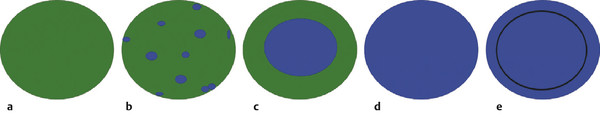
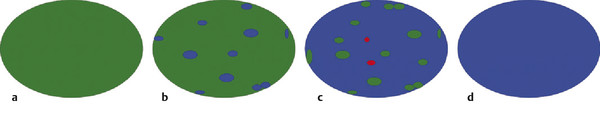
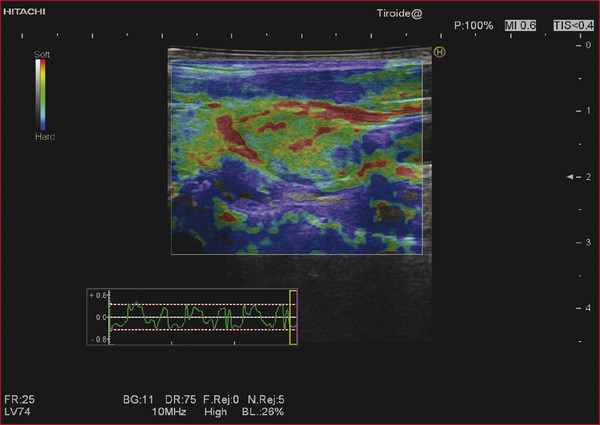
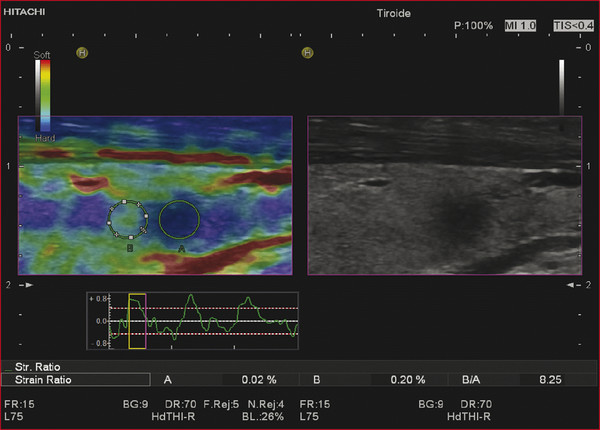
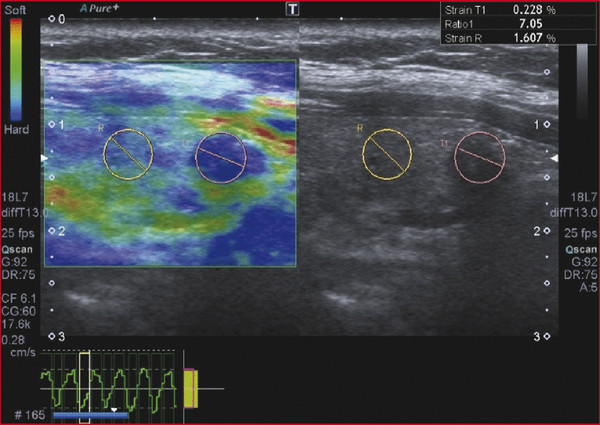
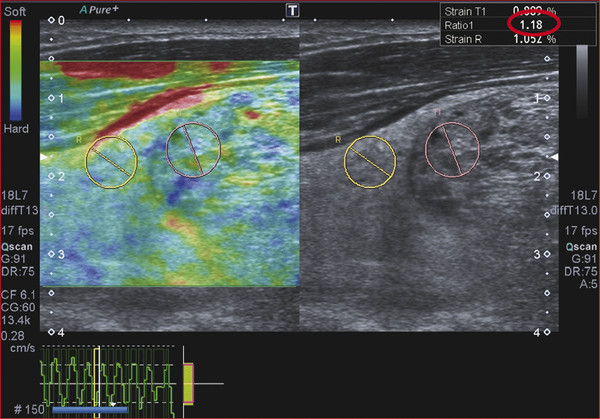
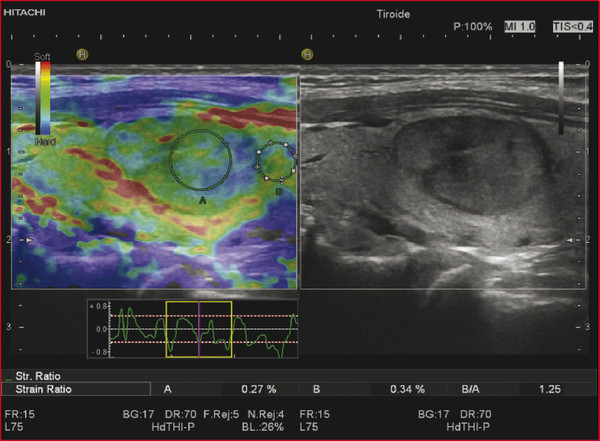
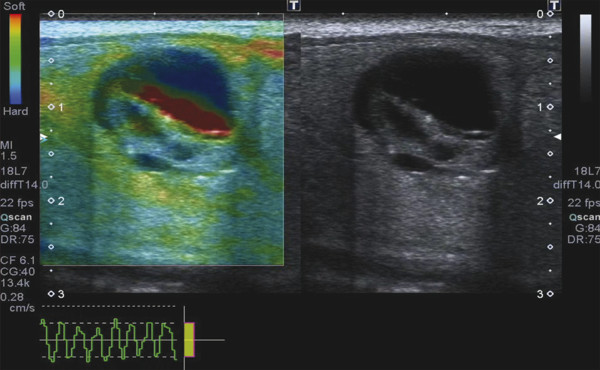
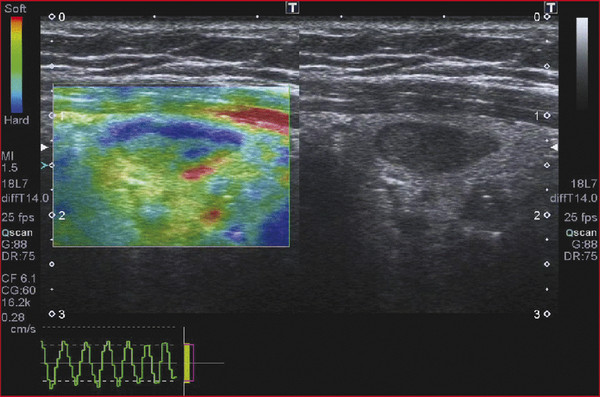
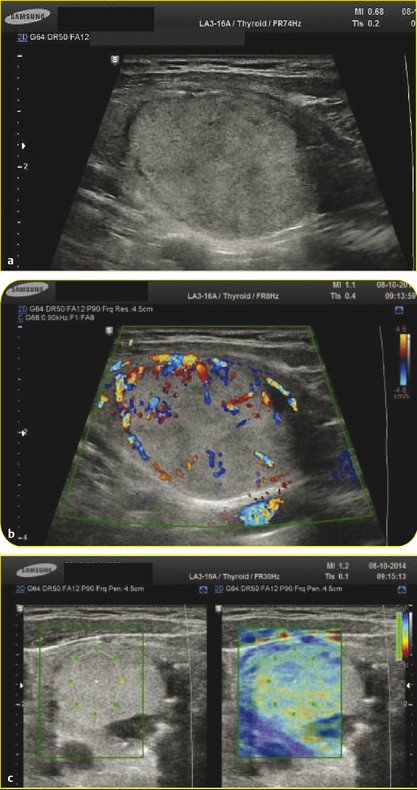
Strain Elastography Imaging Today strain elastography (SE) is the elastography method most widely available in ultrasound equipment for thyroid evaluation. SE may be performed on longitudinal or axial planes. However, some authors note that transverse (axial) scans through the thyroid are more susceptible to interference from carotid pulsations19 and, therefore, are less suitable for SE utilizing external force, In these cases, longitudinal scans are preferred, as they are less susceptible to carotid pulsations and they also offer more thyroid gland for reference tissue. Usually a color-coded map of elastographic information indicating relative tissue stiffness is superimposed on the grayscale B-mode image, in what is called real-time SE. The map can also be displayed side-by-side with the B-mode image (twin view). If the elastographic data is displayed using a grayscale map, it is important to turn off the grayscale B-mode image on which it is superimposed, otherwise evaluation is difficult. Nowadays, the offline variants of SE are less used and real-time SE is provided by most manufacturers. In the elasticity color map, or elastogram, the relatively stiffest structures, usually malignant nodules (with lowest elastic strain or no strain) are displayed in blue or red depending on the color scale used, while the soft, most-deformed tissues (with higher elastic strain) in red or green or blue. Some confusion has arisen because of the different color-coding systems selected by different manufacturers. However, lately, most manufacturers display stiff tissues in blue, soft tissues in red, and the intermediate tissues in green and the array of hues in between. The examiner should keep in mind that the default color scale of the machine can be customized by the user. Most SE systems provide a color bar or scale to allow the user to optimize the amount of external compressive force applied for optimal imaging on that system. The mechanical force in some variants of SE is applied internally— the physiologic pulsations of the carotid artery that offer sufficient displacement of the thyroid against the trachea. SE allows for a qualitative and a semiquantitative assessment of elasticity. Scoring systems based on the predominant color pattern of the lesion with 4- or 5-point scales have been proposed as an attempt to standardize SE interpretation . Note that there are various default color scales used by manufacturers, some with blue as stiff and some with red as stiff. It is important to include the color scale when viewing images. In this chapter we will use blue as stiff and red as soft unless otherwise stated. On SE, classic benign nodules present as soft, represented in the elastogram as red or green, and nodules suspicious for malignancy present as hard (high stiffness), represented in the elastogram as a pattern of blues or mostly blues (stiff).20,21,22,23,24 Subjective scoring of the predominant color in a nodule, which originated from breast nodule research and has been adopted for the thyroid, uses the breast elastography scale of Itoh et al (▶ Fig. 6.1, ▶ Fig. 6.2)25,26 or a similar scoring (which follows) for thyroid devised by Rubaltelli et al:23: Fig. 6.1 Qualitative strain elastography scores: criteria according to Ueno et al applied to thyroid by Rago et al. (a) A score of 1 indicates even elasticity in the whole nodule. (b) A score of 2 indicates elasticity in a large part of the nodule. (c) A score of 3 indicates elasticity only at the peripheral part of the nodule. (d) A score of 4 indicates no elasticity in the nodule. (e) A score of 5 indicates no elasticity in the nodule or in the area showing posterior shadowing. Fig. 6.2 Qualitative strain elastography scores: criteria according to Ito et al applied to the thyroid by Asteria. (a) A score of 1 indicates elasticity in the whole examined area. (b) A score of 2 indicates elasticity in a large part of the examined area. (c) A score of 3 indicates stiffness in a large part of the examined area. (d) A score of 4 indicates a nodule without elasticity. Score 1: homogenously soft Score 2: heterogenously soft (▶ Fig. 6.3) Score 3A: mixed with peripheral stiff areas Score 3B: mixed with central stiff areas Score 4: homogenously hard (▶ Fig. 6.4) For the Rubaltelli scale, scores of 1 and 2 are characteristic of benign nodules, and scores of 3 and 4 are characteristic, of malignant nodules, with higher scores having a higher probability of malignancy.23 Fig. 6.3 SE of benign thyroid nodule with a score of 2 according to the scale of Asteria. Fig. 6.4 Strain elastography of a malignant thyroid nodule that appears hard, with a strain ratio of 8.25 (in the malignant range). With the Ito scale, scores of 1 and 2 are classified as suggestive for benignity, and higher scores, suspicious for malignancy. Other authors have found that assigning benignity to the score 3 further increases the specificity of the method for cancer detection.27 Most authors using the Itoh scale consider hard—a score of 4 or 5—suggestive of malignancy, and soft—a score of 1 to 3—suggestive of benign nodules. Neither of the scoring systems appears to be superior. The subjectively determined score combined with the operator-dependent freehand compression may contribute to interobserver variability.20,28,29 Semiquantitative measurements can be obtained by comparing the stiffness of the nodule to that of normal thyroid or muscle. The calculation of a strain ratio (SR) is obtained by placing a region of interest (ROI) in the normal thyroid parenchyma and a ROI usually on the nodule or any area of the thyroid under investigation. A strain ratio (SR) is generated in real-time by the device or offline by dividing the strain of the normal thyroid parenchyma by that of the nodule.20,30,31 It is important that the two ROIs be at the same or similar tissue depths, with a difference of less than 10mm, in order to obviate the effects of strain decay.19 The SR evaluation does not directly represent the elasticity (i.e., Young’s modulus) due to an array of technical reasons, (mainly the difficulty of measuring the amount of the applied stress with the freehand techinique),19 but it does measure how much stiffer the lesion is than normal thyroid. The published papers to date, with some variation depending on the techniques used, show different cutoff values of SR ranging from 220 to 432,33,34 with low values assigned to benignity and values above the cutoff suggestive of cancer (▶ Fig. 6.4, ▶ Fig. 6.5, ▶ Fig. 6.6, ▶ Fig. 6.7). Fig. 6.5 Strain elastography of a papillary carcinoma. The lesion appears blue (hard) with strain ratio of 7.05, thus consistent with its malignant nature. Fig. 6.6 Strain elastography of follicular hyperplasia. The lesion presents with elastographic score 2, with a strain ratio less than 2. Thus it is a benign lesion. Fig. 6.7 Strain elastography of a benign thyroid nodule that appeared soft, with a strain ratio of 1.25. This corresponded with a final histological diagnosis of a benign nodule. For the carotid artery pulsation SE, a semiquantitative measure similar to the strain ratio, called the elasticity contrast index (ECI), is calculated.35 In this techinique, the transducer is held still, with slight contact with the skin over the thyroid. The thyroid vibrates because of carotid artery pulsations as the sole strain inductor, while the operator holds the probe in the transverse scan plane over the thyroid, gently and motionlessly. The systolic expansion of the carotid artery compresses the thyroid against the trachea with consequent anteroposterior expansion that is detected and used for strain measurements. US signals in pre-and postcompression are tracked and strain images are generated.20,36,37 A ratio of the strain near the carotid artery (a high strain area) divided by the thyroid nodule strain, called the thyroid stiffness index (TSI) or the elasticity contrast index (ECI), is calculated.20,38,39,40,41 To maximize the efficacy, the software compares the highest strain near the carotid artery with the lowest strain in the nodule. Whatever color-coding is selected, it is important to bear in mind that what is displayed is a representation of the relative stiffness of the tissues in the field of view (FOV) and that SE is by no means capable of measuring absolute values of strain. The measured strain is dependent on the amount of compression, which is always variable in SE. Nowadays, most of the manufacturers provide a real-time quality-assessment indicator during the compression, such as a numeric scale or an elasticity bar, color bar, or cycle-compression bar. By these means the operator obtains a feedback in real-time, whether his compression has reached a range estimated as reliable or if it is advisable to repeat it. Some authors advocate that three different measurements of the SR should be taken and their average should be considered for elasticity assessment.27,41,42 The ROI for elasticity evaluation in SE should ideally be placed as close as possible to the transducer, as strain diminishes with distance from the transducer. However, the ROI must include the whole nodule and a portion of the surrounding thyroid parenchyma, with some authors advising 5mm or more of parenchyma around the borders of the nodule.43 The normal parenchyma is required in the ROI as it serves as the normal reference tissue, whose elasticity is required along with that of the nodule for calculating the strain ratio. The carotid artery and hard tissues, such as muscles and the trachea, should be not be included in the ROI as they notably alter the contrast and the displayed scale of the SE image. During the examination, the patient is asked to extend the neck and stay still without breathing and swallowing for as much time as he or she can. A good quantity of coupling gel is needed for assuring slight skin contact of the transducer. The B-mode focus is positioned at the nodule level or slightly below. An elasticity image scale preset for the thyroid must be used. If not available, some modifications of the displayed elasticity scale may be needed for a correct representation of the thyroid parenchyma and nodule elasticity in the image. The operator applies light freehand compressions in a regular repetitive manner and the quality of these compressions is checked with a graphic scale of quality or numerical values on the screen, depending on the equipment manufacturer. Operator experience is required for a good compression technique. The strain measured depends on amount of compression, and, for correct strain measurements, slight and uniform compressions are needed. Calcifications inside a nodule, being very stiff, alter stiffness measurements and may make the nodule appear as stiff. On the other hand, the presence of colloid and cystic fluid also impair stiffness assessment.21,29,44,45 The elastography signal inside a cyst is essentially noise due to fluid movement during compression; the result is low-quality strain estimates.17,20 Thus, if the ROI is placed in a mixed solid and cystic area, the strain measurement is altered. It has been shown that experienced operators have greater specificity in their results than those without experience.46 The pressure of the freehand of different radiologists is difficult to standardize and strain variations due to changes in the amplitude and velocity of compression are unavoidable.20 Nonuniform compressions produce intraobserver and interobserver variability.28 For all elastographic methods, the fact that tissue becomes stiffer as it is stressed by focused compression is an important factor: precompression can result in misleadingly high stiffness readings, especially in superficial tissues.20,45,47 The color-coded scoring systems involve subjectivity in evaluation, as seen by the wide variability of performance of SE in different literature reports.28,29,35 Isthmic nodule evaluation with SE is limited in efficacy, as these nodules are compressed between the transducer and the trachea, both hard structures, and with very little normal thyroid, which is necessary as it serves as reference tissue. Carotid artery pulsations adjacent to the thyroid induce deformations in the thyroid that interfere with the freehand compression-release and degrade the strain measurements. This effect is more pronounced with nodules that are adjacent to the carotid artery, especially those that are positioned anterior to the carotid artery, which suffer more from the interference of the carotid pulsation in RTSE evaluation. Thyroid nodules deep in the posterior thyroid are subject to impaired transmission of compression and so experience less strain, which may make them appear artifactually stiff.48 The qualitative visual evaluation of color-coded elastograms is impaired mainly by subjectivity due to operator experience, but also by a certain amount of mottled noise. In SE, error in the estimation of tissue displacement leads to noise in the elastogram.48 These areas of the elastogram, where accurate strain values cannot be computed, are not color-coded. Noise in elastogram brings about a further increase in the interpretation subjectivity.20 The added time needed to complete the elastography evaluation after the ultrasound examination is variable with the different techniques.20 The limitations of qualitative SE also apply to strain ratio SE. Further, in situations where the thyroid nodule or multiple nodules are so large that they occupy the whole thyroid lobe, there may not be enough normal thyroid left in the scan for placement of the second ROI to calculate the strain ratio. Also thyroid tissue outside a nodule may not be normal but may present with multinodular goiter or lymphocytic thyroiditis, both conditions with a hard tissue consistency that would alter the strain ratio.20 These limitations also apply to SE with carotid artery pulsations. One study found that stronger pressure with the freehand altered results, thus light and uniform compression for all measurements is important.33 To summarize, the literature; the above-mentioned limitations; the many and different technological solutions of SE; and the variable scoring systems, values, and cut-off points make results less comparable and to a certain extent, difficult to assess for validity.51 RGB (red-green-blue), or the three-color layer artifact, may appear in the elastograms of cystic lesions from some systems,50,51 while the bull’s eye artifact can be seen in others52 (▶ Fig. 6.8). In mixed lesions, we also found a so-called rainbow sign (▶ Fig. 6.9). Fig. 6.8 Example of red-green-blue (RGB) sign in a cystic lesion. Fig. 6.9 Strain elastography of a FNAC proven thyroid indeterminate nodule (at cytology), which after surgery/at histology was diagnosed as hyperplasia. At qualitative evaluation, the lesion showed the rainbow sign, which can be assigned to score 2 according to Asteria. During the free hand compression, the nodule can slip out of the US imaging plane and the operator does not have the lesion in the elastogram, or has only part of it. This can be corrected by performing the compression right on the lesion, i.e., in the right plane, moving the patient into a different and more stable position, with the chin slightly up on the opposite side, and also asking the patient to hold his breath. Although SE is reported to have high accuracy, as the number of studies, patients, and nodules have increased, more cautious results and suggestions for thyroid SE have emerged. There may be a preselection bias in these studies as some evaluate all patients with nodules while others evaluate a selected group of patients who had a high probability of malignancy based on B-mode findings. Over time, some studies achieved lower sensitivities and positive predictive values around 80%,27 but high to very high negative predictive values remain common to all studies, some reaching 99%.19 Most authors used SE with scoring for their qualitative analysis, which was an attempt towards systematization of the SE method for reading elastograms; however, as reported in different studies,23,44,53,54 scoring did not offer a high and reproducible performance, and its utility has become a subject of debate.55 The discrepancies in performance of SE may also be related to the imperfection of the reference gold standard (fine needle aspiration biopsy [FNAB]) used in most studies, and only a few studies have used