Elbow
Theodore T. Miller
INTRODUCTION
The elbow is commonly injured in sports and occupational activities. Elbow injuries account for approximately 20% of upper extremity sports injuries1 and the elbow is the second most commonly dislocated joint after the shoulder.2 The elbow is well suited to sonographic evaluation: it is small and easily manipulated by the examiner, enabling dynamic assessment; it is accessible around its entire circumference, allowing long and short axis scanning of every segment of the joint; and the structures of interest are superficial and linear and thus easily examined.
ANATOMY AND TECHNIQUE
Linear high-frequency transducers should be used since the ligaments, tendons, and nerves about the elbow are superficial and linear. Unlike the shoulder, which has a standard scanning protocol, the elbow is scanned by placing the transducer over the site of clinical concern. Nonetheless, for the purpose of the description of anatomy, the elbow can be divided into four quadrants: anterior, lateral, posterior, and medial.3
Anterior Quadrant
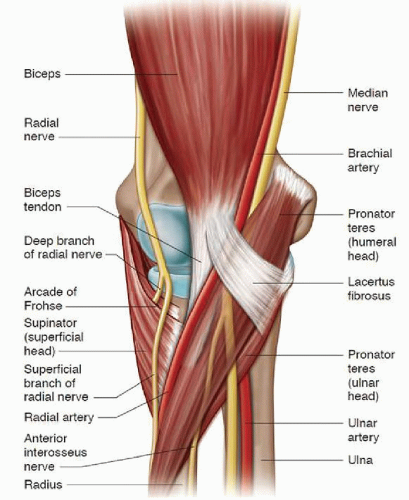
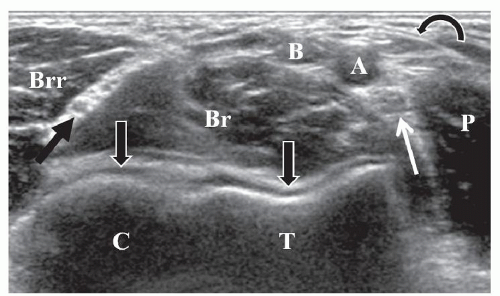
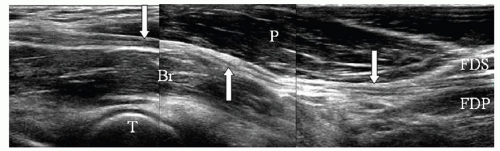
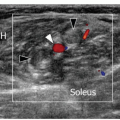
The anterior quadrant contains the biceps muscle and tendon, the radial and median nerves, and the anterior aspects of the radiocapitellar and humeroulnar joints. Scanning is performed with the elbow extended and supinated (Fig. 4.1). The transducer is placed transversely across the distal arm. The pulsating brachial artery is midline and is a major landmark. Lateral to the brachial artery is the distal biceps tendon, and medial to the brachial artery is the median nerve. The biceps aponeurosis (also called the lacertus fibrosus) is a fascial layer that extends from the flexor pronator muscle group to the biceps tendon (Figs. 4.2 and 4.3).
Tip:
You may have to rock the transducer cranially to make the tendons and nerves echogenic.
 Figure 4.1. Scanning of the anterior quadrant. The transducer is placed transversely across the antecubital fossa. |
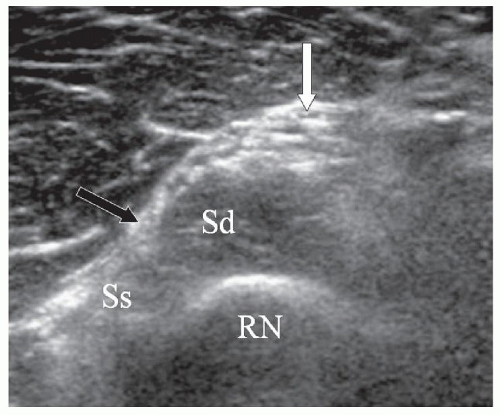
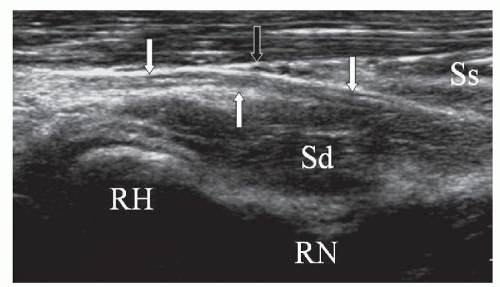
As the transducer slides distally, the anterior aspects of the radiocapitellar and humeroulnar joints come into view. The curvilinear bony surfaces are covered by anechoic articular cartilage. The radial nerve is visible deep to the brachioradialis muscle at this level (Fig. 4.3). As the transducer moves distally, the deep branch of the radial nerve can be identified as it enters the supinator muscle between the superficial and deep muscle heads (Fig. 4.4). Rotating the transducer 90 degrees over either the radial or median nerves demonstrates the hypoechoic fibrillar appearance of the nerve in long axis (Fig. 4.5).
The radial nerve is the terminal branch of the posterior cord of the brachial plexus (C5-8, T1). In the arm it courses posterior to the humerus in the spiral groove, and pierces the intermuscular septum in the distal arm to lie anterior to the lateral condyle of the humerus. The radial nerve supplies the triceps, anconeus, brachioradialis, and the lateral half of the brachialis.
At the level of the elbow joint, the radial nerve divides into a superficial sensory branch, which courses in the forearm along the deep surface of the brachioradialis, and a deep motor branch, which enters the radial tunnel. The radial tunnel extends from the level of the radiocapitellar joint to the proximal aspect of the supinator,4 and is bounded by the joint capsule posteriorly, the
brachialis muscle and biceps tendon medially, and the brachioradialis muscle and the extensor carpi radialis brevis and longus muscles laterally.5
brachialis muscle and biceps tendon medially, and the brachioradialis muscle and the extensor carpi radialis brevis and longus muscles laterally.5
At the distal aspect of the radial tunnel, the deep branch pierces the supinator muscle anteriorly between the superficial and deep heads of the supinator (Figs. 4.2 and 4.5). The proximal edge of the superficial head of the supinator is called the Arcade of Frohse and is the most common site of radial nerve entrapment (Fig. 4.2). The deep branch of the radial nerve exits the posterior aspect of the supinator as the posterior interosseous nerve (PIN) and enters the posterior compartment of the forearm. At the elbow, the deep branch supplies the extensor carpi radialis brevis and the supinator. In the posterior compartment of the forearm, the deep branch, now called the PIN, supplies the extensor carpi ulnaris, the extensor digitorum communis, the extensor digiti minimi, the abductor pollicis longus, the extensor pollicis longus and brevis, and the extensor indicis proprius.4
The median nerve arises from the medial and lateral cords of the brachial plexus (C6-8, T1) and courses
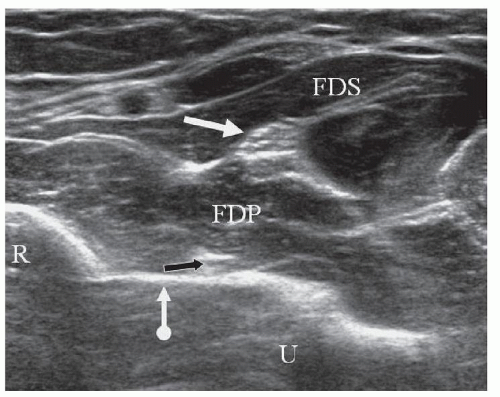
alongside the brachial artery in the anterior compartment of the arm and at the elbow, passing through the antecubital fossa deep to the biceps aponeurosis (see below) and anterior to the brachialis muscle. The nerve lies between the humeral (superficial) and ulnar (deep) heads of the pronator teres muscle at the level of the elbow joint (Fig. 4.2), and enters the anterior compartment of the forearm by passing beneath the fibrous arch of the heads of the flexor digitorum superficialis (FDS)6 (Fig. 4.6). At the elbow and proximal aspect of the forearm the median nerve supplies the pronator teres, flexor carpi radialis, palmaris longus, and FDS.7 Within the forearm, the nerve courses between the FDS and FDP.
alongside the brachial artery in the anterior compartment of the arm and at the elbow, passing through the antecubital fossa deep to the biceps aponeurosis (see below) and anterior to the brachialis muscle. The nerve lies between the humeral (superficial) and ulnar (deep) heads of the pronator teres muscle at the level of the elbow joint (Fig. 4.2), and enters the anterior compartment of the forearm by passing beneath the fibrous arch of the heads of the flexor digitorum superficialis (FDS)6 (Fig. 4.6). At the elbow and proximal aspect of the forearm the median nerve supplies the pronator teres, flexor carpi radialis, palmaris longus, and FDS.7 Within the forearm, the nerve courses between the FDS and FDP.
The anterior interosseous nerve (AIN) arises from the median nerve at the level of the humeral head of the pronator teres, and travels along the anterior aspect of the interosseous membrane of the forearm between the flexor pollicis longus and the flexor digitorum profundus (Fig. 4.7). The AIN is purely motor and supplies the pronator quadratus muscle, the flexor pollicis longus muscle, and the FDP muscle for the index and the middle fingers.4,8
Longitudinal scanning over the radiocapitellar joint shows the joint space and the thin stripe of anechoic articular cartilage of the capitellum (Fig. 4.8). Sliding the transducer medially demonstrates the coronoid fossa of the distal humerus. This is a good place to look for joint fluid and intra-articular loose bodies.
The distal biceps tendon can be challenging to image because it dives deep in the antecubital fossa to insert on the radial tuberosity and because it does not have a straight sagittal orientation. There are several techniques for scanning the distal biceps:
Anterior approach3,9—With the arm extended and maximally supinated, find the tendon in short axis in the distal arm, just proximal to the elbow crease, and then rotate the transducer 90 degrees (Fig. 4.9). Alternatively, place the transducer longitudinally on the antecubital fossa, find the brachial artery, and then slide the transducer just lateral to the artery (Fig. 4.10).
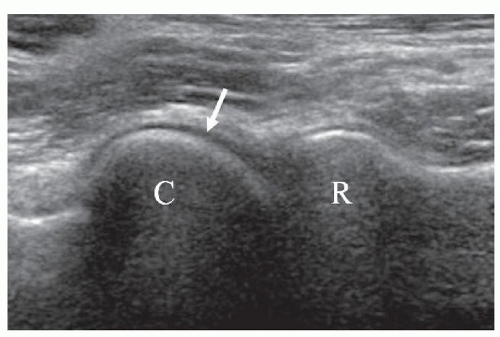
Figure 4.8. Long-axis image shows the capitellum (C), thin hypoechoic cartilage (arrow), and the radial head (R).

Figure 4.9. Anterior approach to the biceps tendon. The transducer is long axis and pressed into the interosseous space. The forearm is maximally supinated.

Figure 4.12. Lateral approach to the biceps tendon. The elbow is bent 90 degrees, the forearm is supinated, and the transducer is placed obliquely along the course of the biceps tendon.
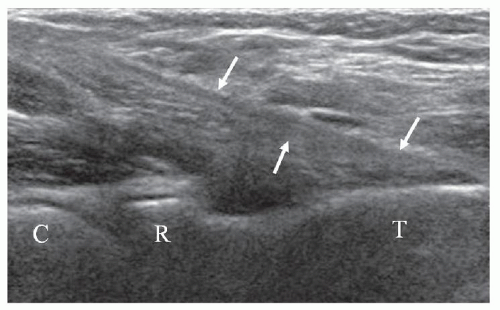
Lateral approach10—With the elbow bent 90 degrees and the forearm supinated, place the transducer longitudinally over the lateral aspect of the forearm, using the brachioradialis muscle as an acoustic window (Figs. 4.12 and 4.13).
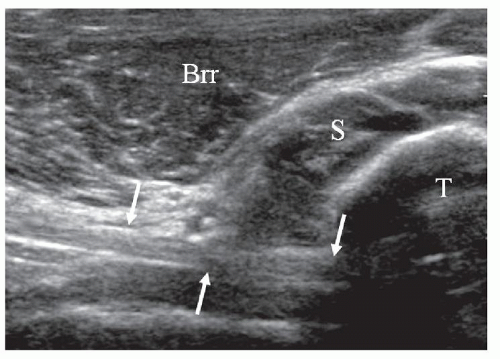
Figure 4.14. Lateral approach to the biceps tendon is seen in long axis (arrows), while the radial tuberosity (T) is seen in short axis. Brr, brachioradialis; S, supinator.
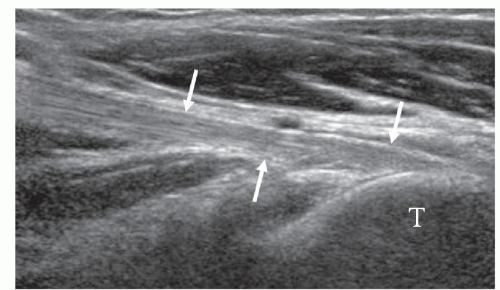
Medial approach11—With the elbow bent 90 degrees and the forearm supinated, place the transducer longitudinally over the distal aspect of the arm from the medial side (Fig. 4.15). Slide the transducer anteriorly until the tendon is identified, and then slide distally, using the flexor-pronator mass as an acoustic window. The radius will be seen in short axis in this method, similar to the lateral approach (Fig. 4.16).
Posterior approach12—With the elbow maximally flexed and the forearm pointing toward the ceiling, place the transducer transversely against the dorsal aspect of the proximal forearm at the level of the radial tuberosity (Fig. 4.17). As the patient supinates and pronates the forearm, the distal aspect of the biceps tendon is identified (Fig. 4.18).
Tip:
To optimally visualize the distal biceps tendon, “heel-toe” the transducer by pressing the distal aspect of the transducer footprint into the forearm and rotate the transducer toward the radius using the radial head, neck, and tuberosity as bony landmarks (Fig. 4.11).
 Figure 4.15. Medial approach to the biceps tendon. The elbow is bent 90 degrees and the transducer is placed parallel to the arm. |
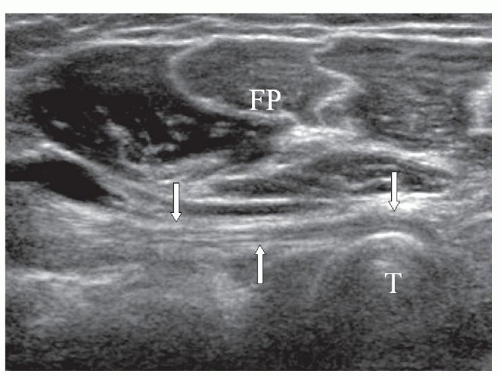 Figure 4.16. Medial approach to the biceps tendon is seen in long axis (arrows), while the radial tuberosity (T) is seen in short axis. Flexor pronator mass (FP). |
In long-axis the biceps tendon is of uniform caliber and has the typical echogenic, fibrillar appearance of a tendon. It appears round and well-defined in short-axis scans. Long head and short head components of the distal biceps tendon have been described, with the long tendon being deeper and inserting on the more proximal aspect of the radial tuberosity and the short tendon being more superficial and inserting more distally,13 but these two components are usually difficult to separate. The bicipitoradial bursa sits saddle-shaped around the
distal biceps tendon to protect it from osseous friction during pronation of the forearm.14 It is not normally distended.
distal biceps tendon to protect it from osseous friction during pronation of the forearm.14 It is not normally distended.
Lateral Quadrant
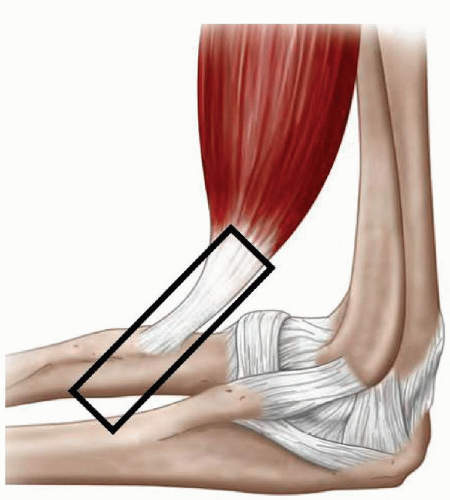
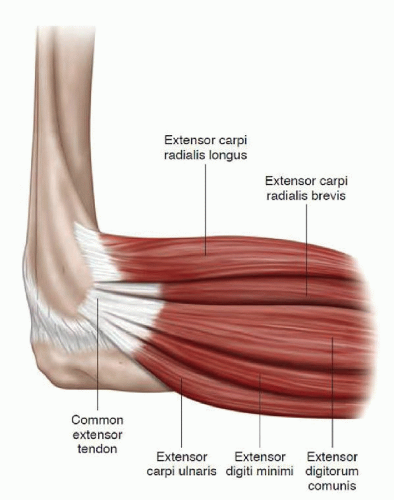
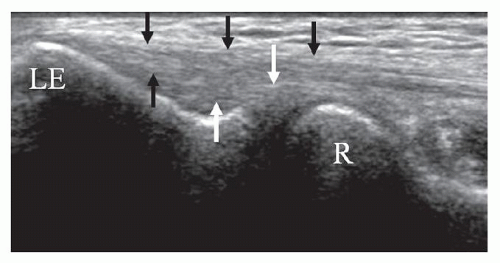
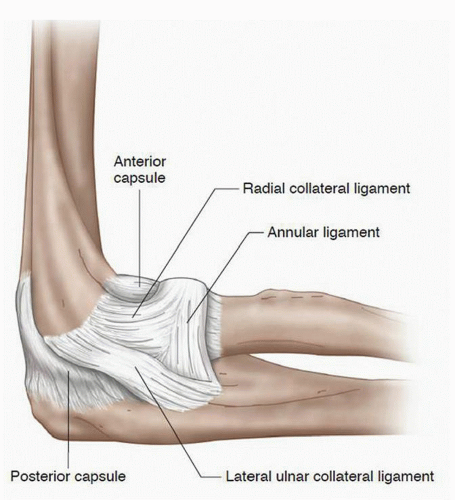
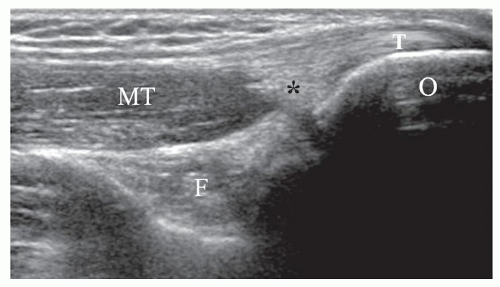
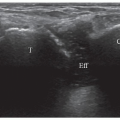
The lateral quadrant contains the lateral aspect of the radiocapitellar joint, the common extensor tendon, and the lateral collateral ligament complex that consists of the radial collateral ligament, lateral ulnar collateral ligament, and the annular ligament.15,16,17 With the patient’s elbow flexed 80 to 90 degrees and the forearm on the examination table, the transducer is placed longitudinally on the lateral elbow at the level of the radiocapitellar joint using the bony landmarks of the radial head and lateral epicondyle (Fig. 4.19). The common extensor tendon originates from the lateral epicondyle of the humerus and is comprised of the extensor carpi radialis brevis, extensor carpi ulnaris, extensor digitorum communis, and extensor digiti minimi (Fig. 4.20). The common tendon has a long thin echogenic fibrillar appearance (Fig. 4.21).
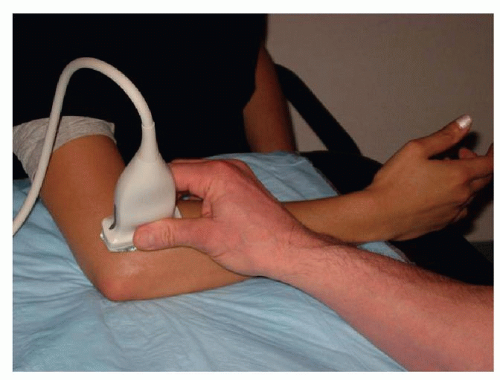 Figure 4.19. Scanning the lateral quadrant. The elbow is flexed, the thumb is up, and the transducer is placed long axis over the radial head. |
The radial collateral ligament complex is composed of the radial collateral ligament, the lateral ulnar collateral ligament, and the annular ligament15,16,17 (Fig. 4.22). The radial collateral ligament lies deep to the common extensor tendon, extending from the undersurface of the lateral epicondyle to blend with the fibers of the annular ligament. It is often difficult to distinguish the radial collateral ligament as a distinct structure from the overlying common extensor tendon (Fig. 4.21).
Short axis scanning over the radial head demonstrates the thin annular ligament. Oblique scanning is necessary to visualize the lateral ulnar collateral ligament, which extends from the undersurface of the lateral epicondyle, passes posterior to the radial head and neck, thus acting as a supporting sling, and inserts on the supinator crest of the ulna.15,16
Posterior Quadrant
The posterior quadrant contains the triceps tendon, olecranon fossa, and ulnar nerve, and it can be scanned in several ways:
The “crawling crab” position, in which the patient’s hand is placed on the examination table with the elbow up and rotated toward the examiner (Fig. 4.23). The disadvantage of this position is that it is static.
The elbow is flexed 90 degrees with the forearm resting on the examination couch in front of the patient (Fig. 4.24). This position is good for the triceps but is difficult for the ulnar nerve since the medial aspect of the elbow is lying against the table.
The patient’s arm is elevated by the examiner who holds the patient’s forearm with one hand and places the transducer against the posterior aspect of the elbow with the other hand. The patient’s elbow rests against the palm of the examiner (Fig. 4.25). The advantage of this technique is that it allows dynamic scanning as the examiner flexes and extends the elbow by moving the patient’s forearm. This is particularly helpful for the evaluation of a clinically suspected
snapping ulnar nerve. The disadvantage is that it requires a steady and experienced hand since both the patient’s elbow and the examiner’s hand are freefloating in the air.
 Figure 4.23. Crawling crab position. The posterior quadrant is well accessible but the elbow is static. |
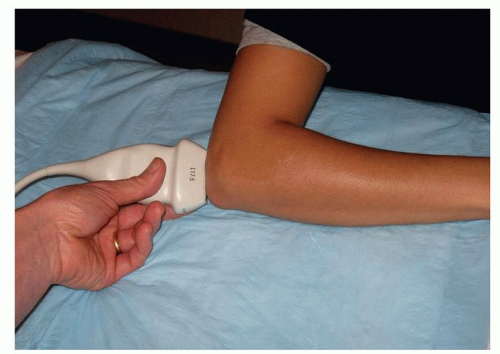 Figure 4.24. The elbow is flexed 90 degrees with the forearm resting on the examination table. The ulnar nerve is difficult to assess in this position. |
 Figure 4.25. Posterior approach for dynamic scanning. This technique is good for assessment of a snapping ulnar nerve or triceps muscle. |
The triceps tendon is a short broad structure with an echogenic fibrillar appearance composed of contributions of the long and lateral heads,18 and inserts on the superficial aspect of the olecranon process The medial head of the triceps muscle has a separate insertion on the olecranon process, deep to the tendon (Fig. 4.26). With the elbow flexed, the olecranon fossa of the humerus is exposed and can be viewed both in short and long axis (Fig. 4.27).
Tip:
The olecranon fossa is a good place to look for synovitis, joint effusion, and loose bodies, and is a good target for elbow aspiration.
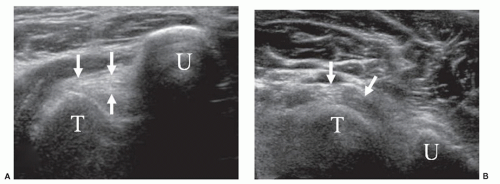
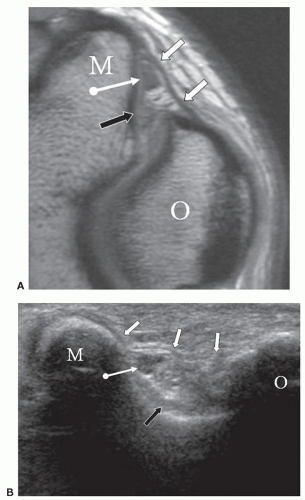
In short axis, slide the transducer medially, posterior to the medial epicondyle to visualize the ulnar nerve. The ulnar nerve arises from the medial cord of the brachial plexus (C8, T1) and courses along the medial side of the brachial artery in the anterior compartment of the proximal arm. It then passes posterior to the medial epicondyle of the humerus in the cubital tunnel, a fibro-osseous channel formed by the olecranon process
laterally, the posterior cortex of the medial epicondyle medially, the elbow joint capsule and posterior bundle of the medial collateral ligament (MCL) anteriorly, and the Ligament of Osborne (the cubital retinaculum) posteriorly (Fig. 4.28). The nerve exits the cubital tunnel to enter the medial aspect of the forearm between the superficial and deep heads of the flexor carpi ulnaris muscle. At the elbow, the ulnar nerve supplies the flexor carpi ulnaris and the medial half of the FDP.
laterally, the posterior cortex of the medial epicondyle medially, the elbow joint capsule and posterior bundle of the medial collateral ligament (MCL) anteriorly, and the Ligament of Osborne (the cubital retinaculum) posteriorly (Fig. 4.28). The nerve exits the cubital tunnel to enter the medial aspect of the forearm between the superficial and deep heads of the flexor carpi ulnaris muscle. At the elbow, the ulnar nerve supplies the flexor carpi ulnaris and the medial half of the FDP.
In the cubital tunnel, the ulnar nerve appears round and hypoechoic, surrounded by echogenic fat in transverse scans, and narrow, linear, and hypoechoic in longitudinal scans. Nerve stability is assessed while scanning transversely during flexion and extension of the elbow.
Medial Quadrant
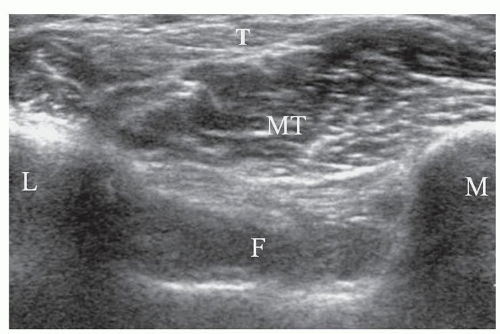
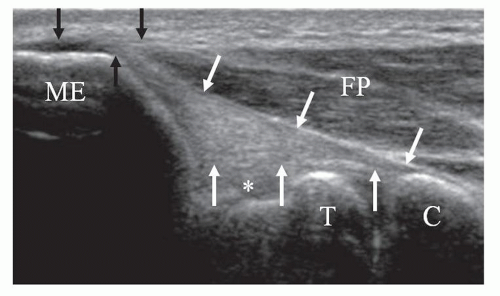
The medial quadrant contains the common flexor tendon and MCL and is scanned with the elbow extended and the forearm supinated (Fig. 4.29). The common flexor tendon originates from the medial epicondyle of the humerus. It is composed of the flexor-pronator group of muscles: pronator teres, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris (Fig. 4.30).
The common flexor tendon is shorter and broader than the common extensor tendon, and has an echogenic fibrillar appearance as it attaches on the medial epicondyle (Fig. 4.31). It is well demonstrated by placing the transducer longitudinally over the medial joint line.
The common flexor tendon is shorter and broader than the common extensor tendon, and has an echogenic fibrillar appearance as it attaches on the medial epicondyle (Fig. 4.31). It is well demonstrated by placing the transducer longitudinally over the medial joint line.
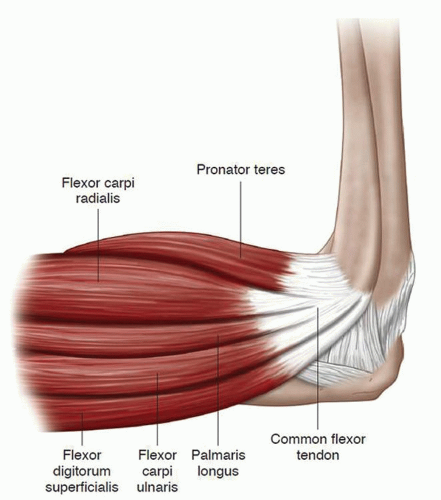 Figure 4.30. Diagram of the flexor pronator group, forming the common flexor tendon. The pronator teres and flexor carpi radialis components are most commonly involved in medial epicondylitis. |
Deep to the common flexor tendon is the anterior bundle of the MCL. The MCL is also composed of a posterior bundle and a transverse bundle, but the anterior bundle is the primary restraint to valgus stress, is the bundle that is usually of clinical concern, and is most visible at imaging (Fig. 4.32). The anterior bundle has a fan shape, with a broad origin on the undersurface of the medial condyle and a thin insertion on the sublime tubercle of the coronoid process of the ulna (Fig. 4.31).
Tip:
The anterior bundle of the MCL may have a hypoechoic appearance because of its oblique course distally. Press the distal aspect of the transducer into the forearm to make the ligament more echogenic.
TENDON PATHOLOGY
Epicondylitis
Lateral epicondylitis (“tennis elbow”) is the term used for pain over the lateral epicondyle and proximal lateral forearm during wrist extension and supination. It is an overuse injury typically affecting the extensor carpi radialis brevis component of the common extensor tendon,19 and got the name “tennis elbow” because of its association with poor backhand technique in amateur players,20 but most cases are not due to tennis, and it may be encountered in the lead elbow of professional golfers21 and activities that require repetitive extension and supination of the wrist.19 Lateral epicondylitis and radial nerve neuropathy may have similar clinical presentations, and imaging plays an important role in distinguishing the two conditions.22
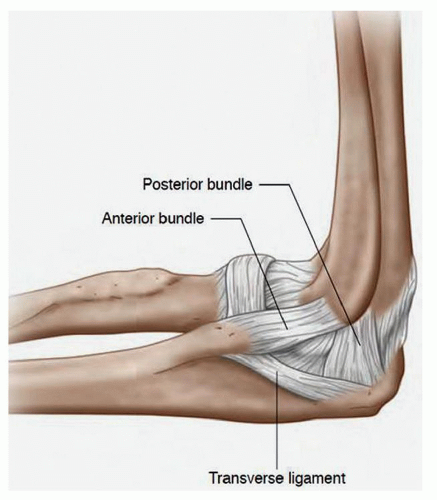 Figure 4.32. Diagram of the medial collateral ligament, showing the anterior and posterior bundles and the transverse ligament component. |
Medial epicondylitis is the term used for pain over the medial epicondyle with wrist and finger flexion and wrist pronation. It is less common than lateral epicondylitis. Medial epicondylitis is also called “golfer’s elbow”, affecting the trail arm as a result of poor swing technique in amateur golfers,21 but most cases are not due to golf. Weight lifting, bowling, and throwing are all associated with medial epicondylitis due to the valgus stress that accompanies these activities.23 The pronator teres and flexor carpi radialis components are predominantly affected.24 Patients with medial epicondylitis may also have ulnar neuritis due to tensile and valgus compressive loads that produce medial epicondylitis.
The term “epicondylitis” is a misnomer, since histologically there is no acute inflammatory process.25,26,27 Rather, it is a degenerative process due to repetitive microtrauma of the common extensor or flexor tendons, with micro tearing of the fibers leading to mucoid degeneration, angiofibroblastic proliferation, and eventual macro tearing if the offending activity continues.
Sonographically, the process looks similar regardless of the side affected. In the early stages the tendon may be hypoechoic and/or thickened (Fig. 4.33).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree