Echocardiography
Richard Andrew Taylor
Christopher L. Moore
INTRODUCTION
Emergency echocardiography is one of the most challenging ultrasound examinations for the emergency physician to become comfortable with, but is potentially the most rewarding. Some images and landmarks can be difficult to be obtained consistently and orientation may be confusing at times. However, certain focused applications are well within the scope of all emergency physicians and can provide immediate, valuable diagnostic information in a variety of presentations, from arrest situations to unexplained shock, dyspnea, or chest pain (1,2).
CLINICAL APPLICATIONS
Emergency echocardiography has been shown to provide diagnostic and prognostic information in an emergency department (ED) population with a variety of suspected cardiac-related symptoms (3, 4, 5, 6, 7, 8, 9). Emergency echocardiography is most likely to be effective when it is used in populations with a relatively high likelihood of pathology that is discernible by focused emergency echo: pericardial effusion, left ventricular systolic dysfunction, severe right ventricular strain, or aortic dilation. The great benefit of emergency echo is that it lowers the threshold for testing, and may aid in making diagnoses that might otherwise be missed if obtaining an echocardiogram is time-consuming, difficult, or even impossible in the ED setting. While much research still needs to be done regarding the training and utility of echo by emergency physicians, the most high-yield presentations that may benefit from emergency echocardiography, especially when the diagnosis is in doubt, are:
The use of emergency echo may provide valuable information in the diagnosis of:
It can also assist in bedside procedures (discussed further in Chapter 8) such as:
IMAGE ACQUISITION
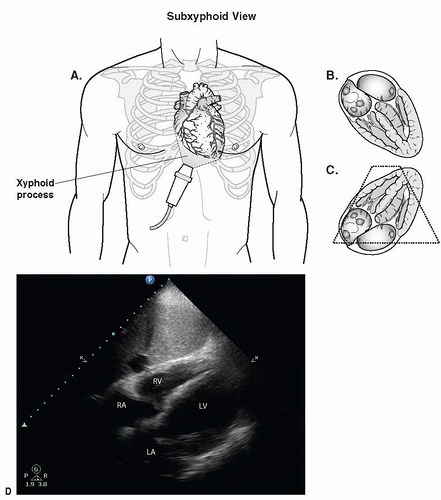
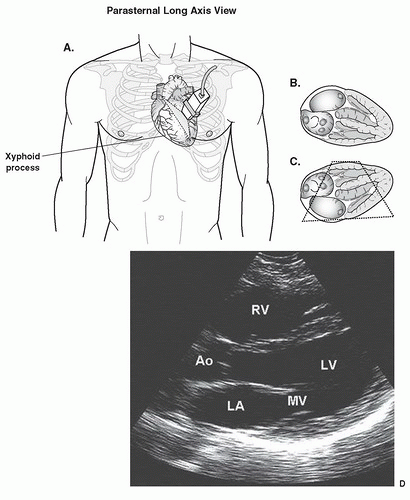
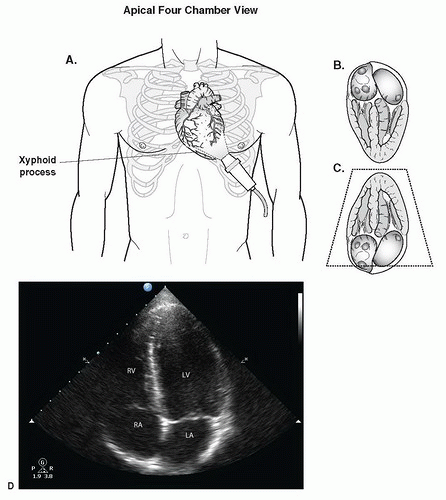
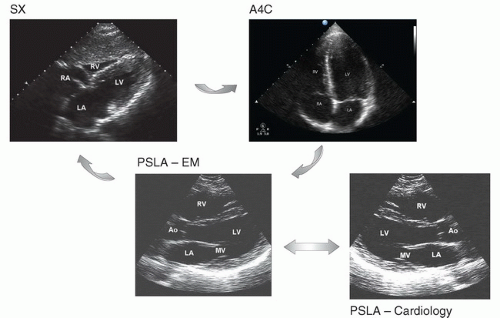
There are three basic sonographic windows to the heart: subxyphoid, parasternal long axis (PSLA), and apical fourchamber views (Figs. 4.1, 4.2, 4.3, 4.4 and 4.5). Many emergency physicians are most familiar with the subxyphoid (or subcostal) view as it is commonly taught as part of the trauma exam, although the parasternal window may be easier to obtain and often provides superior visualization of many cardiac structures. It can be difficult to obtain all three windows in all patients, but comfort with different views should allow some visualization in even the most difficult patients. Additional windows that may be of use to the emergency physician are the parasternal short axis and the suprasternal notch views (Fig. 4.2).
Begin with patients supine and completely flat if they are able to tolerate the position. Some windows may also be improved by having the patient assume a left lateral decubitus position, which pulls the heart away from behind the sternum and toward the ribs of the left chest. Because the heart is on the left side of the body, some sonographers choose to position the machine on this side of the patient, although scanning from the right side of the patient is typically not too difficult and may be more comfortable if other examinations are done from this side.
The transducer choice is typically a small footprint phasedarray transducer with a frequency range of 2 to 5 MHz, allowing visualization between the ribs, although, if unavailable, a curvilinear probe may be used, particularly for the subxyphoid view. Many machines have a cardiac setting or application for the transducer that is optimized for cardiac visualization allowing improved differentiation between myocardium and blood. If available, tissue harmonic imaging should be turned on to enhance visualization.
In contrast to many other areas of the body in which there are well-defined and separate internal anatomic landmarks, such as the vertebral body for abdominal aorta identification, the landmarks for sonographic images of the heart are structures within the heart itself, making it often difficult to initially orient oneself when scanning. The position of the heart in relation to external landmarks may vary remarkably from patient to patient. Obese patients tend to have a heart that is high up in the chest with a more transverse axis, while patients with chronic obstructive lung disease often have a heart in a nearly longitudinal axis and dropped down almost to the costal margin.
Scanning technique and transducer orientation may be a source of confusion in echocardiography. Cardiologists
typically perform echocardiography from the left side of the patient, with the transducer indicator corresponding to the right side of the screen. PEDIATRIC CONSIDERATIONS: Pediatric cardiologists perform echocardiograms with the image originating from the inferior portion of the screen (i.e., upside down as compared with standard ultrasound imaging).
PEDIATRIC CONSIDERATIONS: Pediatric cardiologists perform echocardiograms with the image originating from the inferior portion of the screen (i.e., upside down as compared with standard ultrasound imaging). This is in contrast to other emergency ultrasound examinations that are typically performed from the right side of the patient with the indicator corresponding to the left side of the screen. The net result is that in emergency echo, two of the three primary cardiac windows (subxyphoid and apical four-chamber) are consistent with a cardiology orientation. However, the PSLA view traditionally described by cardiologists is flipped so that the apex of the heart appears on the left side of the screen. This leaves the emergency physician with two choices in obtaining the PSLA view: either reverse the indicator in order to get an image that differs from typical emergency ultrasound orientation, or obtain a PSLA view that is consistent with abdominal applications, but reversed from a typical cardiology scan. In this text we have chosen to use an orientation consistent with the rest of emergency ultrasound, in which all windows (including the PSLA) are obtained by keeping the transducer to the patient’s right, with right-sided cardiac structures appearing on the left side of the screen as they are viewed. Regarding the primary cardiac views, the only image that will appear significantly different from illustrations in cardiology texts is the PSLA (Fig. 4.6) (14). With practice, using a consistent orientation (indicator in the arc from the patient’s right to the patient’s head), each of the three views will meld into a coherent picture of the heart, with the PSLA being slightly higher than the subxyphoid and rotated clockwise from the apical view, but with structures consistently oriented on the same side of the screen throughout (Fig. 4.6).
This is in contrast to other emergency ultrasound examinations that are typically performed from the right side of the patient with the indicator corresponding to the left side of the screen. The net result is that in emergency echo, two of the three primary cardiac windows (subxyphoid and apical four-chamber) are consistent with a cardiology orientation. However, the PSLA view traditionally described by cardiologists is flipped so that the apex of the heart appears on the left side of the screen. This leaves the emergency physician with two choices in obtaining the PSLA view: either reverse the indicator in order to get an image that differs from typical emergency ultrasound orientation, or obtain a PSLA view that is consistent with abdominal applications, but reversed from a typical cardiology scan. In this text we have chosen to use an orientation consistent with the rest of emergency ultrasound, in which all windows (including the PSLA) are obtained by keeping the transducer to the patient’s right, with right-sided cardiac structures appearing on the left side of the screen as they are viewed. Regarding the primary cardiac views, the only image that will appear significantly different from illustrations in cardiology texts is the PSLA (Fig. 4.6) (14). With practice, using a consistent orientation (indicator in the arc from the patient’s right to the patient’s head), each of the three views will meld into a coherent picture of the heart, with the PSLA being slightly higher than the subxyphoid and rotated clockwise from the apical view, but with structures consistently oriented on the same side of the screen throughout (Fig. 4.6).
typically perform echocardiography from the left side of the patient, with the transducer indicator corresponding to the right side of the screen.
 PEDIATRIC CONSIDERATIONS: Pediatric cardiologists perform echocardiograms with the image originating from the inferior portion of the screen (i.e., upside down as compared with standard ultrasound imaging).
PEDIATRIC CONSIDERATIONS: Pediatric cardiologists perform echocardiograms with the image originating from the inferior portion of the screen (i.e., upside down as compared with standard ultrasound imaging). This is in contrast to other emergency ultrasound examinations that are typically performed from the right side of the patient with the indicator corresponding to the left side of the screen. The net result is that in emergency echo, two of the three primary cardiac windows (subxyphoid and apical four-chamber) are consistent with a cardiology orientation. However, the PSLA view traditionally described by cardiologists is flipped so that the apex of the heart appears on the left side of the screen. This leaves the emergency physician with two choices in obtaining the PSLA view: either reverse the indicator in order to get an image that differs from typical emergency ultrasound orientation, or obtain a PSLA view that is consistent with abdominal applications, but reversed from a typical cardiology scan. In this text we have chosen to use an orientation consistent with the rest of emergency ultrasound, in which all windows (including the PSLA) are obtained by keeping the transducer to the patient’s right, with right-sided cardiac structures appearing on the left side of the screen as they are viewed. Regarding the primary cardiac views, the only image that will appear significantly different from illustrations in cardiology texts is the PSLA (Fig. 4.6) (14). With practice, using a consistent orientation (indicator in the arc from the patient’s right to the patient’s head), each of the three views will meld into a coherent picture of the heart, with the PSLA being slightly higher than the subxyphoid and rotated clockwise from the apical view, but with structures consistently oriented on the same side of the screen throughout (Fig. 4.6).
This is in contrast to other emergency ultrasound examinations that are typically performed from the right side of the patient with the indicator corresponding to the left side of the screen. The net result is that in emergency echo, two of the three primary cardiac windows (subxyphoid and apical four-chamber) are consistent with a cardiology orientation. However, the PSLA view traditionally described by cardiologists is flipped so that the apex of the heart appears on the left side of the screen. This leaves the emergency physician with two choices in obtaining the PSLA view: either reverse the indicator in order to get an image that differs from typical emergency ultrasound orientation, or obtain a PSLA view that is consistent with abdominal applications, but reversed from a typical cardiology scan. In this text we have chosen to use an orientation consistent with the rest of emergency ultrasound, in which all windows (including the PSLA) are obtained by keeping the transducer to the patient’s right, with right-sided cardiac structures appearing on the left side of the screen as they are viewed. Regarding the primary cardiac views, the only image that will appear significantly different from illustrations in cardiology texts is the PSLA (Fig. 4.6) (14). With practice, using a consistent orientation (indicator in the arc from the patient’s right to the patient’s head), each of the three views will meld into a coherent picture of the heart, with the PSLA being slightly higher than the subxyphoid and rotated clockwise from the apical view, but with structures consistently oriented on the same side of the screen throughout (Fig. 4.6).NORMAL ULTRASOUND ANATOMY AND PRIMARY CARDIAC WINDOWS
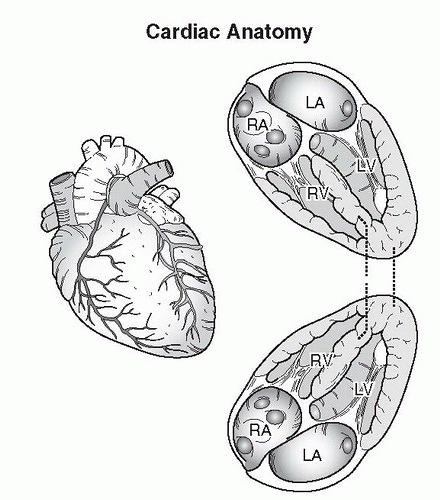
The heart is a three-dimensional structure that sits obliquely in the chest. The base of the heart, which includes the atria and major valves, is to the right and slightly posterior, while the apex of the heart points to the left, anteriorly and inferiorly (Fig. 4.1). Blood flowing from the right-sided inferior vena cava (IVC) joins the right atrium (RA), and then proceeds through the tricuspid valve to the right ventricle (RV).
Typically, hepatic veins in the liver can be followed sonographically into the IVC and then through the RA to the RV from a subxyphoid approach, which is often a useful maneuver for ultrasound orientation. The RV is anterior and to the right, with the free wall frequently seen adjacent to the liver. The left atrium (LA) is posterior and drains across the mitral valve to the muscular left ventricle (LV). The left ventricular outflow tract (aortic valve and aortic root) is in the center of the base of the heart and is typically best seen on the PSLA view. In general, the “long axis” of the heart may be thought of as a line that runs from the center of the base of the heart to the apex, corresponding to a line from the patient’s right shoulder to left lower flank. A long axis view is one in which the ultrasound plane is parallel to this line, while a short axis is perpendicular to this axis and typically cuts across the left ventricle, providing a “donut” type of image.
Typically, hepatic veins in the liver can be followed sonographically into the IVC and then through the RA to the RV from a subxyphoid approach, which is often a useful maneuver for ultrasound orientation. The RV is anterior and to the right, with the free wall frequently seen adjacent to the liver. The left atrium (LA) is posterior and drains across the mitral valve to the muscular left ventricle (LV). The left ventricular outflow tract (aortic valve and aortic root) is in the center of the base of the heart and is typically best seen on the PSLA view. In general, the “long axis” of the heart may be thought of as a line that runs from the center of the base of the heart to the apex, corresponding to a line from the patient’s right shoulder to left lower flank. A long axis view is one in which the ultrasound plane is parallel to this line, while a short axis is perpendicular to this axis and typically cuts across the left ventricle, providing a “donut” type of image.
Subxyphoid Window
The subxyphoid view is obtained by placing the transducer below the sternum at the costal margin with the transducer indicator to the patient’s right (Fig. 4.3). The plane of the ultrasound transducer should be angled up toward the left chest,  PEDIATRIC CONSIDERATIONS: The heart in young children sits more in the center of the chest. Therefore the plane of the beam is directed toward the chin as opposed to the left shoulder.
PEDIATRIC CONSIDERATIONS: The heart in young children sits more in the center of the chest. Therefore the plane of the beam is directed toward the chin as opposed to the left shoulder. with the transducer pressed nearly flat on the abdomen and a firm amount of pressure applied in order to get the plane of the ultrasound beam below the rib cage. A helpful technique is to ask patients to bend their knees slightly to allow the physician to press the transducer flat and into the abdomen more deeply below the costal margin.
with the transducer pressed nearly flat on the abdomen and a firm amount of pressure applied in order to get the plane of the ultrasound beam below the rib cage. A helpful technique is to ask patients to bend their knees slightly to allow the physician to press the transducer flat and into the abdomen more deeply below the costal margin.  PEDIATRIC CONSIDERATIONS: Probe position under the costal margin is often uncomfortable for children. Slide the probe more caudal toward the umbilicus to reduce discomfort. It is often easier to push into the more protuberant abdomen than under the relatively recessed xyphoid process.
PEDIATRIC CONSIDERATIONS: Probe position under the costal margin is often uncomfortable for children. Slide the probe more caudal toward the umbilicus to reduce discomfort. It is often easier to push into the more protuberant abdomen than under the relatively recessed xyphoid process. Although it may be somewhat counterintuitive (as the heart is a left-sided structure), it is also sometimes helpful to move the transducer slightly to the right to use the liver as a sonographic window into the left chest. Remember that the subxyphoid window is obtained from the abdomen and the heart is in the chest and requires the ultrasound beam to be directed cephalad. One of the most frequent causes of novice sonographers being unable to obtain a subxyphoid image is that they are placing the transducer on the abdominal wall and imaging straight down (i.e., toward the back), instead of flattening the transducer against the abdomen and applying adequate pressure to image the chest cavity. Placing the scanning hand over the top of the transducer with the thumb on the indicator and pressing into the abdomen with the transducer nearly flat on the abdomen will help to avoid this tendency. If the subxyphoid scan is done as a part of the focused assessment with sonography for trauma (FAST) scan, it will be necessary to
Although it may be somewhat counterintuitive (as the heart is a left-sided structure), it is also sometimes helpful to move the transducer slightly to the right to use the liver as a sonographic window into the left chest. Remember that the subxyphoid window is obtained from the abdomen and the heart is in the chest and requires the ultrasound beam to be directed cephalad. One of the most frequent causes of novice sonographers being unable to obtain a subxyphoid image is that they are placing the transducer on the abdominal wall and imaging straight down (i.e., toward the back), instead of flattening the transducer against the abdomen and applying adequate pressure to image the chest cavity. Placing the scanning hand over the top of the transducer with the thumb on the indicator and pressing into the abdomen with the transducer nearly flat on the abdomen will help to avoid this tendency. If the subxyphoid scan is done as a part of the focused assessment with sonography for trauma (FAST) scan, it will be necessary to
increase the focus depth to completely visualize the posterior pericardial space. PEDIATRIC CONSIDERATIONS: With the relative tachycardia, it may be difficult to evaluate the pediatric heart in real time. Record video clips then play them back at half speed (an option or setting on most ultrasound machines) for easier analysis.
PEDIATRIC CONSIDERATIONS: With the relative tachycardia, it may be difficult to evaluate the pediatric heart in real time. Record video clips then play them back at half speed (an option or setting on most ultrasound machines) for easier analysis.
 PEDIATRIC CONSIDERATIONS: The heart in young children sits more in the center of the chest. Therefore the plane of the beam is directed toward the chin as opposed to the left shoulder.
PEDIATRIC CONSIDERATIONS: The heart in young children sits more in the center of the chest. Therefore the plane of the beam is directed toward the chin as opposed to the left shoulder. with the transducer pressed nearly flat on the abdomen and a firm amount of pressure applied in order to get the plane of the ultrasound beam below the rib cage. A helpful technique is to ask patients to bend their knees slightly to allow the physician to press the transducer flat and into the abdomen more deeply below the costal margin.
with the transducer pressed nearly flat on the abdomen and a firm amount of pressure applied in order to get the plane of the ultrasound beam below the rib cage. A helpful technique is to ask patients to bend their knees slightly to allow the physician to press the transducer flat and into the abdomen more deeply below the costal margin.  PEDIATRIC CONSIDERATIONS: Probe position under the costal margin is often uncomfortable for children. Slide the probe more caudal toward the umbilicus to reduce discomfort. It is often easier to push into the more protuberant abdomen than under the relatively recessed xyphoid process.
PEDIATRIC CONSIDERATIONS: Probe position under the costal margin is often uncomfortable for children. Slide the probe more caudal toward the umbilicus to reduce discomfort. It is often easier to push into the more protuberant abdomen than under the relatively recessed xyphoid process. Although it may be somewhat counterintuitive (as the heart is a left-sided structure), it is also sometimes helpful to move the transducer slightly to the right to use the liver as a sonographic window into the left chest. Remember that the subxyphoid window is obtained from the abdomen and the heart is in the chest and requires the ultrasound beam to be directed cephalad. One of the most frequent causes of novice sonographers being unable to obtain a subxyphoid image is that they are placing the transducer on the abdominal wall and imaging straight down (i.e., toward the back), instead of flattening the transducer against the abdomen and applying adequate pressure to image the chest cavity. Placing the scanning hand over the top of the transducer with the thumb on the indicator and pressing into the abdomen with the transducer nearly flat on the abdomen will help to avoid this tendency. If the subxyphoid scan is done as a part of the focused assessment with sonography for trauma (FAST) scan, it will be necessary to
Although it may be somewhat counterintuitive (as the heart is a left-sided structure), it is also sometimes helpful to move the transducer slightly to the right to use the liver as a sonographic window into the left chest. Remember that the subxyphoid window is obtained from the abdomen and the heart is in the chest and requires the ultrasound beam to be directed cephalad. One of the most frequent causes of novice sonographers being unable to obtain a subxyphoid image is that they are placing the transducer on the abdominal wall and imaging straight down (i.e., toward the back), instead of flattening the transducer against the abdomen and applying adequate pressure to image the chest cavity. Placing the scanning hand over the top of the transducer with the thumb on the indicator and pressing into the abdomen with the transducer nearly flat on the abdomen will help to avoid this tendency. If the subxyphoid scan is done as a part of the focused assessment with sonography for trauma (FAST) scan, it will be necessary to increase the focus depth to completely visualize the posterior pericardial space.
 PEDIATRIC CONSIDERATIONS: With the relative tachycardia, it may be difficult to evaluate the pediatric heart in real time. Record video clips then play them back at half speed (an option or setting on most ultrasound machines) for easier analysis.
PEDIATRIC CONSIDERATIONS: With the relative tachycardia, it may be difficult to evaluate the pediatric heart in real time. Record video clips then play them back at half speed (an option or setting on most ultrasound machines) for easier analysis.
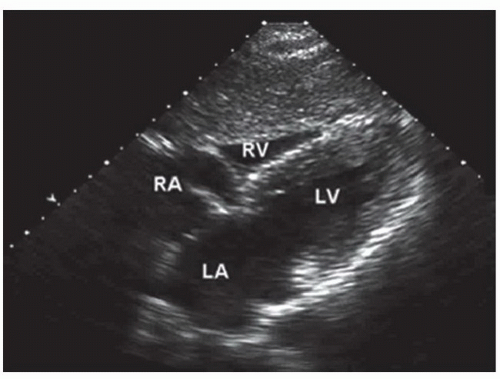
When correctly obtained, the subxyphoid view is a four-chamber image that includes the RA, RV, LA, and LV (Figs. 4.3 and 4.7;  VIDEO 4.1). The RA, tricuspid valve, and RV are somewhat anterior and to the right. The LA, mitral valve, and LV are more posterior. The apex of the LV should be anterior and to the right side of the screen (patient’s left). It may be helpful to trace the hepatic veins draining from the liver into the IVC and up into the RA. The subxyphoid view is an excellent view for pericardial effusion, which is typically seen as a significant anechoic space between the right ventricular free wall and the liver, corresponding to an inferior location of the fluid around the heart, but seen anteriorly on the screen (near the transducer). Be aware that the subxyphoid window may overemphasize the relative size of the RV if it cuts across it in an oblique plane, but overall is a good window for comparing the RV:LV ratio. The subxyphoid view is typically excellent in patients with chronic obstructive lung disease, as chest hyperexpansion moves the heart closer to the abdomen, but may be limited in patients who are obese or have other causes of abdominal distension. If the patient is cooperative, the subxyphoid view may often be enhanced by having the patient take and hold a deep breath.
VIDEO 4.1). The RA, tricuspid valve, and RV are somewhat anterior and to the right. The LA, mitral valve, and LV are more posterior. The apex of the LV should be anterior and to the right side of the screen (patient’s left). It may be helpful to trace the hepatic veins draining from the liver into the IVC and up into the RA. The subxyphoid view is an excellent view for pericardial effusion, which is typically seen as a significant anechoic space between the right ventricular free wall and the liver, corresponding to an inferior location of the fluid around the heart, but seen anteriorly on the screen (near the transducer). Be aware that the subxyphoid window may overemphasize the relative size of the RV if it cuts across it in an oblique plane, but overall is a good window for comparing the RV:LV ratio. The subxyphoid view is typically excellent in patients with chronic obstructive lung disease, as chest hyperexpansion moves the heart closer to the abdomen, but may be limited in patients who are obese or have other causes of abdominal distension. If the patient is cooperative, the subxyphoid view may often be enhanced by having the patient take and hold a deep breath.
 VIDEO 4.1). The RA, tricuspid valve, and RV are somewhat anterior and to the right. The LA, mitral valve, and LV are more posterior. The apex of the LV should be anterior and to the right side of the screen (patient’s left). It may be helpful to trace the hepatic veins draining from the liver into the IVC and up into the RA. The subxyphoid view is an excellent view for pericardial effusion, which is typically seen as a significant anechoic space between the right ventricular free wall and the liver, corresponding to an inferior location of the fluid around the heart, but seen anteriorly on the screen (near the transducer). Be aware that the subxyphoid window may overemphasize the relative size of the RV if it cuts across it in an oblique plane, but overall is a good window for comparing the RV:LV ratio. The subxyphoid view is typically excellent in patients with chronic obstructive lung disease, as chest hyperexpansion moves the heart closer to the abdomen, but may be limited in patients who are obese or have other causes of abdominal distension. If the patient is cooperative, the subxyphoid view may often be enhanced by having the patient take and hold a deep breath.
VIDEO 4.1). The RA, tricuspid valve, and RV are somewhat anterior and to the right. The LA, mitral valve, and LV are more posterior. The apex of the LV should be anterior and to the right side of the screen (patient’s left). It may be helpful to trace the hepatic veins draining from the liver into the IVC and up into the RA. The subxyphoid view is an excellent view for pericardial effusion, which is typically seen as a significant anechoic space between the right ventricular free wall and the liver, corresponding to an inferior location of the fluid around the heart, but seen anteriorly on the screen (near the transducer). Be aware that the subxyphoid window may overemphasize the relative size of the RV if it cuts across it in an oblique plane, but overall is a good window for comparing the RV:LV ratio. The subxyphoid view is typically excellent in patients with chronic obstructive lung disease, as chest hyperexpansion moves the heart closer to the abdomen, but may be limited in patients who are obese or have other causes of abdominal distension. If the patient is cooperative, the subxyphoid view may often be enhanced by having the patient take and hold a deep breath.Parasternal Long Axis (PSLA) View
The PSLA view is an outstanding window to the heart and is often complementary to the subxyphoid view. Patients with a heart that is high up in the chest or with abdominal distension often have a poor subxyphoid window, but an excellent PSLA window. Conversely, patients with hyperexpanded lungs (chronic lung disease or on a ventilator) typically have a good subxyphoid view, but lack the PSLA view.
The PSLA view is obtained with the transducer lateral to the sternum at the left fourth or fifth intercostal space  PEDIATRIC CONSIDERATIONS: As the pediatric heart lies higher in the chest, begin at the third or fourth interspace.
PEDIATRIC CONSIDERATIONS: As the pediatric heart lies higher in the chest, begin at the third or fourth interspace. And the indicator directed toward the patient’s right shoulder, keeping the ultrasound plane along the long axis of the heart (Fig. 4.4).
And the indicator directed toward the patient’s right shoulder, keeping the ultrasound plane along the long axis of the heart (Fig. 4.4).  PEDIATRIC CONSIDERATIONS: In children 3 months and younger, the heart is more midline. Better quality images can often be obtained by scanning on the right of the sternum. Subtle shifts in position (more tilting than sliding) will produce dramatic changes in image quality. The sternum provides less acoustic interference in young children, so scanning directly through the sternum may be possible.
PEDIATRIC CONSIDERATIONS: In children 3 months and younger, the heart is more midline. Better quality images can often be obtained by scanning on the right of the sternum. Subtle shifts in position (more tilting than sliding) will produce dramatic changes in image quality. The sternum provides less acoustic interference in young children, so scanning directly through the sternum may be possible. If a cardiology orientation for the PSLA view is desired, the indicator can be reversed (either on the machine or by directing the transducer indicator toward the patient’s left hip).
If a cardiology orientation for the PSLA view is desired, the indicator can be reversed (either on the machine or by directing the transducer indicator toward the patient’s left hip).
 PEDIATRIC CONSIDERATIONS: As the pediatric heart lies higher in the chest, begin at the third or fourth interspace.
PEDIATRIC CONSIDERATIONS: As the pediatric heart lies higher in the chest, begin at the third or fourth interspace. And the indicator directed toward the patient’s right shoulder, keeping the ultrasound plane along the long axis of the heart (Fig. 4.4).
And the indicator directed toward the patient’s right shoulder, keeping the ultrasound plane along the long axis of the heart (Fig. 4.4).  PEDIATRIC CONSIDERATIONS: In children 3 months and younger, the heart is more midline. Better quality images can often be obtained by scanning on the right of the sternum. Subtle shifts in position (more tilting than sliding) will produce dramatic changes in image quality. The sternum provides less acoustic interference in young children, so scanning directly through the sternum may be possible.
PEDIATRIC CONSIDERATIONS: In children 3 months and younger, the heart is more midline. Better quality images can often be obtained by scanning on the right of the sternum. Subtle shifts in position (more tilting than sliding) will produce dramatic changes in image quality. The sternum provides less acoustic interference in young children, so scanning directly through the sternum may be possible. If a cardiology orientation for the PSLA view is desired, the indicator can be reversed (either on the machine or by directing the transducer indicator toward the patient’s left hip).
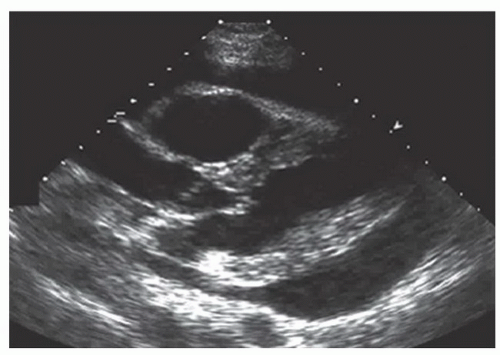
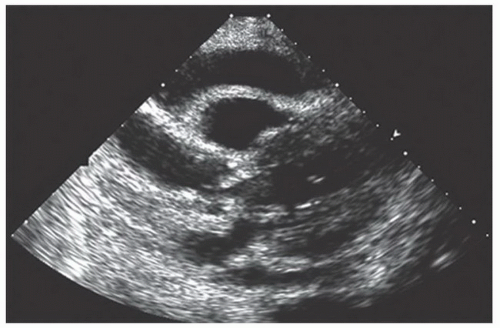
If a cardiology orientation for the PSLA view is desired, the indicator can be reversed (either on the machine or by directing the transducer indicator toward the patient’s left hip).The PSLA view typically includes the RV anteriorly, with LA, mitral valve, LV, and left ventricular outflow tract more posteriorly (Figs. 4.4 and 4.8;  VIDEO 4.2). The anterior and posterior leaflets of the mitral valve are often clearly seen, along with the accompanying chordae tendinae and papillary muscles. The aortic valve can usually be seen to open in systole. The descending aorta can be seen passing down the chest posterior to the left ventricle (Fig. 4.8). Pericardial effusions are often located posteriorly on the PSLA view (Fig. 4.9;
VIDEO 4.2). The anterior and posterior leaflets of the mitral valve are often clearly seen, along with the accompanying chordae tendinae and papillary muscles. The aortic valve can usually be seen to open in systole. The descending aorta can be seen passing down the chest posterior to the left ventricle (Fig. 4.8). Pericardial effusions are often located posteriorly on the PSLA view (Fig. 4.9;  VIDEO 4.3). As they enlarge, they may also be seen anteriorly between the RV free wall and the pericardium as well as circumferentially, and it may be helpful to tilt the transducer in order to include the apex of the heart (Figs. 4.10 and 4.11). Again, be careful to visualize the posterior (deep) pericardium as well, which may harbor an isolated effusion (Fig. 4.12). If feasible, the PSLA window may be enhanced by having the patient lie in a left lateral
VIDEO 4.3). As they enlarge, they may also be seen anteriorly between the RV free wall and the pericardium as well as circumferentially, and it may be helpful to tilt the transducer in order to include the apex of the heart (Figs. 4.10 and 4.11). Again, be careful to visualize the posterior (deep) pericardium as well, which may harbor an isolated effusion (Fig. 4.12). If feasible, the PSLA window may be enhanced by having the patient lie in a left lateral
decubitus position, allowing gravity to pull the heart from behind the sternum into a better window.
 VIDEO 4.2). The anterior and posterior leaflets of the mitral valve are often clearly seen, along with the accompanying chordae tendinae and papillary muscles. The aortic valve can usually be seen to open in systole. The descending aorta can be seen passing down the chest posterior to the left ventricle (Fig. 4.8). Pericardial effusions are often located posteriorly on the PSLA view (Fig. 4.9;
VIDEO 4.2). The anterior and posterior leaflets of the mitral valve are often clearly seen, along with the accompanying chordae tendinae and papillary muscles. The aortic valve can usually be seen to open in systole. The descending aorta can be seen passing down the chest posterior to the left ventricle (Fig. 4.8). Pericardial effusions are often located posteriorly on the PSLA view (Fig. 4.9;  VIDEO 4.3). As they enlarge, they may also be seen anteriorly between the RV free wall and the pericardium as well as circumferentially, and it may be helpful to tilt the transducer in order to include the apex of the heart (Figs. 4.10 and 4.11). Again, be careful to visualize the posterior (deep) pericardium as well, which may harbor an isolated effusion (Fig. 4.12). If feasible, the PSLA window may be enhanced by having the patient lie in a left lateral
VIDEO 4.3). As they enlarge, they may also be seen anteriorly between the RV free wall and the pericardium as well as circumferentially, and it may be helpful to tilt the transducer in order to include the apex of the heart (Figs. 4.10 and 4.11). Again, be careful to visualize the posterior (deep) pericardium as well, which may harbor an isolated effusion (Fig. 4.12). If feasible, the PSLA window may be enhanced by having the patient lie in a left lateral decubitus position, allowing gravity to pull the heart from behind the sternum into a better window.
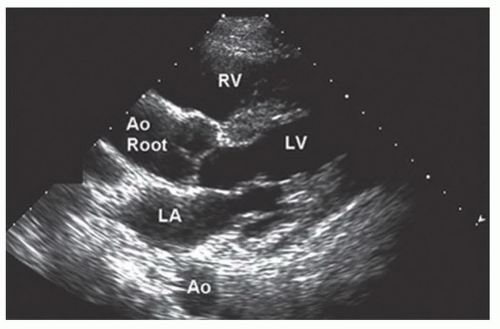 FIGURE 4.8. Parasternal Long Axis View. The aortic valve and aortic root are clearly seen. Note the descending aorta (Ao). |
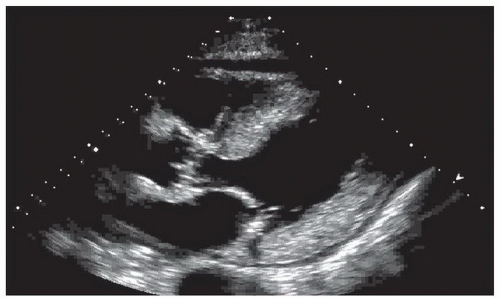 FIGURE 4.9. Parasternal Long Axis View. Small pericardial fluid is seen both posteriorly and anteriorly. |
Apical Four-Chamber View
The apical four-chamber view is typically the most difficult of the three primary windows to obtain, but also holds the most potential information (Fig. 4.5). The ability to obtain an apical view may be greatly enhanced by having the patient assume a left lateral decubitus position, allowing the apex of the heart to be pressed against the left chest. The apical view is obtained laterally at about the level of the nipple in males. In females, the transducer will frequently need to be placed lateral to and somewhat beneath the breast tissue. As in all emergency ultrasounds, the transducer indicator should be directed to the patient’s right, although this may be more toward the ceiling in a supine patient when obtaining a very lateral apical view. (Think of the direction of the indicator as wrapping around the torso.) To obtain a window, a rib interspace should be found. The transducer may need to be rotated somewhat to obtain an unobstructed view between the ribs.
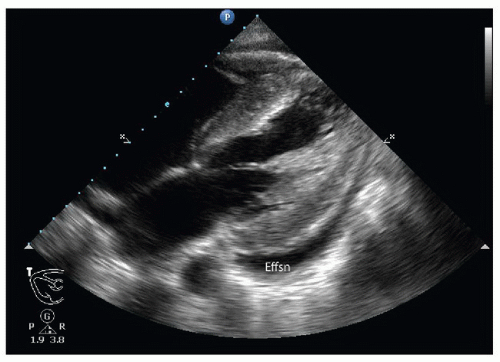 FIGURE 4.12. Parasternal Long Axis View. Predominant posterior pericardial effusion (Effsn). This is a moderate-sized effusion, but only trace fluid is seen anteriorly. |
In a properly obtained apical view, the apex of the heart is close to and near the center of the transducer face. The ventricles will be toward the face of the transducer, and the atria will be deeper. The interventricular septum should run nearly vertically down the screen, with the right-sided structures (RV and RA) on the left of the screen and the left-sided structures (LV and LA) on the right side of the screen. The tricuspid valve should be seen between the RV and the RA and the mitral valve between the LV and the LA (Fig. 4.13). A common pitfall with this approach is not being sufficiently lateral on the patient when obtaining the image, resulting in an image that appears more like a subxyphoid view, with the septum running diagonally toward the apex on the right side of the screen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree