Elbow
Sarah Yanny
Eugene McNally
Thomas L. Pope Jr.
GENERAL CONSIDERATIONS
Radiographic Examination
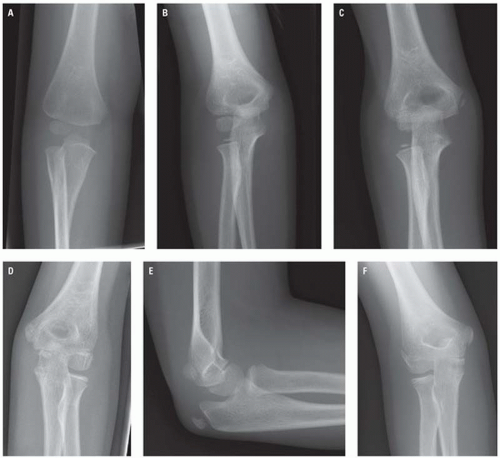
Standard radiographic examination of the elbow includes anteroposterior (AP) and lateral views (Fig. 9.1). The AP view should be obtained with the elbow fully extended, the forearm fully supinated (if possible), and the fingers slightly flexed. The central beam is directed perpendicular to the elbow joint. There should be no rotation of the forearm. The lateral view should be obtained with the elbow at 90 degrees of flexion and the forearm in a neutral position with the thumb pointing upward. The vertical central beam is centered over the lateral epicondyle of the humerus. If the limb cannot be moved, two perpendicular projections can be taken by rotating the x-ray tube.
When a fracture of the radial head, coronoid process, or capitellum is suspected, a radial head-capitellar view, a variant of the lateral view, should be obtained (Fig. 9.2). The elbow is positioned at 90 degrees of flexion, the forearm resting on its ulnar side with the thumb pointing upward, and the central beam directed at the radial head with a 45 degrees angle to the forearm.
In children, oblique projections may be useful if the routine views do not demonstrate a fracture but a joint effusion is present. Internal oblique views are valuable when humeral lateral condylar fractures are suspected. Comparison views of the other elbow should not be part of routine radiographic practice and should only be performed in exceptional circumstances.
Computed tomography (CT) may be indicated in the context of severe or complex injuries, dislocations, and foreign bodies. Magnetic resonance imaging (MRI) is useful in the detection of soft tissue and ligamentous injury, radiographically occult fractures, osteochondral injuries, and is of particular use in children to detect injury of the nonossified epiphysis. Ultrasound (US) is widely used in the context of soft tissue injuries, whether acute or chronic, and can detect intra-articular injury following trauma by demonstration of a lipohemarthrosis.
Anatomy
The elbow is a complex pivotal-hinge synovial joint with three articulations (the humeroulnar, radiocapitellar, and proximal radioulnar joints). Flexion-extension occurs mostly at the humeroulnar articulation (uniaxial joint), whereas pronation-supination occurs at the radiocapitellar and radioulnar articulations. The joint is held together by a fibrous capsule, the deep surface of which is lined by synovium. Three fat pads rest in the radial, coronoid, and olecranon fossae. They are enveloped by fibers of the joint capsule separating the fat pads from the synovial lining, making them intracapsular and extrasynovial. The articulating surfaces of the head of the radius and ulna are held together by the annular ligament. The capsule is weak anteriorly and posteriorly, but joint stability is reinforced by the medial (ulnar)
and lateral (radial) collateral ligament complexes. The flexor-pronator group of muscles originates from the medial epicondyle, whereas the extensor-supinator muscles attach to the lateral epicondyle. The ulnar nerve courses posterior to the medial epicondyle and is closely applied to the ulnar collateral ligament, passing between the heads of flexor carpi ulnaris.
and lateral (radial) collateral ligament complexes. The flexor-pronator group of muscles originates from the medial epicondyle, whereas the extensor-supinator muscles attach to the lateral epicondyle. The ulnar nerve courses posterior to the medial epicondyle and is closely applied to the ulnar collateral ligament, passing between the heads of flexor carpi ulnaris.
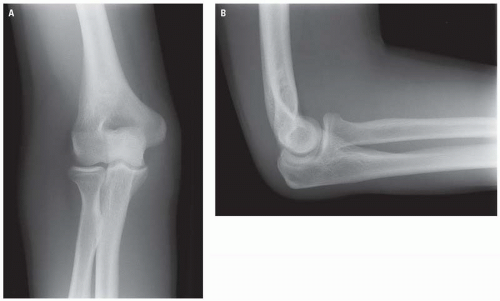 Figure 9.1. Routine radiographic examination of the elbow. Anteroposterior (A) and lateral view (B). |
Ossification of the elbow is complex. Careful and systematic assessment of the pediatric elbow is essential, particularly in the context of avulsion of the epicondylar apophyses. The distal humerus has four secondary ossification centers; those for the capitellum and trochlea, which comprise the articular surface, and those for the medial and lateral epicondyles (Fig. 9.3). The acronym “CRITOL” is often used to describe the usual order of the six ossification centers of the elbow (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, lateral [external] epicondyle). The capitellar ossification center appears at 1 to 2 years of age, the radial head at 2 to 4 years, the internal epicondyle at 4 to 6 years, the trochlea at 8 to 11 years, the olecranon at 9 to 11 years, and the lateral epicondyle at 10 to 11 years. The age at which these centers are first seen varies considerably and usually proceeds earlier in girls than in boys. The main role of CRITOL is to highlight that the medial epicondyle center should be present before the trochlea. If following trauma a trochlear center is visible and the medial epicondyle is not, a displaced medial epicondyle should be suspected.
Ununited ossification centers may persist unfused into adulthood and may be confused with avulsion fractures. The trochlea has two or more ossification centers, which may result in a fragmented appearance. The olecranon may also be very irregular during its normal development. The medial epicondyle fuses directly with the humerus, whereas the lateral epicondyle fuses first with the capitellum, then both fuse with the humeral shaft. This often causes the lateral epicondyle to appear widely separated from the humerus due to the thicker cartilaginous plate associated with it.
Landmarks
Fracture lines can be difficult to visualize after acute elbow injury, particularly in children. Important landmarks should be reviewed to confirm the adequacy of the radiograph and aid in recognition of occult signs of injury.
Anteroposterior View
A common complication of supracondylar fracture is an abnormal carrying angle. In full extension and supination, the forearm lies at 165 degrees to the
humerus (15 degrees of valgus) to clear the hips. The angle is greater in females. Various angles are measured on AP radiographs to determine the proper alignment of the distal humerus.
humerus (15 degrees of valgus) to clear the hips. The angle is greater in females. Various angles are measured on AP radiographs to determine the proper alignment of the distal humerus.
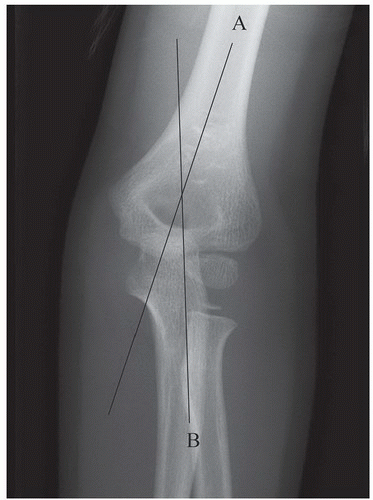 Figure 9.4. The humeroulnar angle formed between the long axis of the humerus (A) and long axis of the ulna (B). This angle most accurately depicts the true carrying angle of the elbow. |
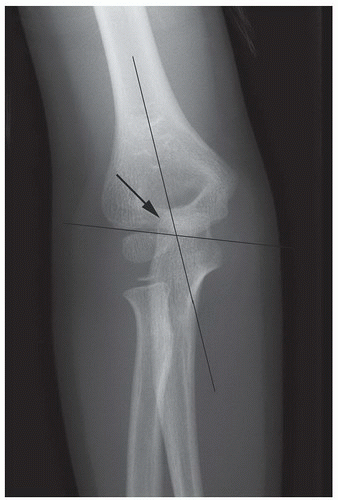 Figure 9.5. Baumann’s angle (arrow) is the angle created between the longitudinal axis of the humerus and the coronal axis of the capitellar physis. |
The humeroulnar angle is the angle formed between the long axis of the humerus and the long axis of the ulna, and normally measures 154 degrees to 178 degrees (Fig. 9.4). This angle most accurately depicts the true carrying angle of the elbow.
Baumann’s angle or the shaft-physeal angle is the angle created between the longitudinal axis of the humerus and a line through the physis of the lateral condyle (Fig 9.5), and is predictive of an acceptable carrying angle. This should measure approximately 70 degrees and within 5 degrees that of the contralateral uninjured elbow. This angle is helpful in determining the adequacy of reduction of a supracondylar fracture and may indicate varus deformity.
The metaphyseal-diaphyseal angle is formed between the long axis of the humerus and a line connecting the lateral and medial epicondyles (Fig. 9.6). This ranges from 72 degrees to 95 degrees but is the least reliable estimate of the clinical carrying angle.
Lateral View
The “hourglass,” “teardrop,” or “figure eight” sign at the distal humerus (Fig. 9.7). This is formed by the anterior margin of the olecranon fossa and the posterior margin of the coronoid fossa. The inferior portion of the teardrop should be the ossification center of the capitellum. The capitellum and trochlea should be superimposed. If not, the image is likely not a true lateral and interpretation of the remaining observations is less reliable.
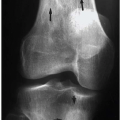
The fat pad sign. Normally on a lateral radiograph, lucency that represents fat is present along the anterior aspect of the distal humerus, and no lucency is visualized along the posterior cortex. An elevated anterior lucency—the radiographic “sail sign”—and/or a visible posterior lucency is described as a positive fat pad sign (Fig. 9.8), although this is not as specific as a positive posterior fat pad.
The anterior humeral line (Fig. 9.9). A line drawn along the anterior cortex of the humerus should intersect the middle third of the capitellum on the lateral view. Supracondylar fractures usually result in displacement of the capitellum posteriorly with resultant displacement of the anterior humeral line anteriorly.
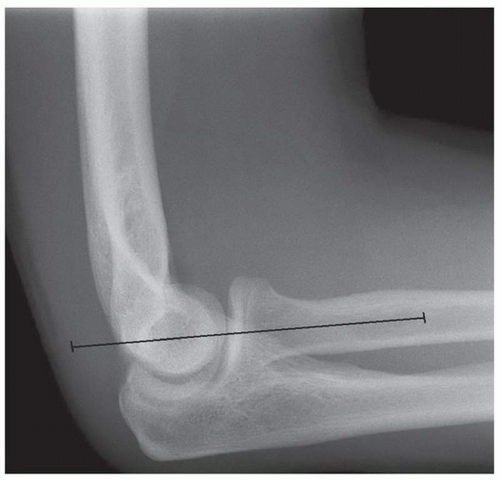
The radiocapitellar line (Fig. 9.10). A line drawn along the center of the proximal radius should normally bisect the capitellum on both the lateral and the AP elbow radiograph. Failure of alignment suggests dislocation of the radial head. This requires prompt reduction because neurovascular compromise may ensue.
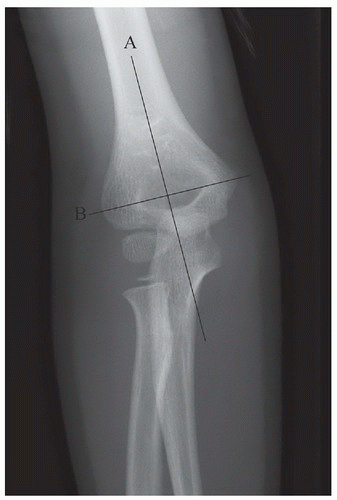 Figure 9.6. The metaphyseal-diaphyseal angle formed between the long axis of the humerus (A) and a line connecting the lateral and medial epicondyles (B). |
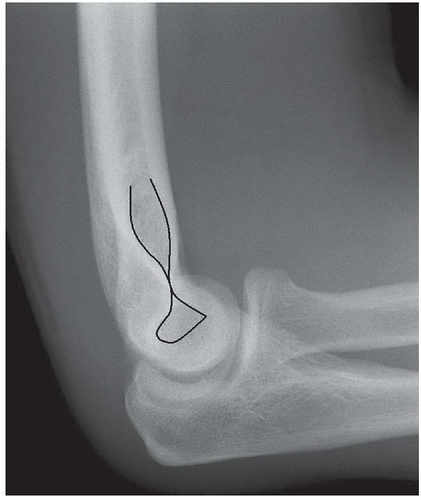 Figure 9.7. Teardrop or figure eight sign at the distal humerus. This is formed by the anterior margin of the olecranon fossa and the posterior margin of the coronoid fossa. |
 Figure 9.8. The fat pad sign. The elevated anterior fat pad and posterior fat pad are, following trauma, consistent with hemarthrosis. |
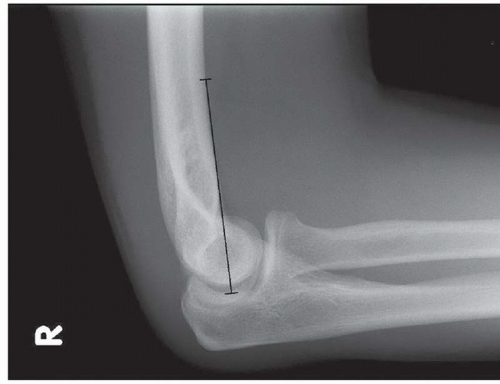 Figure 9.9. The anterior humeral line. A line along the anterior cortex of the humerus should intersect the middle third of the capitellum. |
RADIOGRAPHIC MANIFESTATIONS OF TRAUMA
Evaluation of the soft tissues is important in elbow trauma. Soft tissue swelling may often be the most obvious radiographic abnormality in the setting of subtle or undisplaced fractures. Extracapsular soft tissue swelling may be diffuse or localized, such as to the radial or ulnar borders of the elbow in fractures of the lateral condyle or medial epicondyle, respectively.
As previously mentioned, three intracapsular fat pads are present between the synovium of the elbow and the joint capsule. The anterior fat pad is a summation of the radial and coronoid fat pads, which are normally pressed into the shallow radial and coronoid fossae by the brachialis muscle during extension. The posterior fat pad is normally pressed into the deep olecranon fossa by the triceps brachii tendon and anconeus muscle during flexion and the third lies over the supinator as it wraps over the radius.
Hemarthrosis or effusion into a structurally intact joint capsule causes distention of the joint and displacement of the fat pads. A visible anterior fat pad may be normal, but if displaced anteriorly and superiorly in the presence of joint distention, it will form a triangular shape, with a convex anterior margin similar to a billowing spinnaker sail (Fig. 9.11). An atraumatic sail sign implies intra-articular fluid of an inflammatory nature (Fig. 9.12), although with chronicity, infiltration of the fat pad may obscure it. A visible posterior fat pad is always regarded as abnormal, signifying fluid in the intra-articular space. In the setting of acute trauma, an occult fracture should be sought, particularly of the radial head in adults or a supracondylar fracture in children. It must be remembered that an absent fat pad sign does not exclude a fracture. This may occur with poor positioning, capsular rupture (e.g., dislocations, displaced intra- articular fractures), or an extracapsular injury (e.g., medial and lateral epicondylar fractures).
 Figure 9.12. Advanced rheumatoid arthritis of the elbow with concentric joint space narrowing, subluxation of the radiocapitellar joint, and a moderate joint effusion. |
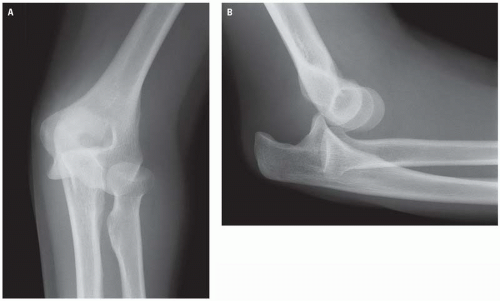 Figure 9.13. AP (A) and lateral (B) views of the elbow demonstrate simple posterior dislocation of the elbow. |
Although one of the most stable joints in the body, dislocation and fracture-dislocation of the elbow are not uncommon. Elbow dislocations are second in frequency only to shoulder dislocations in adults, and the elbow is the most frequently dislocated joint in children. Elbow dislocations are classified as simple or complex. Simple dislocations are classified according to direction of displacement of the radius and/or ulna in relation to the distal humerus, namely posterior (Fig. 9.13), poste rolateral, posteromedial, lateral, medial, or divergent. Fracture-dislocations are referred to as complex, the most common complex dislocation involving concomitant fracture of the radial head (Fig. 9.14). Complications include vascular injury, particularly in the setting of open and/or anterior dislocations, where the brachial artery is disrupted by forcible hyperextension, and neuropraxia, most commonly involving the ulnar nerve or anterior interosseous branch of the median nerve. Long-term sequelae include valgus or posterolateral instability, which may result in recurrent elbow dislocation.
PEDIATRIC INJURIES
In children, the most common elbow fractures are supracondylar (60%), lateral condylar (15%), and medial epicondylar (10%).
Supracondylar Fractures
Supracondylar fractures are the most common pediatric fractures around the elbow and have a peak incidence in the first decade of life. They are extraarticular, lying beyond the proximal extensions of the joint capsule. They occur at a potential site
of weakness in the humeral metaphysis, which is relatively under-trabeculated in children. There are two types based on the mechanism of injury. The vast majority (96%) are extension injuries. Such fractures result from a fall on the outstretched hand with the elbow hyperextended. They result in posterior displacement or angulation of the distal fracture fragment. Conversely, the rarer flexiontype fractures are usually caused by a blow to the posterior aspect of the elbow resulting in anterior displacement of the distal fragment and are potentially very unstable. Supracondylar fractures may be complete or incomplete.
of weakness in the humeral metaphysis, which is relatively under-trabeculated in children. There are two types based on the mechanism of injury. The vast majority (96%) are extension injuries. Such fractures result from a fall on the outstretched hand with the elbow hyperextended. They result in posterior displacement or angulation of the distal fracture fragment. Conversely, the rarer flexiontype fractures are usually caused by a blow to the posterior aspect of the elbow resulting in anterior displacement of the distal fragment and are potentially very unstable. Supracondylar fractures may be complete or incomplete.
 Figure 9.14. AP (A) and lateral (B) radiographs demonstrating a complex fracture-dislocation involving concomitant fracture of the radial head. |
The anterior humeral line is useful in the diagnosis of supracondylar fractures, passing anterior to the middle third of the capitellum in most cases (Fig. 9.15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree