10 | Doppler Ultrasound Diagnosis in Preeclampsia, Eclampsia, and HELLP Syndrome |
The Working Group on High Blood Pressure in Pregnancy classifies hypertensive disorders in pregnancy as follows:
 Preeclampsia/eclampsia: Occurs after the 20th week; increased bood pressure (gestational hypertension) with proteinuria. Eclampsia adds tonic/ clonic seizures. HELLP syndrome: hemolysis, elevated liver enzymes, low platelet count;
Preeclampsia/eclampsia: Occurs after the 20th week; increased bood pressure (gestational hypertension) with proteinuria. Eclampsia adds tonic/ clonic seizures. HELLP syndrome: hemolysis, elevated liver enzymes, low platelet count;
 Chronic hypertension: primary or secondary;
Chronic hypertension: primary or secondary;
 Preeclampsia superimposed on chronic hypertension;
Preeclampsia superimposed on chronic hypertension;
 Gestational hypertension (only during pregnancy): Elevated blood pressure occurring after the 20th week of pregnancy that lasts no longer than six weeks postpartum. Proteinuria is absent;
Gestational hypertension (only during pregnancy): Elevated blood pressure occurring after the 20th week of pregnancy that lasts no longer than six weeks postpartum. Proteinuria is absent;
 Transient hypertension (only after pregnancy).
Transient hypertension (only after pregnancy).
‘Toxemia’ of pregnancy has been known since antiquity. The disease does not present a uniform clinical picture and its causes and pathogenesis have not been clearly defined to date. No doubt immunological changes play an important role. The vessels show constriction that interferes with blood flow. Vascular damage leads to subendothelial deposition of thrombo-cytes and fibrinogen. Ensuing disturbances in the microcirculation may eventually lead to the disseminated intravascular thrombosis of the HELLP syndrome. The term pregnancy-induced or gestational hypertension (PIH) was introduced to describe the principal symptom.
The endothelium probably plays a significant role in the pathophysiology of gestational hypertension (McCarthy et al. 1993, Roberts et al. 1981, Taylor and Roberts 1991). The production of prostacyclin, which acts as a vasodilator, is reduced in the endothelium, (Goodman et al. 1982, Mäkilä et al. 1984, Walsh 1985), while vasoconstrictive endothelin is increased (Nova et al. 1991). Additional nitrogen monoxide (NO), an endothelium-derived relaxing factor (EDRF), is probably an important factor in the genesis of gestational hypertension. The corresponding endothelial changes can be demonstrated morphologically (Furchgott and Zawadski 1980, Palmer et al. 1987, Pinto et al. 1991, Roberts et al 1981). Beinder and Lang (1994), using a laser Doppler flow meter, were able to show changes in the reactivity of the microcirculation in toxemic patients.
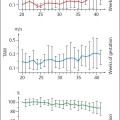
There is a fundamental change in hemodynamics during pregnancy. Partly this is due to the greatly dilated vascular bed. Total peripheral resistance can be observed to decrease considerably during the 14th to 24th week of pregnancy. The resistance then rises again slowly until the end of pregnancy to normal values similar to those found prior to pregnancy. An exception is renal perfusion, which has been found to rise steadily until the end of pregnancy.
In contrast to this normal course, during preeclampsia and eclampsia vascular resistance increases significantly as described above. This rise reduces perfusion and is responsible for the symptoms of preeclampsia.
Pathological Changes in Preeclampsia
Over time numerous hypotheses for the development of preeclampsia have been developed, based on its three cardinal symptoms, namely edema, proteinuria, hypertension (EPH) and the observation that it is often associated with fetal growth restriction.
The changes based on the most robust observations may be summarized as follows:
 Decreased perfusion of uterus and kidney,
Decreased perfusion of uterus and kidney,
 Reduced glomerular filtration rate,
Reduced glomerular filtration rate,
 Increased vascular sensitivity for angiotensin II,
Increased vascular sensitivity for angiotensin II,
 Reduced urine output after sodium loading,
Reduced urine output after sodium loading,
 Glomerular changes,
Glomerular changes,
 Fibrin monomers dissolved in the plasma.
Fibrin monomers dissolved in the plasma.
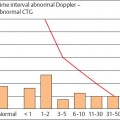
Plethysmographic studies found significant elevations in the total peripheral resistance in preeclamptic patients. This is the expression of contraction of the vascular musculature in the peripheral resistance system and a decrease in the resistance of the venous bed. A number of symptoms can be ascribed to this vascular spasm (Fig. 10.1).
The cause of the vasoconstriction and salt retention is considered to be the heightened sensitivity to angiotensin II, added to the decreased production of prostacyclin. The effects of prostacyclin include vasodilatation and inhibition of thrombocyte aggregation. Moreover, the fluid properties of the blood are altered by increased aggregation of erythrocytes and plasma viscosity, resulting in reduced perfusion. At the same time colloid osmotic pressure and the plasticity of the erythrocytes decrease.
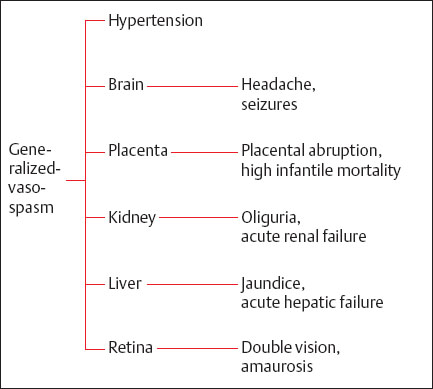
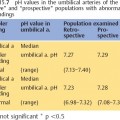
Fig. 10.1 The effects of vasospasm on various organs and development of symptoms.
Our own research showed that in women with preeclampsia uterine and renal vascular resistance was increased. In order to determine if this increase in resistance also affected other maternal vessels, we additionally examined the thyroid vessels. In these vessels there was no difference in perfusion between women whose pregnancy was normal, and those who suffered from preeclampsia, suggesting that the increase in resistance in the uterine and renal vascular beds must be of local origin. The reduction in perfusion in our preeclamptic population was more marked in the kidneys than in the uterus.
Another attempt to explain the pathogenesis of preeclampsia was by abnormal immune processes. However, despite an increase in antibody formation in preeclamptic women so far no unequivocal evidence has shown this process to be causative in the clinical picture of preeclampsia.
The primary symptom of preeclampsia is a rise in blood pressure in the course of pregnancy. The course of preeclampsia is monitored by following blood pressure and edema, as well as total protein and uric acid. Other available options include quantitative monitoring of albuminuria, ultrasonic monitoring of the fetus, and cardiotocography. Doppler ultrasound can provide important information concerning fetal condition in clinical picture.
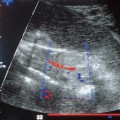
Changes in the placental vascular bed can be demonstrated by tissue examination in patients with preeclampsia and are relatively common. In such cases changes in the maternal vessels supplying the placenta may be demonstrated by Doppler ultrasound. Such Doppler sonographic changes can at times be demonstrated long before clinical symptoms appear, making Doppler ultrasound a future screening tool for preeclampsia (cf. Chapter 9, p.<). However, changes in the placental bed on the maternal side do not necessarily signify anomalies on the fetal side. In this respect the placenta has an enormous compensatory capacity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree