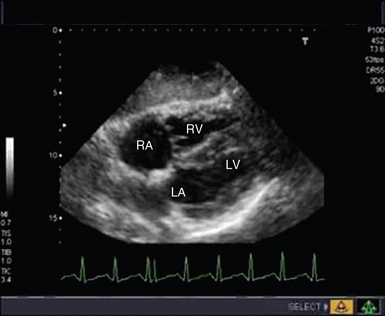
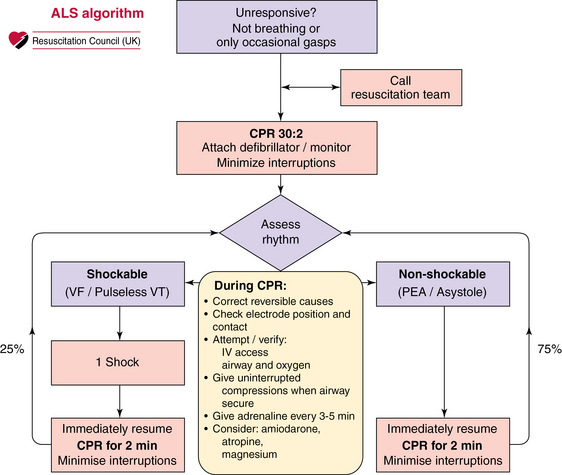
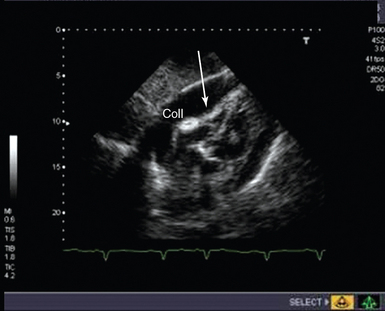
31 The incidence of out-of-hospital cardiac arrest is estimated to be 50 to 55 per 100,000 in the United States.1 When a primary electrical cause of cardiac arrest is found, definitive treatment is directed toward reversing the rhythm disturbance (cardioversion, defibrillation, pacing). When a nonelectrical cause of cardiac arrest is diagnosed (pulseless electrical activity [PEA]/asystole), practitioners are urged to exclude and treat potentially reversible causes because otherwise the outlook is poor (Figure 31-1).2 Of the reversible causes, only hypoxia, hypokalemia, hyperkalemia, and hypothermia may be diagnosed definitively with existing standard point-of-care testing. Hypovolemia, tamponade, pulmonary embolism (PE), coronary thrombosis, and tension pneumothorax are diagnosed primarily clinically and toxins by laboratory investigations. Figure 31-1 Advanced life support (ALS) algorithm. On the right side of the algorithm, in the nonshockable rhythm, the team is urged to seek and correct reversible causes of cardiac arrest. Such causes include the four H’s and four T’s: hypovolemia, hypocapnia/hypercapnia, hypoxemia, hypothermia, tamponade, thrombosis (coronary/pulmonary), toxins, and tension pneumothorax. Appropriately applied and interpreted transthoracic echocardiography (TTE) may be used to diagnose or exclude many potentially reversible causes of cardiac arrest while guiding potentially lifesaving therapeutic interventions.3 Echocardiography has been used in several studies to determine the presence or absence of cardiac activity; indeed, in some cases it has been shown to predict outcome. Moreover, echocardiography facilitates the diagnosis of true electromechanical dissociation (EMD)—the absence of effective cardiac activity despite electrical activity, which in and of itself may also determine the probable outcome of resuscitation.4 Although the American Heart Association continues to recommend that the history and clinical examination be used to direct management of PEA/asystole (low sensitivity and specificity),5 the 2010 International Liaison Committee on Resuscitation (ILCOR) guidelines suggest that ultrasound imaging may help identify reversible causes of cardiac arrest and, when appropriately trained personnel are available, should be used to assist in the assessment and treatment of potentially reversible causes of cardiac arrest.6 Traditionally, detection of cardiac output is achieved by palpation of central pulses or by noninvasive blood pressure measurement, although both these methods have been shown to be imprecise,7,8 with up to 45% of health care professionals being unable to accurately assess central pulses during cardiac arrest, which can potentially result in prolonged periods with no chest compressions and premature cessation of resuscitation.9 Periresuscitation echocardiography has not only been shown to identify the presence or absence of cardiac motion during resuscitation but can also be performed without detracting from the advanced life support (ALS) protocol.10 The potential causes of cardiac arrest that can be diagnosed with TTE include tamponade, coronary artery disease, PE, and hypovolemia. Extension of ultrasound imaging beyond the heart can be used to diagnose or exclude pneumothorax with lung views.10,11 Left ventricular (LV) end-diastolic volume has been shown to correlate well with blood loss and can reportedly be used to detect small changes in intravascular volume.12 In the critically ill, a number of parameters have been found to indicate severe hypovolemia, including the presence of a small hyperkinetic left ventricle (Figure 31-2) (and a normal right ventricle) with obliteration of the cavity at end-systole,12 an LV end-diastolic area of less than 5.5 cm2/m2 body surface area (BSA), a small inferior vena cava (IVC) with inspiratory collapse in spontaneously breathing patients,13 or a small IVC at end-expiration14 with variable respiratory changes in mechanically ventilated patients.15 Hypovolemia leading to cardiac arrest is likely to be severe, and although there is debate in the literature regarding the sensitivity and specificity of echocardiographic features of hypovolemia in the arrested state, the finding of a small, underfilled left ventricle with collapsed caval veins suggests the need for aggressive volume resuscitation and a search for the cause of the hypovolemia.16 The physiologic features of tamponade result from an increase in intrapericardial pressure causing impaired filling and an adverse effect on cardiac function. Echocardiographic features that indicate hemodynamic significance of a collection include the presence of a swinging heart, right ventricular (RV) diastolic collapse, right atrial diastolic collapse, pseudo-SAM (systolic anterior wall motion abnormality), an enlarged nonpulsatile vena cava (all parts of the respiratory cycle), reciprocal changes in the size of cardiac chambers, and transvalvular flow that varies with respiration.17 Demonstration of these echocardiographic features of tamponade has erroneously become synonymous with the diagnosis of tamponade, which is a clinical diagnosis. In cardiac arrest, demonstration of a pericardial collection (Figure 31-3) should lead to consideration of immediate drainage since the echocardiographic features of tamponade may not be present in certain circumstances (particularly following cardiac surgery). Figure 31-3 Subcostal view of a patient with tamponade. The image taken is shown in late diastole, where indentation and collapse of the right ventricular free wall are seen (arrows). coll, Collection. It is recommended that pericardiocentesis be performed under echocardiographic guidance (class I), with success rates higher than 90% being achieved, depending on the volume and location of the collection and operator experience.18 Major complications include cardiac perforation, pneumothorax, coronary perforation, trauma to abdominal organs, and death, but the incidence of complications is significantly reduced with echocardiographic guidance.18
Echocardiography in cardiac arrest
Overview
Echocardiography for the diagnosis of cardiac arrest
Echocardiography and the underlying cause of cardiac arrest
Hypovolemia
Tamponade and pericardiocentesis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Echocardiography in cardiac arrest