Introduction
Lateral and posterior hip pain may be due to variety of intra- and extraarticular conditions. Ultrasound is a useful image modality for rapid assessment of extraarticular soft tissue abnormalities, many of which are tendon or muscle related. Certain specific soft tissue mass lesions occur around the lateral aspect of the hip, and may or may not be associated with pain.
Common conditions include:
- •
greater trochanteric pain syndrome
- •
iliotibial band (ITB) snapping
- •
lateral hip masses
- •
tensor fasciae latae (TFL) tendinopathy and hypertrophy
- •
hamstring tendinopathy
- •
sciatic nerve compression and piriformis syndrome.
Greater Trochanter Pain Syndrome
Abductor tendon abnormalities are a common cause of the so-called greater trochanter pain syndrome:
- •
abductor tendinopathy
- •
abductor tendon tears
- •
gluteal bursitis
- •
abductor calcific tendonitis.
Patients present with a dull, aching pain over the lateral and posterior aspect of the greater trochanter, often with focal tenderness on palpation. Pain usually occurs while walking or lying on the affected side. However, in the majority of patients there is no limitation of movement. Pain is mostly unilateral, but sometimes bilateral. Middle aged and elderly women are commonly affected, where a wider pelvis is thought to be a contributory factor. Symptoms are often accredited to trochanteric bursitis, but it is more frequently due to gluteus medius and minimus tendinopathy associated with subgluteus medius and minimus bursitis. The aetiology of abductor tendinopathy is unknown, but it is thought that microtrauma causes tendon degeneration and tearing at the tendon insertion.
Tendon insertion abnormalities are readily amenable to sonographic evaluation. Anisotropy may be encountered on longitudinal scanning due to the oblique course of gluteus medius tendon fibres, which may mimic a tear or tendinopathy.
| In obese patients it may be necessary to use probe pressure or decrease probe frequency to adequately visualize the tendon insertion. |


Partial thickness tears usually involve the deep and anterior fibres of the gluteus medius tendon. Partial tears appear as areas of tendon thinning or anechoic defects in the tendon substance.
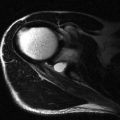
A ‘bald facet’ and absence of tendon fibres are consistent with a full-hickness tear ( Fig. 19.3 ).

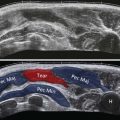
The trochanteric bursa, or subgluteus maximus bursa, is a crescenteric low-echo structure that lies lateral and superficial to the gluteus medius insertion, adjacent to the posterior facet of greater trochanter, and deep to the gluteus maximus muscle. Trochanteric bursitis is thought to be the result of an impingement phenomenon and may be present in up to 40% of patients with gluteus medius and minimus tendinopathy ( Fig. 19.4 ). If the hip abductors are weakened by tendinopathy, lateral subluxation of femoral head occurs, leading to impingement of the soft tissues between the greater trochanter and the iliotibial tract and development of bursitis. Therefore, trochanteric bursitis may be a sequela of hip joint instability, and hence the association with tendinopathy. Bursitis is commonest in the fifth and sixth decades but may be encountered in other age groups. Other less common causes of trochanteric bursitis are rheumatoid arthritis, tuberculosis and other systemic inflammatory conditions.

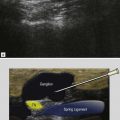
Calcification in the gluteal tendons has been reported in 10–40% of cases of gluteal tendinopathy. This can be linear or in the form of multiple small foci near the tendon insertion, and is often a result of degenerative tendinopathy. However, larger deposits of calcific tendinopathy may occur in hydroxyapatite deposition disease. The calcification appears as areas of increased echogenicity, which may or may not cast an acoustic shadow dependent on size and status of the calcification ( Fig. 19.5 ). Spontaneous resorption of the calcific deposits may occur. Calcific tendinosis may be associated with trochanteric bursitis.