and Siddharth P. Jadhav2
(1)
Department of Radiology, University of Texas Medical Branch Pediatric Radiology, Galveston, TX, USA
(2)
The Edward B. Singleton Department of Pediatric Radiology, Texas Children’s Hospital, Houston, TX, USA
Abstract
This chapter provides a summary of the various types of fractures seen in children. It serves as a basis for later evaluation of these fractures at different sites in the body.
Types of Fractures Seen in Children
The types of fractures most peculiar to childhood are (a) cortical/buckle or torus fractures, (b) greenstick fractures, (c) plastic bending or bowing fractures, and (d) epiphyseal–metaphyseal (Salter–Harris) fractures (Fig. 4.1). Of course, typical midshaft, transverse, spiral, oblique, and comminuted fractures also occur, but none are specifically peculiar to childhood, and most are not difficult to detect unless they are hairline fractures which occur most commonly in the tibia and small bones of the hands and feet. In the tibia, the original diaphyseal spiral toddler fracture described by Dunbar et al. [1] and the more recently described upper tibial hyperextension-induced fracture of the tibia [2] are the most common hairline fractures seen in the lower extremity. We have over the years referred to these fractures, respectively, as the toddler fracture type I and toddler fracture type II.
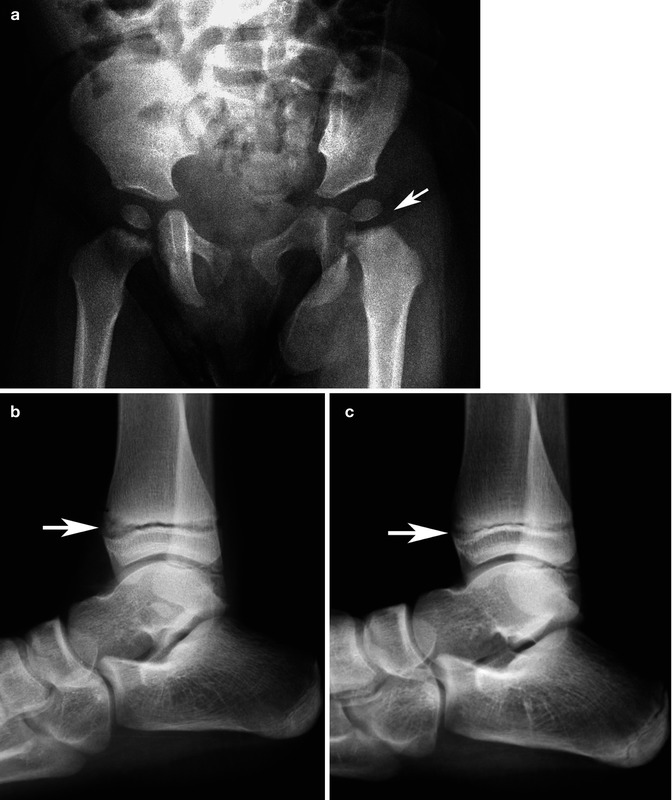
Fig. 4.1
Fractures peculiar to children. (a) Typical buckle fracture. (b) Greenstick fracture. (c) Plastic bowing fracture. (d) Salter–Harris epiphyseal metaphyseal fracture with a displaced epiphysis (arrow)
Buckle or torus fractures are simple axial load induced compression fractures which manifest as buckling, kinking, or notching of the cortex. They occur most frequently in the metaphyseal regions of long bones, for this is where the cortex is weakest. Some of these fractures are quite subtle, but if one follows the rule that the distal ends of the long bones should have smooth, continuous curves, then one will not accept even the slightest bump, dent, buckle, or angled cortex as normal. In this regard, there are two types of buckle/torus fractures [3].
The first type of buckle fracture is the typical buckle fracture which results in outward buckling/bulging of the cortex (Fig. 4.2), but equally common is the second type of buckle fracture which presents as unilateral angled buckling of the subepiphyseal metaphyseal cortex (Fig. 4.3). In the first case, the buckling results from a direct axial load transmitted down the length of the bone with an abrupt deceleration (i.e., the outstretched upper or lower extremity). With such abrupt deceleration the bone of the metaphysis impacts and crumbles/buckles. The trabeculae are compressed and outward bulging of the cortex through the metaphysis occurs (Fig. 4.2b). With the angled buckle fracture, the axial load is shifted off center, and as a result, the cortex buckles, in an angled configuration, to one side or another (Fig. 4.3d). In actual fact this fracture is the precursor of a frank Salter–Harris II fracture.
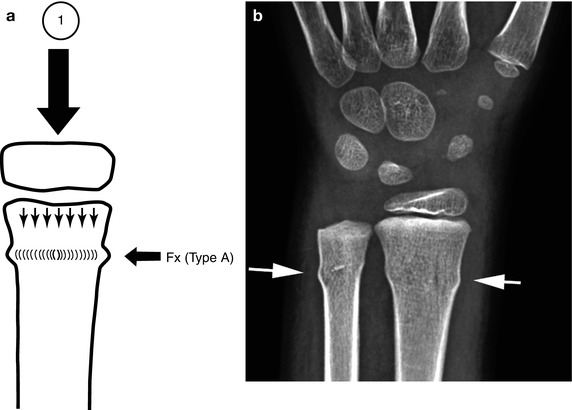
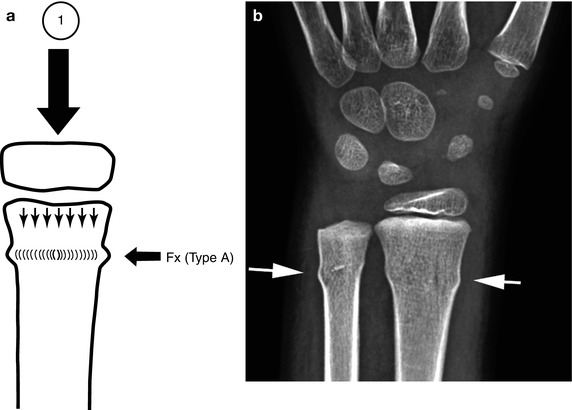
Fig. 4.2
Buckle fracture type (a) Axial loading forces (1) are exerted down the length of any given bone. The result is a cortical buckle fracture (fx). (b) Typical type A buckle fractures of the radius and ulna (arrows)
Fig. 4.3
Buckle fracture type B. (a) Axial loading forces (1) are exerted down the length of the bone. However, other forces such as valgus also are at play. (b) This results in shifting of the axial load axis (3) and compression of the underlying metaphysis (2). (c) The same laterally placed axial loading forces (3) eventually result in an angled buckle fracture (fx). (d) Typical angled buckle fracture of the distal radius (arrow). Compare with the smooth cortex over the anterior aspect of the radius
Greenstick and plastic bending/bowing fractures are related, both resulting from axial loading forces exerted along the long axis of a long bone. In infants and young children, because the bones are soft, before actually fracturing, plastic bending (bowing) occurs. Thereafter, if the forces are stronger, the plastic bending fracture becomes a “greenstick” fracture (Fig. 4.4). The term “greenstick” comes from the comparison of this type of fracture to the manner in which a “green,” supple tree branch breaks if it is bent. It can be bent only so far, and then it snaps and breaks. Most often plastic/bending fractures occur in the forearm [4–6]. However, they are also very common in the clavicle. They are less common in the fibula [7]. These fractures are discussed in more detail in later sections, but it might be noted at this point that seldom, if ever, do these fractures show classic signs of healing. In other words, whereas with a greenstick fracture, one sees healing sclerosis and periosteal new bone formation, with the usual bending fracture, nothing but the persisting deformity is seen.


Fig. 4.4
Plastic/greenstick fractures. (a) Note typical greenstick fractures through the distal radius and ulna (arrows). (b) In this patient, a greenstick fracture is present through the midshaft of the ulna (arrow). A plastic bending fracture is present in the radius. (c) This patient demonstrates only a plastic bending fracture of the radius (arrows)
Epiphyseal–metaphyseal fractures are very common in childhood and, of course, occur exclusively in the child. Because the junction between the epiphysis and metaphysis is a weak area, if a shearing/twisting force is applied to the end of a long bone, it is quite natural that epiphyseal–metaphyseal slippage or separation would occur. A variety of injuries can be sustained at this junction, and to facilitate their understanding and categorization, the Salter–Harris classification of five types [8] usually still is employed (Fig. 4.5). Even though other more complicated classifications have been suggested, this basic classification still is most useful.
Fig. 4.5
Salter–Harris injuries. Note typical displaced and non-displaced Salter–Harris I through V fractures
As far as the radiologist is concerned, the greatest challenge comes from Salter–Harris type I and II injuries. The reason for this is that if in these cases, the epiphysis is not displaced, bony changes are subtle, and one must rely more on soft tissue changes and widening of the epiphyseal line (Fig. 4.6). Salter–Harris type III and IV fractures usually are relatively easy to detect, for most often some degree of epiphyseal displacement exists and, in any case, the fracture lines are more readily visible. Type III fractures occur most commonly in the distal tibia, followed by the small bones of the hands and feet.