese patients with lax musculature, although it is relatively easy to identify the vessels deep to rectus abdominis, it is difficult to continuously follow them because of the patient’s body habitus. Therefore, another technique is to begin with the femoral vessels in the transverse plane and move cranially until the epigastric vessels are seen at their origin and are beginning to pass medially. However, at this point, because the actual course of the inguinal canal is in the transverse oblique plane, the transducer should also be oblique by rotating the medial aspect of the transducer inferiorly.
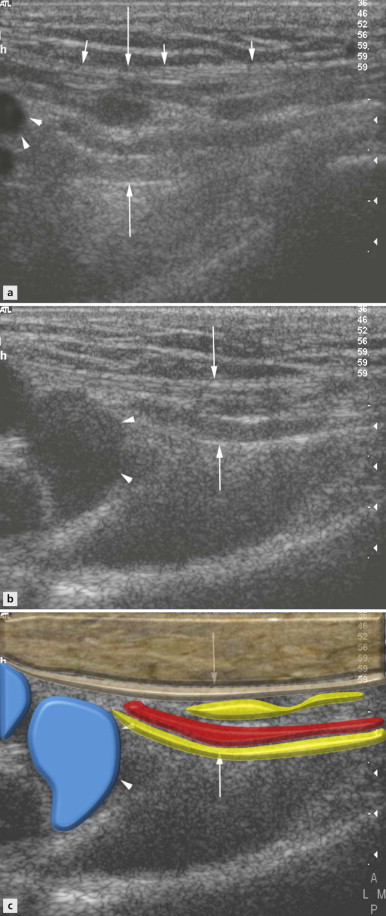
In this position a longitudinal image of the canal is obtained, which includes the epigastric vessels, femoral vessels and proximal inguinal canal. The inguinal ligament is seen as an echogenic line deep to the subcutaneous fat blending with the deep fascia ( Figs 17.2 and 17.4 ). Deep to the ligament are multiple hyperechoic and hypoechoic linear structures (representing vessels, nerves and cords) within the canal. Their prominence is variable and they pass medially to exit the canal through the external ring (seen as a defect of the inguinal ligament) ( Figs 17.2 and 17.4 ). Depending on body habitus the amount of fat within the canal will also vary. Deep to the canal lies the psoas muscle, but echogenic peritoneum and hypoechoic bowel (and a varying amount of preperitoneal fat) lie posterosuperiorly ( Figs 17.1 and 17.5 ).
Assessment of this area with the patient at rest and straining (performing a slow Valsalva manoeuvre) is now performed.
With Valsalva manoeuvre, there is normally bulging of the posterior wall and peritoneum but it should not completely occlude the canal ( Fig. 17.4 ).
| It is important to instruct the patient to perform the Valsalva manoeuvre slowly (i.e. not cough) and to ensure that transducer pressure is not applied too firmly otherwise any potential hernia will be maintained in reduction. |
Short Axis View
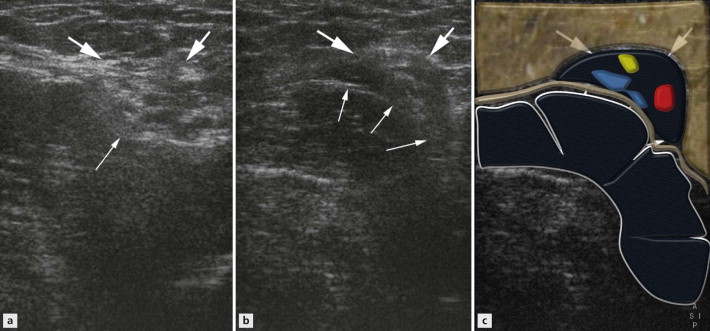
The canal should then be assessed in its short axis, which is the anatomical sagittal plane ( Fig. 17.1 ). To primarily obtain this view a sagittal image of the hip is obtained. The probe is then moved medially to the external iliac/femoral vessels and longitudinally to view the IEVs as they arise and begin to pass superiorly towards rectus abdominis ( Fig. 17.5A ). At this point the transducer should be moved slightly more medially to come off the epigastric vessels. The short axis of the inguinal canal with its hypoechoic tubular contents can now be visualized with peritoneum and bowel posterosuperiorly ( Fig. 17.5 ). On straining in a normal subject, there may be slight dilatation of the vessels within the canal and the bowel should move towards the canal but should not completely efface or enter the canal ( Fig. 17.6 ).
Ultrasound Appearance of Inguinal Hernias
Indirect hernias protrude through the internal inguinal ring and extend along the inguinal canal parallel to its long axis. The hernia usually consists of peritoneum, fat and bowel. Occasionally the hernia can be congenital due to a persistent processus vaginalis; however, this can be an incidental finding with the condition persisting in 29% of adults.
Direct inguinal hernias occur due to a defect in the posterior inguinal wall, within the transversus abdominis fascia, allowing protrusion of peritoneum and bowel through the wall into the inguinal canal. Because of this the hernia rarely continues distally along the inguinal canal itself and is more localized in comparison to indirect hernias.
On ultrasound the appearance of the normal inguinal contents can be variable and, unless there is a large irreducible hernia present, it is difficult to determine a small hernia within the canal on static imaging.
It is during the dynamic component of the examination that the hernia sac and its contents can be observed moving into the canal and reducing (partially or completely) on rest with transducer pressure.
| In the transverse plane a direct hernia will protrude through the posterior canal wall medial to the epigastric vessels ( Fig. 17.9A ). |