postsurgery histology as a reference standard.56 In a meta-analysis, 8 studies of qualitative SE, selected on the basis of a high rating in quality assessment, with a total of 639 thyroid nodules, were analyzed.57 For the diagnosis of malignant thyroid nodules with elastography, the overall mean sensitivity of the 8 studies was 92% (95% confidence interval [CI], 88–96%) and the overall mean specificity was 90% (95% CI, 85–95). A significant heterogeneity was found for specificity in the different studies. Furthermore, the patient population was highly selected with a 24% prevalence of malignancy, which does not reflect typical clinical practice. The encouraging initial results of qualitative SE were challenged by conflicting reports.46,58 In a large retrospective study26 of 703 nodules (217 malignant), SE was assessed with two different elastogram scoring systems. The results showed inferior performance of SE (sensitivity 65.4%, negative predictive value [NPV] 79.1%), compared with grayscale B-mode features in combination (sensitivity 91.7%, NPV 94.7%), so the authors concluded that elastography was not useful in recommending for fine needle aspiration cytology (FNAC). Similarly, another study,58 based on 237 thyroid nodules (58 malignant), reported lower performance of SE in comparison with grayscale B-mode ultrasound. On the contrary, a recent study59 found good accuracy of SE (84%, odds ratio (OR) 29) in a cohort of 132 thyroid nodules with 40 malignancies. With regard to qualitative SE, a review and systematic meta-analysis based on Asteria’s classification60 applied in 20 studies including thyroid nodules was published. Pooled results of elastography showed a summary sensitivity of 85% (95% CI, 79–90%) and specificity of 80% (95% CI, 73–86%). The respective pooled negative predictive and positive predictive values were 97% (95% CI, 94–98%) and 40% (95% CI, 34–48%), respectively. The authors concluded that qualitative elastography has a fair specificity and sensitivity for diagnostic accuracy. Its major strength is the detection of benignity, especially when only completely soft nodules qualify as benign. The outcome of their analysis (pooled NPV 97%) shows that fine needle aspiration could safely be omitted in patients referred for analysis of their thyroid nodule when elastography shows it to be completely soft. This could prevent unnecessary invasive diagnostic procedures in a substantial portion of patients. When combined in a single evaluation, the elastographic and B-mode ultrasound findings improved diagnostic performance, as shown by two additional studies61,62 that demonstated increased sensitivity and negative predictive values. The multicenter study of Trimboli et al62 with 498 nodules observed added value for B-mode ultrasound when combined with qualitative SE, reporting increased sensitivity for malignancy detection and a better selection of nodules needing cytology evaluation with FNAC. In comparison with the contradictory results of qualitative SE in identifying malignancy, consistently improved results seemed to be obtained with semiquantitative SE. A study27 found that in benign nodules, SR was 2.59 ± 2.12 and in malignant ones 9.10 ± 7.02. In another more recent study64 on 97 patients using the Q-elastography technique (Toshiba) for the prediction of malignancy and with a SR cutoff value ≥ 2, sensitivity, specificity, positive predictive value (PPV), and NPV of 97.3%, 91.7%, 87.8%, and 98.2%, respectively, were obtained. Wang et al45 found the best SR cutoff value for suspicion of malignancy with different strain elastographic techniques was 3.79 with 97.8% sensitivity and 85.7% specificity. The area under the curve for the strain ratio was 0.92, whereas that for the 4-point scoring of real-time strain elastography (RTSE) was 0.85. For grayscale B-mode ultrasound features, microcalcification had the highest area under the curve, 0.72. Ding et al31 reported the best SR cutoff points of two evaluations were 3.5 (82% sensitivity, 72% specificity) and 4.225 (81% sensitivity, 83% specificity). However, at least one study found low accuracy for SR evaluation. Another study (conducted on a different machine) found that adding SR to the color-scale classification results does not improve the diagnosis; on the contrary, the association of the two brought about a lower diagnostic efficacy.19,63,64 Even more recently with the respect to the use of SR in diagnosis of malignancies, two comprehensive meta-analyses were published. In the first meta-analysis, published by Razavi et al,65 both qualitative (elasticity score) and SR results were provided. In the paper, relevant information on more than 2624 patients and 3531 thyroid nodules (927 malignant and 2604 benign) in 24 studies were provided. Six ultrasound features (echogenicity, calcifications, margins, halo sign, shape, and color Doppler flow pattern) were compared with the elasticity score and strain ratio. The respective sensitivities and specificities were as follows: elasticity score, 82% and 82%; strain ratio, 89% and 82%; hypoechogenicity, 78% and 55%; microcalcifications, 50% and 80%; irregular margins, 66% and 81%; absent halo sign, 56% and 57%; nodule vertical development, 46% and 77%; and intranodular vascularization, 40% and 61%. They showed and confirmed that elastography appears to be both more sensitive and specific than each of the ultrasound features in thyroid nodule differentiation. In a more recent study, Sun et al66 performed a meta-analyses extending the previous meta-analysis to assess the diagnostic power of elastography in differentiating benign and malignant thyroid nodules using elasticity scores and SR assessment. A total of 5481 nodules in 4468 patients for elasticity score studies and 1063 nodules in 983 patients for SR studies published up until January 2013 were analyzed. The overall mean sensitivity and specificity of elastography for differentiation of thyroid nodules were 79% for elasticity-score assessment and 85% and 80% for strain-ratio assessment, respectively. The areas under the curve for the elasticity score and strain ratio were 0.8941 and 0.9285. Another issue is the role of SE in the evaluation of thyroid nodules of indeterminate FNAC.43,52,53 In two studies67,68 SE was reported as an accurate tool for the evaluation of nodules with indeterminate or nondiagnostic cytology and therefore potentially useful in selecting patients who are candidates for surgery. However, these results were not confirmed in another study that suggested the need for quantitative analytical assessment of nodule stiffness to improve SE efficacy.69 A meta-analysis of qualitative SE published by Trimboli et al62 achieved an area under the curve of 0.77 and concluded that SE has suboptimal diagnostic accuracy to diagnose thyroid nodules previously classified as indeterminate. They advised further studies using other elastographic approaches and using combined RTSE and B-mode ultrasonography. More recently, Cantisani et al reported better results with an accuracy of 89.8% by using strain ratio SE.55 Freehand elastography (i.e., manual probe-mediated compression of the tissue) has intrinsic limitations related to the experience on the operator, the conformation of the patient’s neck, and carotid artery pulsation. All these factors may influence the acquisition results. Operator experience also influences the assignment of elasticity scores using color scales, thus failing to insure objective and reproducible elastogram interpretation, and so, score assignment. An early study focused on interobserver agreement of SE published by Park et al28 reported no or poor interobserver agreement with the use of the Itoh scale for scoring. Subsequent studies reported good results for the SE 4-point scale with almost perfect interobserver agreement47,59,70,71 and good intraobserver agreement.72 One study found the interobserver agreement with use of the 4-point scale better than that with the use of the Thyroid Imaging–Reporting and Data System (TI-RADS) score.71 Given the availability of scoring scales with 3 steps up to 6 steps, some authors advocate the use of simple scoring systems to obviate the interobserver variability.19 An attempt to develop an even more reproducible method of evaluation to use the strain ratio.73 However, even in this case, the selection of the ROIs for calculating the SR is manual and may lead to error. A learning curve and experience influence the interobserver and intraobserver agreement, but when a standardized protocol is used in making compressions and selecting ROIs, the results were very good.20,73 Most papers showed no dependency of the elasticity assessment score on the nodule size.20,24,44,71,74 However 2 studies had worse performance of SE with nodules < 1 cm in comparison with nodules > 1 cm26,34 and 2 other studies reported unacceptable accuracy of qualitative SE for nodules < 5mm.44,75 On the contrary, a study45 with 51 small solid nodules of 3 to 10mm suggested that SE seemed to be useful even in small nodules: sensitivity 91%, specificity 89%, PPV 94%, and NPV 85%. Nodules >3.5 cm have been reported not to be suitable for SE evaluation as they are larger than the possible ROI.41,76 Papillary carcinoma and its variants are the most common thyroid malignancies; the second most common histology is follicular carcinoma. A number of studies have documented that SE cannot differentiate follicular carcinoma from benign nodules44,47,51,79,70,76 as it presents as elastic in almost half of the cases. In Bojunga et al’s meta-analysis,57 the authors’ remark that most malignant nodules missed by elastography were follicular carcinomas, which can be soft and difficult to differentiate from benign nodules. Furthermore, medullary, nondifferentiated, and metastatic carcinoma can also present as soft and cannot be diagnosed with elastography.53,76 However, another study74 found SE to be useful for predicting malignancy in nodules with nondiagnostic cytological findings by analyzing 101 patients with at least one indeterminate nodule. The authors reported a better performance of SE than ultrasound and the potential capability of SE for reducing unnecessary surgery. Cystic areas produce artifacts at elastography, and evaluation of mixed cystic and solid nodules should be focused on the solid areas, whose small dimensions may not be suitable for elasticity assessment. Also when part of a nodule consists of benign tissue and the other portion is malignant, evaluation with elastography is difficult. A study showed that a microcarcinoma (< 10mm) in a very hard nodule with score 4 or 5 has a predilection to extrathyroid extension,77 although another study did not find an increased risk of neck lymph node metastases in such type of nodules.78 With freehand SE, it is not possible to have equal compression–release cycles and to maintain exactly the same initial compression, and these variabilities confer variation in the strain and in the elastographic image.20,28,35,76 Therefore complying with the quality indicator on the screen while executing freehand compression is crucial for an accurate evaluation of elasticity. Experience is needed for performing compression–release cycles that lead to reproducible and reliable elasticity readings. A study report claims that for liver elastography, an operator with experience of over 500 examinations produces better results.79 However, to date, only one study evaluated the learning curve in the thyroid setting, showing a very steep learning curve, with constant and reproducible results after only 7 patients.80 Out-of-plane motion of the nodule during the compression–release cycles can impair strain measurements. Some manufacturers offer combined autocorrelation methods to address this issue.19 Because SE displays the relative strain of the tissues (in comparison of one against the other in the field of view) in color-coded elastograms, it is important to select a field of view (FOV) large enough to include healthy thyroid tissue, which serves as the standard for normal thyroid tissue strain. On the other hand, for nodules with an anterior position in the gland, the strap muscles should be left out of the FOV due to their stiffness, as they alter the measure of relative strain in the elasticity image; a malignant nodule may appear as soft (relative to the stiff strap muscles). Another fact is that the strain values obtained during elastography can cover a very large range of values, much larger than the low range that can be displayed on a color-coded elastogram.49 For this reason, an elastogram whose range of values has been optimized for a rather soft material will not display the variations in hard materials such as nodules and cancers well. Therefore, customization of the display scale according to the stiffness of the material under investigation is needed to obtain quality elastograms.49 On the contrary, a strain ratio considers in the computation the full range of strain values and therefore may be more accurate. See the selected studies results in ▶ Table 6.1 and ▶ Table 6.2. Study No. of nodules Sensitivity (%) Specificity (%) Reference standard Rago et al 200724 92 97 100 Surgery Asteria et al 200854 86 94 81 FNAB or surgery Tranquart et al 200881 108 100 93 FNAB Hong et al 200944 145 88 90 Surgery Rubaltelli et al 200923 51 82 86 FNAB or surgery Lippolis et al 201169 102 89 6 Presurgery of indeterminate cytology (follicular) Moon et al 201278 703 65 58 FNAB or surgery Azizi et al 201382 912 80 70 FNAB or surgery Ko et al 201346 367 89 81 FNAB or surgery Mehrotra et al 201383 146 90 79 FNAB or surgery Ragazzoni et al 201259 132 85 83 Surgery Razavi et al 201365 3531 82 82 FNAB or surgery Nell et al 201560 3908 79–90 73–86 FNAB or surgery Sun et al 201566 5481 79 85 FNAB or surgery Abbreviation: FNAB, fine needle aspiration biopsy Study No. of nodules Sensitivity (%) Specificity (%) Reference standard Dighe et al 200836 62 100 79 FNAB or surgery Cakir et al 201132 391 73 70 Surgery Cantisani et al 201263 97 97.3 91.7 Surgery Razavi et al 201365 3531 89 82 FNAB or Surgery Cantisani et al 201473 354 93 92 FNAB or Surgery Sun et al 201466 54–81 85 80 FNAB or Surgery *Dighe et al used carotid artery compression strain elastography. Abbreviation: FNAB, fine needle aspiration biopsy. This technique, also called in vivo carotid artery compression elastography, may provide, depending on the equipment, a thyroid stiffness index, or systolic thyroid strain index, (TSI) and an elasticity contrast index (ECI). The TSI requires a FOV placed in axial direction, covering both the nodule and the carotid artery. The software calculates a ratio (TSI): the strain of the carotid artery, which is very stiff, divided by the lowest strain inside the nodule.19,36,38,84 Among the few reports in the literature involving internal quasi-static SE is a significant study that obtained the value of TSI (called in this study, systolic TSI) of benign nodules at 6.82 ± 3.54 and 18.43 ± 5.99 in the malignancies, with a cutoff value of 10 yielding best performance,20,38 with sensitivity of 100% and specificity of 79.5%. The elasticity contrast index (ECI, or SR) method, called Elastoscan (Samsung), again uses a quasi-static, steady-state physiologic excitation technique based on carotid pulsations to induce the strain.19,35,85 The software measures the strain in a FOV that includes the nodule and adjacent normal thyroid. Thereafter, strain differences in the FOV are represented as a color-coded map and an elasticity contrast index is computed which is high for malignancies and low for benign nodules.19,36,81. The operator holds the transducer in transverse scan, with only minimal pressure and waits to obtain a steady state, while the quality of the technique is shown by a scale indicator on the screen.81 The operator then draws a FOV that comprises the nodule and some tissue around it or is located only within the nodule (▶ Fig. 6.10).81 Some authors suggest that two measurements be taken with the highest one being considered for diagnosis.35,86 Fig. 6.10 Follicular adenoma. (a) At baseline ultrasound, the lesion appears isoechoic with a tiny halo. (b) At color Doppler, the nodule shows peri-intraleisonal vascularization corresponding to Pattern III. (c) Elasticity contrast index (ECI) evaluation at Elastoscan was lower than 3, and thus consistent with benignity of the lesion.
6.2.1 Technique
6.2.2 Qualitative Strain Elastography
6.2.3 Semiquantitative Strain Elastography
Strain Ratio Elastography
In Vivo Strain Elastography Using Carotid Artery Pulsation
6.2.4 Tips and Tricks
6.2.5 Limitations and Artifacts of SE
6.2.6 Interpretation of Results
6.2.7 Drawbacks of SE
6.2.8 Interpretation of Results of Internal Quasi-Static Strain Elastography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree