Distal Intestinal Obstruction in a Neonate
Ramesh S. Iyer, MD
LEARNING OBJECTIVES
1. Identify distal bowel obstruction on neonatal abdominal radiographs.
2. Recognize a microcolon.
3. Discuss how the presence or absence of a microcolon may be used to tailor your differential diagnosis for distal bowel obstruction.
4. Describe differences in enema findings and management between ileal atresia and meconium ileus (both ileal disorders causing microcolon).
5. Identify typical features of Hirschsprung disease on contrast enema, including an abnormal rectosigmoid (R/S) ratio.
6. Identify typical features of meconium plug syndrome on contrast enema.
7. Discuss additional anomalies associated with anorectal malformations.
8. Describe imaging features of anorectal malformations, including calculating a sacral ratio and findings on distal colostogram.
INTRODUCTION
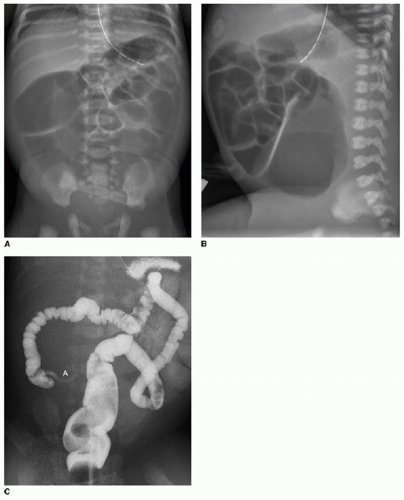
The majority of neonates with distal bowel obstruction present with abdominal distension and failure to pass meconium within their first 24 to 48 hours of life. Radiography shows distension of proximal and distal bowel (Fig. 13.1A, B). It is not possible to reliably distinguish small bowel from colon in young infants on radiography, and therefore, “proximal” and “distal” are used. Contrast enema using a water-soluble iso-osmolar agent should then be performed. Water-soluble contrast agents are preferred over barium in neonates because of their potential to be therapeutic, while barium may exacerbate obstruction from inspissated meconium. Water-soluble agents are also favored when there is a possibility of bowel perforation.1
A primary goal with contrast enema is to determine the presence or absence of a microcolon (Fig. 13.1C). A microcolon refers to large intestine that is diffusely small in caliber due to disuse. While there is no consensus regarding what luminal caliber constitutes a microcolon, the term has been applied when the colon is distended with contrast and does not exceed 1 cm.2 In general, when there is a microcolon present, then ileal pathology is suspected. Ileal atresia and meconium ileus are the most likely causes of microcolon. Total colonic or total intestinal Hirschsprung disease also produces a microcolon, but is rare. If there is no microcolon, then a colorectal disorder is likely, making Hirschsprung disease and meconium plug syndrome the primary considerations. This categorization is summarized in Table 13.1. Anorectal malformations will be discussed separately at the end of the chapter.
ILEAL DISORDERS (MICROCOLON PRESENT)
Ileal atresia
The small bowel is the most common site of atresia in the gastrointestinal tract, accounting for approximately half of cases. The duodenum is the next most common site at 40%, followed by the colon (approximately 10%).1,3 In contrast to duodenal atresia, which is caused by failure of luminal recanalization, it is widely accepted that small bowel atresia results from an intrauterine vascular injury. Predisposing conditions for intestinal ischemia with subsequent atresia include gastroschisis, omphalocele, and in utero volvulus or intussusception.4, 5, 6 and 7 Ileal atresia is much more common than is stenosis and occurs in the distal ileum in two-thirds of cases.1 Multiple atretic segments may be present in a minority of cases. Postnatal presenting symptoms of ileal atresia include failure to pass meconium within the first 24 to 48 hours of life, abdominal distension, and less commonly bilious emesis and jaundice. Prenatal imaging may reveal polyhydramnios that increases in severity with more proximal atresia.1,7
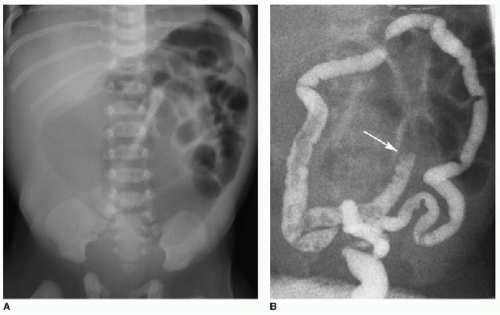
On radiography, neonates with ileal atresia will display gaseous distension of both proximal and distal bowel, often with
bulging flanks and elevated diaphragm (Figs. 13.1A, B and 13.2A). There will be no rectal gas, which is best assessed on a lateral projection. Contrast enema will demonstrate a microcolon (Figs. 13.1C and 13.2B). Contrast refluxes into a collapsed terminal ileum before cessation at a cutoff point (Fig. 13.2B). The dilated small bowel loops above the atretic segment will not fill with contrast.1,4,7,8
bulging flanks and elevated diaphragm (Figs. 13.1A, B and 13.2A). There will be no rectal gas, which is best assessed on a lateral projection. Contrast enema will demonstrate a microcolon (Figs. 13.1C and 13.2B). Contrast refluxes into a collapsed terminal ileum before cessation at a cutoff point (Fig. 13.2B). The dilated small bowel loops above the atretic segment will not fill with contrast.1,4,7,8
Table 13.1 CATEGORIZATION OF DISTAL BOWEL OBSTRUCTIVE DISORDERS IN NEONATES | |||||||
|---|---|---|---|---|---|---|---|
|
Treatment of ileal atresia is achieved by resecting the atretic segment and performing either a primary anastomosis or a tapering enteroplasty. Long-term patient outcomes following surgical
management are favorable, with a survival rate of 80% to 90%. Potential complications include short-bowel syndrome, intestinal dysmotility, and adhesions.7
management are favorable, with a survival rate of 80% to 90%. Potential complications include short-bowel syndrome, intestinal dysmotility, and adhesions.7
Meconium ileus
Meconium ileus accounts for 20% of neonatal bowel obstruction.1 The obstruction is located in the terminal ileum and is caused by the accumulation of inspissated meconium. The vast majority of children with meconium ileus become diagnosed with cystic fibrosis (CF). Meconium ileus is the presenting illness in 10% to 20% of CF patients.9, 10, 11 and 12 The pathology may occur in the absence of CF; however, the exact pathogenesis in these cases has not been fully elucidated.12,13 Patients with CF have defective chloride transport across cell membranes in multiple organ systems (discussed in more detail in Chapter 8). Within the fetal bowel, the resultant electrolyte imbalance and increased protein content give rise to thick, tenacious meconium. This material inspissates in the distal small bowel and causes a highgrade obstruction.1
Meconium ileus presents with abdominal distension and failure to pass meconium within the first 1 to 2 days of life. The condition may be subdivided into simple and complex meconium ileus. Complex meconium ileus occurs in 40% to 50% of cases and may be associated with intrauterine volvulus, atresia, necrosis, or perforation. When bowel perforation occurs in utero, sterile meconium spills into the peritoneal cavity, termed meconium peritonitis.12 Meconium peritonitis may result from bowel perforation of any etiology and is not specific to meconium ileus.
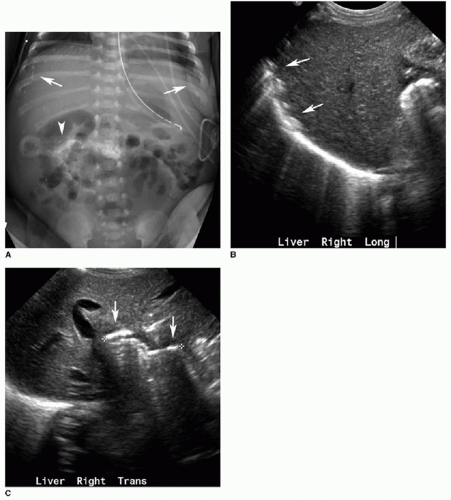
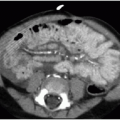
On radiography, simple meconium ileus shows a distal bowel obstruction with no rectal gas in the neonate, similar to ileal atresia. Gas-fluid levels are usually not seen because of the pasty consistency of the luminal contents. Meconium peritonitis manifests as multiple intraperitoneal calcifications, while a meconium pseudocyst (a single loculated collection) will exert mass effect upon adjacent bowel loops (Fig. 13.3). Occasionally, the inspissated meconium in the distal ileum produces bubbly lucencies that have been likened to a “soap bubble” appearance.4,12,14,15 As with ileal atresia, the next diagnostic imaging step would be to perform a water-soluble contrast enema, which will also reveal a microcolon. If contrast refluxes into the distal ileum, this segment is frequently filled with meconium pellets and may be distended, in contrast to the collapsed terminal ileum in distal small bowel atresia (Fig. 13.4). Contrast may or may not traverse the distal ileum into the dilated small bowel loops upstream of the obstruction.1,8,10,11
Prenatal imaging findings that suggest meconium ileus include fetal bowel that is abnormally dilated or echogenic (brighter than bone).12,16 Prenatal ultrasound may identify punctate echogenic foci with posterior acoustic shadowing scattered throughout the abdomen, representing meconium peritonitis.4 Fetal MR will also show dilated bowel loops with T1-hyperintense intraluminal contents for both meconium ileus and ileal atresia.17
The mainstay of initial treatment for simple meconium ileus is water-soluble enema with hyperosmolar agents such as diatrizoate meglumine and diatrizoate sodium (Gastrografin). While success rates vary widely in the literature, performing serial enemas may increase treatment efficacy. The radiologist should be aware of the risks of fluid shifts and further electrolyte imbalance by using hyperosmolar contrast agents. Surgery is reserved for patients who do not respond to enemas and for cases of complex meconium ileus. In such cases, enterotomy with meconium evacuation is performed, sometimes requiring a temporary doublebarrel enterostomy.1,11,12,18
COLORECTAL DISORDERS (MICROCOLON ABSENT)
Hirschsprung disease
Hirschsprung disease is functional obstruction of the distal bowel caused by the congenital absence of enteric ganglion cells. It is characterized as a neurocristopathy and results from arrested migration of vagal neural crest cells. The aganglionic bowel segment lacks parasympathetic Auerbach (intermuscular) and Meissner (submucosal) plexuses. The affected bowel is spasmodic and contracts, and the obstruction causes the upstream bowel to dilate.2,19,20 Several potential causative genetic mutations have been identified. The RET protooncogene at 10q11 is responsible for 20% of sporadic cases and up to half of familial cases.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree