and Siddharth P. Jadhav2
(1)
Department of Radiology, University of Texas Medical Branch Pediatric Radiology, Galveston, TX, USA
(2)
The Edward B. Singleton Department of Pediatric Radiology, Texas Children’s Hospital, Houston, TX, USA
Abstract
This chapter deals with injuries of the elbow and forearm. Various types of fractures and other injuries are presented. MR is discussed where it significantly adds to evaluation of these injuries.
Normal Soft Tissues and Fat Pads
In the elbow, the most important fat pads to assess are the anterior and posterior fat pads over the distal humerus [1]. The anterior fat pad is located in the coronoid fossa while the posterior fat pad is located in the olecranon fossa. These fat pads must be evaluated on true lateral, flexed views of the elbow, for with any degree of rotation or extension, their usefulness diminishes or becomes totally invalid. Normally, on the true lateral flexed view of the elbow, the anterior fat pad is visible, but the posterior fat pad is not (Fig. 6.1a). The reason for the lack of visualization of the posterior fat pad is that it lies deep in the olecranon fossa. It becomes visible only if fluid in the joint displaces it posteriorly. On extension it may be visible in normal individuals, but never on a flexed view. These fat pad configurations are very consistent, and any deviation from the normal pattern should be considered abnormal and suspicious. On the other hand, if the fat pads are normal, underlying abnormality is basically nonexistent [2].


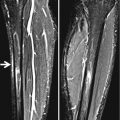
Fig. 6.1
Elbow fat pads. (a) Note the position of the normal anterior fat pad (arrow). The posterior fat pad is not visible on normal 90° flexed elbows. (b) In this patient with fluid in the joint from an injury, both the anterior and posterior fat pads (arrows) are elevated. (c) Normal supinator fat pad. Note the appearance and position of the normal supinator fat pad (arrow)
Fluid in the elbow joint usually produces upward and outward displacement of the anterior and posterior fat pads, often referred to as the “sail sign” or the “fat pad sign” (Fig. 6.1b). These fat pads are intracapsular but extrasynovial [3] and their displacement is very accurate in reflecting the presence of intra-articular fluid. Ultrasonography also can be used to detect fluid in the elbow joint [4] but seldom is needed because the findings on true lateral elbow images are very sensitive.
The supinator fat pad [5] is another normal fat pad around the elbow. It also is seen on true lateral views and overlies the anterior aspect of the supinator muscle (Fig.6.1c). This fat pad is less consistently visualized in infants and young children, but in older children when it is obliterated/displaced, fractures of the proximal radius should be suspected. It also can be obliterated with generalized, nonspecific edema around the elbow.
Finally, in the elbow it is important to appreciate whether soft tissue swelling is present and whether it predominates medially or laterally. The reason for this is that with lateral swelling a fracture of the lateral condyle and capitellum should be suspected, while with medial swelling fractures of the medial epicondyle should be sought for. These findings are more specifically addressed in future sections of this chapter.
Elbow Fractures and Injuries
Injuries of the three bones around the elbow are perhaps one of the most commonly encountered injury groups in infants and children. Each of these bones, because of their configuration and articulations tend to fracture in different ways. It is most important to appreciate these mechanisms of injury because this enables one to detect the more subtle injuries [6]. For the most part, elbow injuries are sustained by falling on the hyperextended upper extremity (“FOOSH” injury). In this injury axial loading forces act on all three bones, while hyperextension forces act on the distal humerus. Rotatory forces along with varus and valgus forces act on the radius and ulna. These force patterns are reviewed more specifically as the individual fractures are dealt with in this chapter. In children with elbow trauma, MR imaging reveals a broad spectrum of bone and soft tissue injury beyond that recognizable radiographically. However, the additional information afforded by MR imaging has little bearing on treatment or clinical outcome [7]. As a result, MR of the elbow is rarely indicated in the ER setting.
Injuries of the Distal Humerus
The most common fracture sustained in the elbow is the supracondylar fracture through the distal humerus, and in our study of over 400 infants and children with elbow injuries [5], supracondylar fracture occurred in 68 % of the patients, lateral condylar fractures in 23 %, and medial epicondylar fractures in 9 % of patients.
The supracondylar fracture results from a fall on the outstretched upper extremity where the olecranon locks into the olecranon fossa producing a “can-opener” effect on the distal humerus resulting in a supracondylar fracture with the distal fracture fragment being posteriorly tilted (Fig. 6.2a). In the classic case the findings are not difficult to identify (Fig. 6.2b, c). However, in some cases while the fracture is obvious on lateral view, it is difficult to visualize on the frontal view. In addition, if the fracture is a plastic/bending fracture, less posterior angulation occurs, a fracture line is not visualized, and it may be difficult to confidently identify the fracture without comparative views. In this situation the anterior humeral line of Rogers et al. [8] becomes very useful.


Fig. 6.2
Supercondylar fracture: injury mechanics. (a) Axial loading forces are applied down the humerus (upper arrow), while “can-opener”-like forces are applied to the distal humerus by the hyperextended ulna (lower arrow). The ulna becomes locked in the trochlear notch, leading to impaction forces (Impact) applied to the posterior aspect of the distal humerus and a fracture (fx) results. (b) Typical imaging findings: lateral view. The point of impact occurs posteriorly (arrow) with a resultant fracture (fx) anteriorly. The entire distal humeral fragment is posteriorly tilted. (c) Anteroposterior view demonstrates the transverse fracture (arrows)
The anterior humeral line is a line drawn along the anterior aspect of the distal humerus and should be applied on true lateral views. Under normal circumstances, it intersects the ossified capitellum somewhere through its middle or posterior third. If it intersects the capitellum through the anterior third or if it misses it entirely, a supracondylar fracture is present (Fig. 6.3). The anterior humeral line is a little more difficult to apply in the young infant where the capitellum is incompletely ossified, but even in these cases, if the findings are compared with those on the normal side, posterior displacement can be detected. In addition to the foregoing, I have found it useful to compare the classic supracondylar fracture to a hockey stick and the plastic bending supracondylar fracture to a polo stick [9] (Fig. 6.4). A spectrum of supracondylar fractures is presented in Fig. 6.5.


Fig. 6.3
Subtle supracondylar fracture: anterior humeral line. (a) Anteroposterior (AP) view. Note the very subtle buckle fracture (arrow) in the distal humerus. Swelling around the area is present. (b) Lateral view demonstrates a minimal posterior buckle fracture (arrow). Both fat pads are elevated. Note the position of the capitellum. (c) Normal side for comparison. First note the position of the capitellum and compare it to the posteriorly displaced capitellum in (b). (d) Anterior humeral line: fracture side. The anterior humeral line intersects the capitellum through the anterior third. (e) Anterior humeral line: normal side. The anterior humeral line intersects the normal capitellum through its posterior third
Fig. 6.4
Supracondylar fracture: polo versus hockey stick. (a) Note elevated fat pads. An overt fracture is not seen but the distal humerus and capitellum are slightly posteriorly tilted (plastic fracture). The capitellum lies directly below the humerus. (b) The configuration resembles a “polo stick” en face. (c) Normal side for comparison. Note the position of the capitellum. It is more anterior in location than in (a). (d) The overall configuration resembles a “hockey stick” (Reprinted from Swischuk [9]. With permission from Springer Science + Business Media)
Fig. 6.5
Spectrum of supracondylar fractures. (a) Minimal plastic bending fracture with a subtle posterior buckle. Note position of the capitellum. (b) Plastic bending fracture of the distal humerus with smooth posterior angulation of the distal humerus. (c) Overt supracondylar fracture with posterior cortical angulation and an anterior fracture line. (d) Completely displaced supracondylar fracture
Another fracture occurring through the distal humerus in conjunction with the supracondylar hyperextension fracture is the “T” fracture. In these cases not only are hyperextension forces applied to the distal humerus, but axial loading on both the lateral and medial condyles results in splitting of the distal humerus and the resultant “T” fracture. This fracture is not difficult to detect. Finally, it should be noted that in some cases a supracondylar fracture with faulty alignment and subsequent healing can result in a cubitus varus (gunstock) deformity of the elbow [10].
A reverse supracondylar fracture results when forces are applied to the posterior aspect of the distal humerus, for example, with falling backwards and landing on the elbow. These fractures are not difficult to detect as they usually are overt.
With condylar and epicondylar injuries of the distal humerus, it is the lateral condyle and medial epicondyle which most commonly are injured. Medial condylar [11] and lateral epicondylar fractures are rare. Lateral condylar fractures tend to occur in young infants and children, while medial epicondylar fractures more often, but not exclusively, occur in older children. Many of these fractures are subtle and examination of the soft tissues becomes important. In this regard abnormality of the elbow fat pads usually is present, but more important is that there usually is telltale unilateral swelling and edema of the soft tissues over the involved area [12]. With lateral condylar fractures, such swelling occurs laterally, while with medial epicondylar fractures, it occurs medially. The presence of such unilateral soft tissue edema is especially important in the assessment of medial epicondylar injuries with minimal or no displacement of the epicondyle or in children younger than 7 years of age in whom the epicondyle often is not yet ossified.
Lateral condylar fractures [13] result when varus forces are applied to the elbow (Fig. 6.6), and in such cases it is most important to determine whether the fracture is undisplaced or displaced and rotated. If the fracture extends through the cartilage between the capitellum and the trochlea, the hinge-like stabilizing function of a nondisplaced fracture fragment is lost, and the injury becomes unstable (Fig. 6.7). At the other end of the spectrum of lateral condylar fractures, only a crescent-/sliver-shaped fragment of bone is avulsed (Fig. 6.8). This fragment can be clearly apparent or very difficult to identify because of its thin sliver-like configuration. In these latter cases it is important to appreciate that the sliver of bone curves downwardly with the apex of the curve pointing downward (Fig. 6.8). The reason this is important is because a psuedofracture configuration can be seen in normal elbows with superimposition of the capitellum on the metaphysis of the humerus. In these cases the apparent “pseudofracture” is convex in the opposite direction with the curve pointing upward (Fig. 6.9).
Fig. 6.6
Lateral condyle fracture. (a) Diagrammatic representation. Axial loading forces are present (force). In addition there are distraction forces applied to the lateral elbow resulting in a lateral condylar avulsion fracture (fx). Fractures of the proximal ulna can coexist. (b) Diagrammatic representation of instability. Stable the fracture does not traverse the cartilage plate. A hinge remains and the fracture is stable, Unstable with a complete fracture no hinge is present and the fracture is unstable
Fig. 6.7
Typical lateral condylar avulsion fracture. (a) First note the swelling (arrows) over the lateral aspect of the elbow. (b) Now note the avulsed fracture fragment (arrow)
Fig. 6.8
Subtle, sliver-like avulsion fractures. (a) Note the subtle thin avulsed fracture fragment (arrow). (b) Another patient demonstrating similar, but less pronounced findings of an avulsion fracture (arrow). There is suggestion of a minimal buckle fracture of the distal humerus on the medial side. (c) Another patient. Healing phase. Note periosteal new bone and callus (arrow) at the fracture site
Fig. 6.9
Pseudofracture; lateral condyle. With certain positioning the cartilaginous plate between the capitellum and lateral condyle is visualized through the distal humeral metaphysis and may erroneously suggest a fracture (arrowheads). Compare with a true fracture in Fig. 6.8
Finally, it might be appreciated that in some cases of lateral condylar avulsion fracture, the fracture is not seen on AP views but can be seen on lateral or oblique views (Fig. 6.10). Oblique views are not standard views for elbow injuries, but very often because a proper lateral view cannot be obtained, the one submitted is slightly obliqued and the fracture becomes visible. A spectrum of lateral condylar avulsion fractures is presented in Fig. 6.11.



Fig. 6.10
Subtle fractures: value of lateral and oblique images. (a) In this patient a very subtle thin sliver-like avulsed fracture fragment (arrow) is seen. (b) On the oblique film the fracture fragment (arrow) is more clearly identified. (c) Another patient. Again note a subtle thin avulsed fracture fragment (arrow). (d) Lateral view more clearly demonstrates the fracture (arrow)

Fig. 6.11
Spectrum of lateral condylar fractures. (a) In this patient a minimal nondisplaced sliver-like avulsed fracture fragment (arrow) is seen. (b) A more classic fracture (arrow) is present. (c) Total avulsion of the capitellum and underlying condylar cortex along with rotation of the fracture fragment (arrow)
With medial epicondylar injuries [14], a wide range of abnormality also occurs raging from simple separation of the epicondyle to complete dislocation, with or without intra-articular entrapment (with elbow dislocations) of the epicondyle. Medial epicondylar injuries result from rotatory forces applied to the bones distal to the elbow (Fig. 6.12). When this occurs there is excessive pull on the medial epicondyle by the flexor pronator muscle/tendon (Fig. 6.12). In some cases minimal or no displacement of the medial epicondyle is seen, but soft tissue changes are present (Fig. 6.13a). In addition the medial epicondyle often also can be avulsed after the epiphyses have fused (Fig. 6.13b).
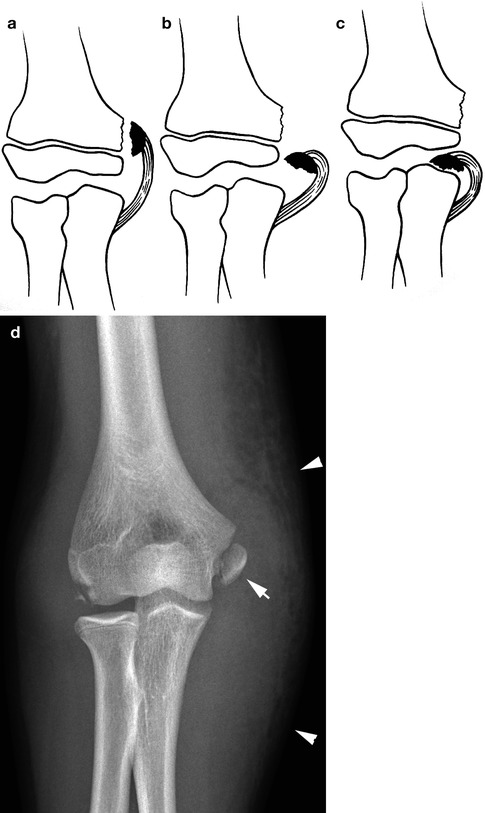
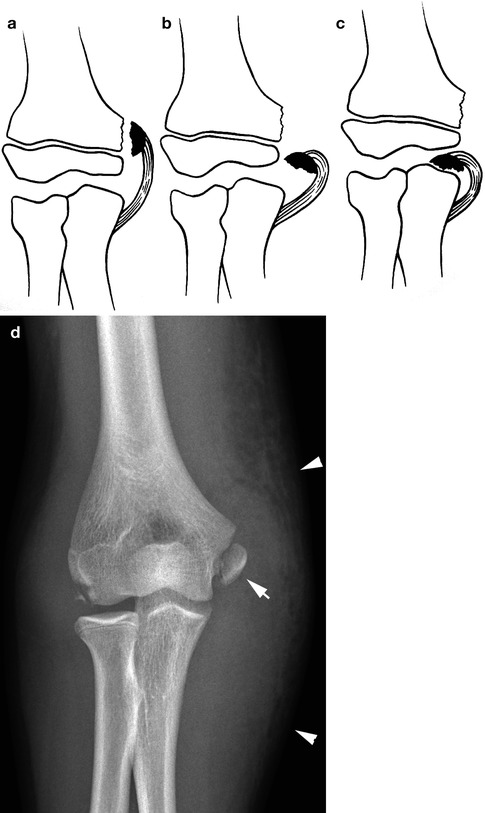
Fig. 6.12




Medial epicondyle avulsion: injury mechanics. (a) Simple avulsion of the medial epicondyle. (b) Complete avulsion of the medial epicondyle. (c) Complete avulsion and entrapment in the elbow joint. (d) Typical avulsed medial epicondyle (arrow). Note extensive swelling over the medial aspect of the elbow (arrowheads)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree