Hand
Emma L. Rowbotham
Dominic A. Barron
Thomas L. Pope Jr.
GENERAL CONSIDERATIONS
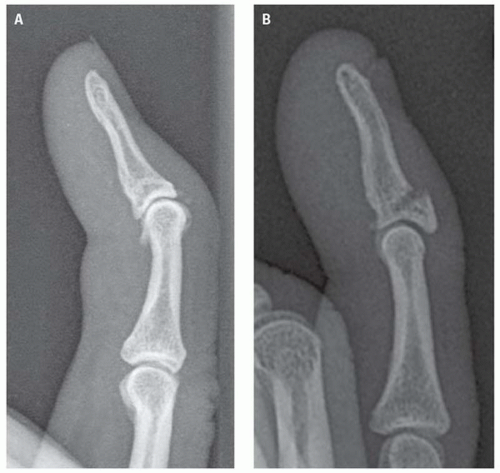
The hand and wrist are commonly considered together in the trauma setting by ED physicians, and although several systemic diseases and traumatic injuries involve both the hand and the wrist, it is important to emphasize that each is a separate anatomic region. The radiographic examination of the hand does not constitute an adequate study of the wrist, and the radiographic examination of the wrist does not constitute an adequate study of the hand. Furthermore, certain special views of the hand and wrist are particular to each and have no application to the other. Therefore, it is mandatory that the attending physician determine as precisely as possible which part is to be studied radiographically and transmit this information to the radiology department. As with all orthopedic radiology, two views of the injured region are mandatory and should be in two different planes—if this is not possible, then bony injury or dislocation cannot be excluded (Fig. 11.1A,B).
During childhood and adolescence, when the epiphyses are undergoing fusion, the extreme variability in the radiographic appearance of the physes may make interpretation of this region difficult. The mechanism, the location of the injury, the clinical findings, and the radiographic appearance of the soft tissues are all important in the radiographic evaluation of the injured part (Fig. 11.2).
The soft tissue shadows often show subtle changes, which provide valuable indirect signs related to subtle but significant bone abnormalities. The value of careful appraisal of these tissue shadows cannot be overemphasized.
IMAGING TECHNIQUES
Radiographic Examination
The optimum routine examination of the hand of patients of all ages should include PA (frontal), oblique, and lateral projections. The digits should be flexed to varying degrees in the oblique and lateral projections to eliminate superimposition (Fig. 11.3A,B). The lateral is the most difficult to interpret but is critical in the evaluation of carpometacarpal (CMC) fractures and fracture- dislocations (Fig. 11.3C).
When the clinical concern is for phalangeal injury, dedicated finger views should be taken with specific lateral views of the injured digits. These are readily obtained by having the patient flex the uninvolved digits.
The thumb requires special mention because none of the positions described affords a PA view of this digit. The frontal view of the thumb is generally obtained with the forearm placed midway between pronation and supination and with the thumb extended away from the volar surface of the hand (Fig. 11.4A-B).
Previously, special views of the hand, including carpal tunnel and reversed oblique views, were employed when the standard series of films could not answer the clinical question. These techniques are now rarely used and have largely been replaced by cross-sectional
imaging. When there is concern regarding, for example, CMC dislocation with equivocal radiography, then computed tomography (CT) is indicated.
imaging. When there is concern regarding, for example, CMC dislocation with equivocal radiography, then computed tomography (CT) is indicated.
Ultrasound
The advent of high-frequency ultrasound probes has revolutionized soft tissue imaging of the hand and wrist. Ultrasound is now increasing the imaging modality of choice in the assessment of ligaments, tendons, foreign body localization, and soft tissue pathology such as joint effusion or hematoma. This is because of the high resolution, accessibility, relatively low cost, and excellent temporal assessment that this modality provides.
Ultrasound of the hand and fingers can prove technically challenging because of the small surface area involved and relative inaccessibility of various areas. A small footprint probe is invaluable as well as a gel stand off or the use of a water bath (Fig. 11.5). These provide a good imaging window without the discomfort of direct pressure on the injured hand or fingers.
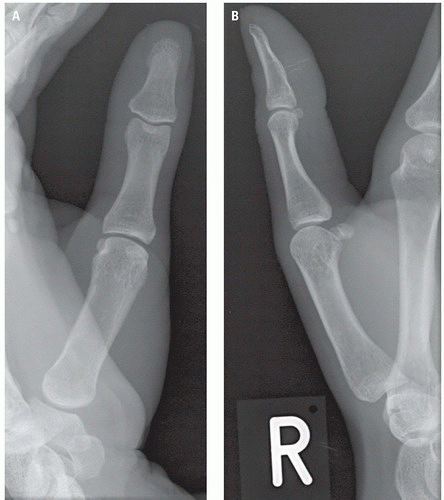 Figure 11.4. A: Normal AP view of the right thumb in an adult patient. B: Normal lateral view of the right thumb in an adult patient. |
Ultrasound also has the benefit of allowing real time and dynamic evaluation of structures, which is particularly helpful in assessment of the tendons. A further immediate advantage for the operator is the ability to compare appearances with the contralateral side to help with interpretation of any abnormal findings. Studies have been published that have shown that ultrasound may be useful in detecting fractures with signs including a break in the hyperechoic line representing the bony cortex and local hematoma.1 However, standard radiographs remain the mainstay of imaging all bony trauma, and the role of ultrasound remains an adjunct at present.
CT/MRI Uses in Trauma
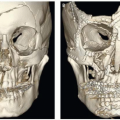
The advent of multislice CT has transformed its use for hand imaging and has an important role in the management of trauma.2 This now allows thin-slice, low-dose volumetric acquisitions of the affected areas in a short time period. The use of submillimeter acquisitions facilitates high-quality images with multiplanar and 3D reformations. These are particularly valuable across the CMC joints where they can accurately characterize the true extent of the injury or, in difficult cases, make the diagnosis.
Three-dimensional images can be particularly valuable when the angulation and rotation of the injured site is critical for surgical planning.
Three-dimensional images can be particularly valuable when the angulation and rotation of the injured site is critical for surgical planning.
Magnetic resonance imaging (MRI) is rarely employed in the investigation and management of traumatic injuries to the hand, whereas ultrasound’s superior resolution is preferred for soft tissue injuries.
RADIOGRAPHIC NORMAL ANATOMY
The locations of the epiphyses of the phalanges and metacarpals and the radiographic characteristics of the nutrient artery canals are key practical aspects of the radiographic anatomy of the hand. The phalangeal and metacarpal epiphyses are differently located, and even among the metacarpals, the location of the growth centers is not uniform (Fig. 11.2). The phalangeal epiphyses are proximally situated compared to the index, middle, ring, and little finger metacarpals that are located distally and constitute the metacarpal heads. The thumb metacarpal has its growth center at its base. Anomalous secondary ossification centers may involve the distal end of the thumb metacarpal or the base of any of the lateral metacarpals.
During childhood, when the physes are open, the epiphyseal plate should not be mistaken for a fracture line, and knowledge of the estimated age of fusion is essential when interpreting pediatric radiographs.
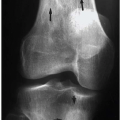
Nutrient artery canals (medullary foramen; Fig. 11.6) are located near the middle of the phalangeal and metacarpal shafts and enter the bone from each side, passing obliquely distally. The margins of these normal vascular grooves are uniformly smooth, sclerotic, parallel, and converge distally. Nutrient artery canals are not, however, constant features. When they are present, their location, course, and radiographic characteristics should distinguish them from incomplete fracture lines.
The sesamoids are small, rounded bones embedded in certain flexor tendons. Five sesamoid bones are commonly found in the hand. These include two lying volar to the thumb metacarpophalangeal (MCP) joint, one volar to the interphalangeal joint of the thumb, and one in the soft tissues anterior to the MCP joint of both the index and little fingers. Sesamoid bones are characterized by dense, smooth cortical margins and a normal trabecular pattern.
RADIOGRAPHIC MANIFESTATIONS OF TRAUMA
Knowledge of the common mechanisms of injury and their associated fracture patterns is essential when both examining a patient presenting with a hand injury and interpreting his or her radiographs. This will facilitate the appropriate imaging being performed for the suspected injury and aid diagnosis of subtle findings.
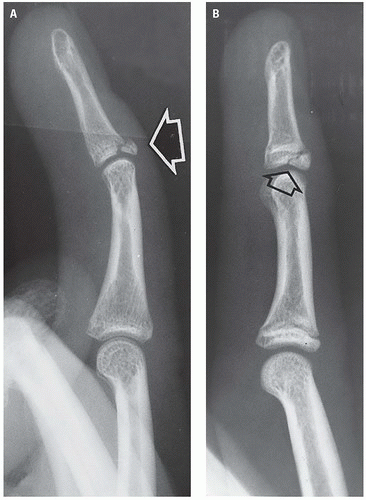
Mallet Finger
“Mallet” finger and “baseball” finger are terms given to the same flexion deformity at the distal interphalangeal joint, which results from a proximally retracted avulsion fracture of the dorsum of the base of the distal phalanx to which the extensor tendon is inserted. The flexion deformity is due, therefore, to the unopposed action of the flexor tendon inserted on the volar aspect of the phalanx. This injury most commonly involves the distal phalanx of the long finger (Figs. 11.7 and 11.8).
The “mallet” finger is the result of the tip of the finger being struck, such as in the act of catching a baseball, softball, or basketball, causing forceful hyperflexion of the distal interphalangeal joint when the extensor tendon is taut, or it is the result of forceful hyperextension of the distal interphalangeal joint. Proximal retraction of the dorsal fragment indicates that the common extensor tendon is attached to the separate fragment.
When the extensor tendon inserts distal to the fracture of the dorsum of the base of the distal phalanx, the separate fragment will neither be retracted nor will there be a flexion deformity at the distal interphalangeal joint (Fig. 11.8B).
Variations of the mallet finger deformity are dependent on the site of the fracture and the relation of the volar plate and of the extensor and flexor tendon insertions to the fragments. Figures 11.9 and 11.10 illustrate two such variants. It is important for the radiologist to have an understanding of the soft tissue anatomy of the interphalangeal joints so that the status of the ligaments and tendons can be incorporated into the interpretation of the radiographic examination.
Volar Plate Injury
The volar plate is a dense fibrous band that forms the palmar aspect of the capsule of the thumb MCP and finger proximal interphalangeal joints (Fig. 11.11




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree