and Siddharth P. Jadhav2
(1)
Department of Radiology, University of Texas Medical Branch Pediatric Radiology, Galveston, TX, USA
(2)
The Edward B. Singleton Department of Pediatric Radiology, Texas Children’s Hospital, Houston, TX, USA
Abstract
This chapter provides an overview of infection, inflammations, and infarctions as they affect the musculoskeletal system. The objective is to present an overview so that each of these entities is not repeated in other chapters. Discussion centers on osteomyelitis, pyomyositis, cellulitis, fascitis, and infarction. MRI is emphasized for infections and tumors.
Osteomyelitis, Pyomyositis, and Cellulitis/Fascitis
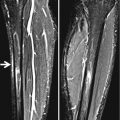
Roentgenographic bony changes in osteomyelitis take 10 days to 2 weeks to develop; therefore, in the early stages, one can only infer the diagnosis from soft tissue changes. Osteomyelitis manifests in deep soft tissue edema as does pyomyositis, while superficial cellulitis demonstrates findings reflecting superficial edema (Fig. 2.1). Because of this, deep edema should suggest the presence of osteomyelitis or pyomyositis until proven otherwise.
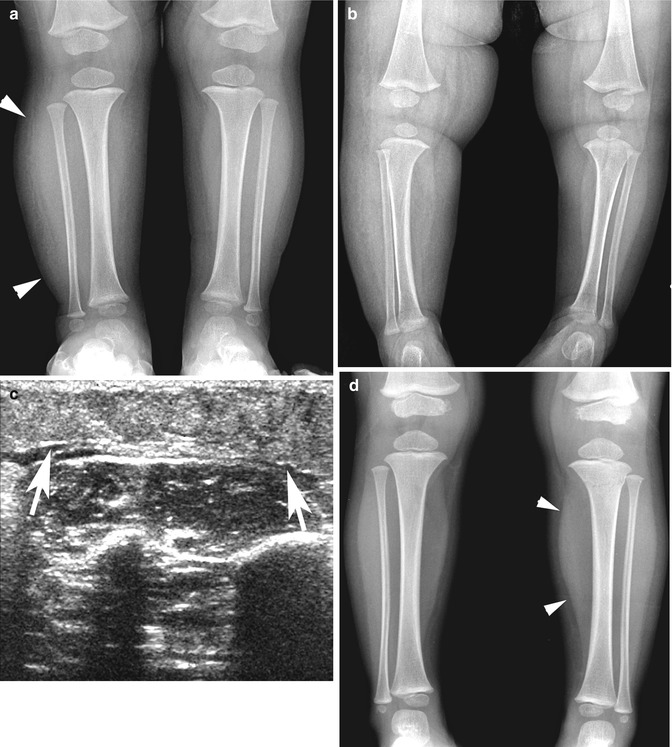
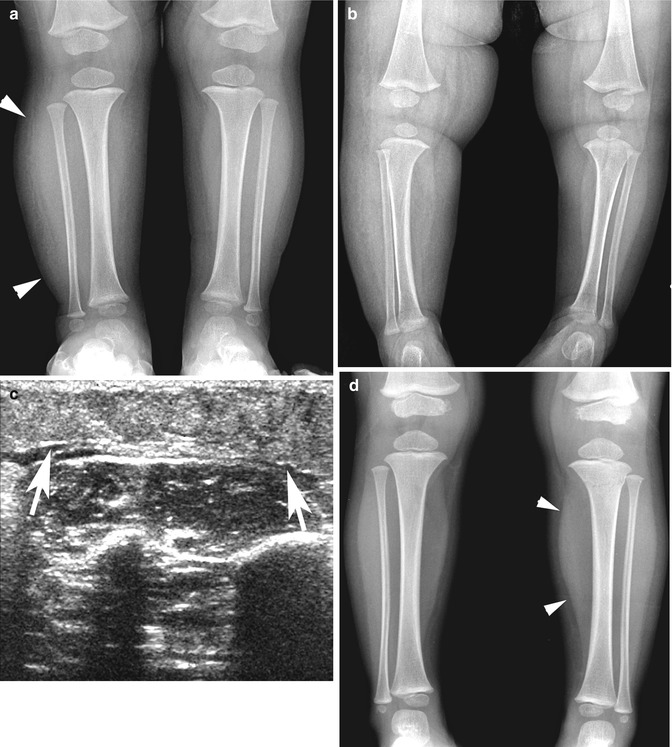
Fig. 2.1
Superficial versus deep edema. (a) Superficial edema. Cellulitis of right leg. Note the swollen leg (arrowheads). The subcutaneous soft tissues are reticulated but the muscle is still visible as a distinct structure. (b) Another patient with superficial edema/cellulitis. Note the swollen right leg, reticulated subcutaneous fatty tissue with preservation of the muscle. (c) Ultrasound in the same patient. Note the nodular, heterogeneous appearance of subcutaneous cellulitis (arrows). (d) Deep edema. Note the expanded deep muscle compartment (arrowheads) in the left leg. The subcutaneous soft tissues are intact. This patient had an upper tibial fracture, and the resultant bleeding and edema caused the deep compartment to expand
After 10–14 days, bony destruction is seen and can manifest as an acute destructive process or a low-grade smoldering problem (low-grade osteomyelitis), which frequently mimics entities such as Ewing’s sarcoma and eosinophilic granuloma [1]. More aggressive permeative and “moth-eaten” changes are seen with the former, while with the latter, more reactive bone healing or sclerosis is seen. In addition, although osteomyelitis usually is a metaphyseal problem, it can involve the epiphysis [2, 3]. All of these variations are demonstrated in Fig. 2.2.
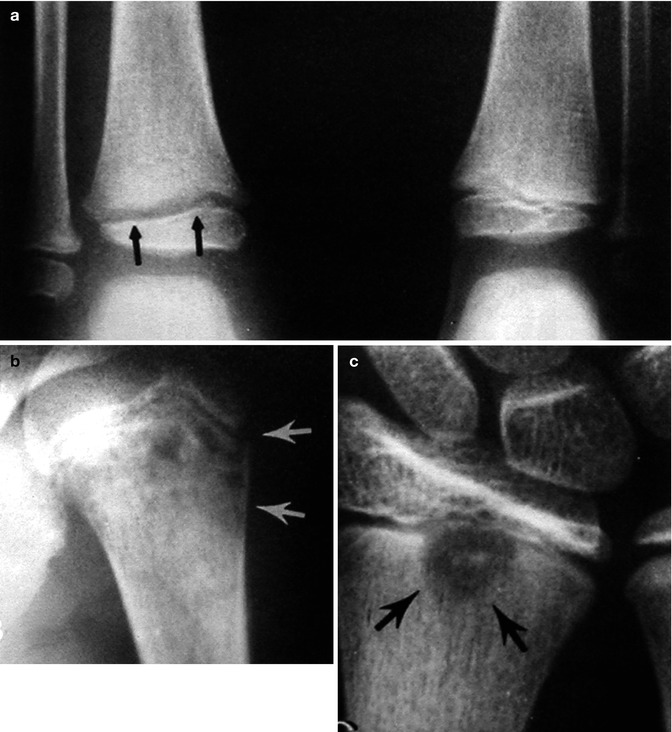
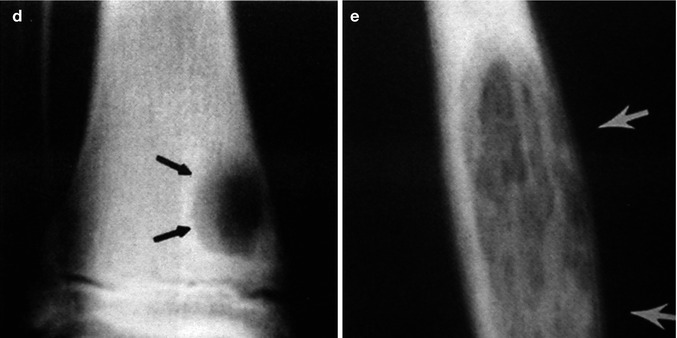
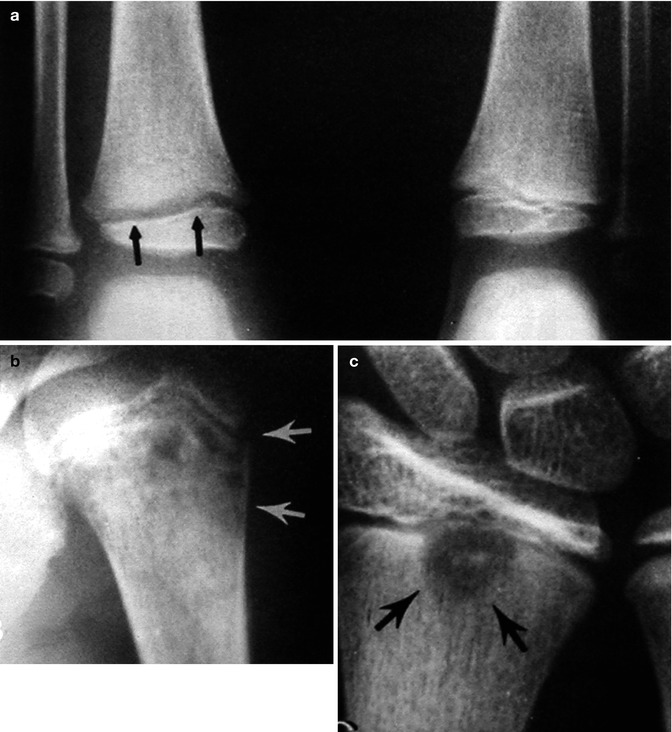
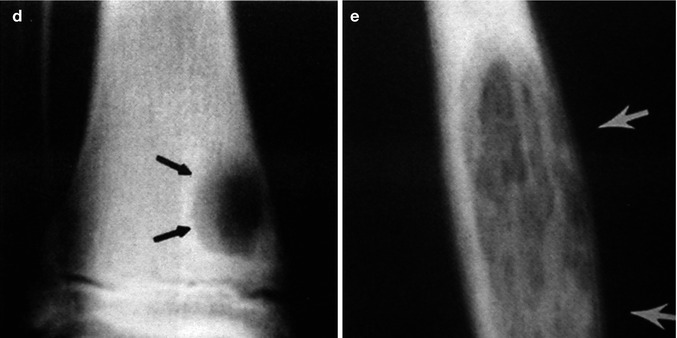
Fig. 2.2
Osteomyelitis, various configurations. (a) In this patient there is widening of the epiphyseal plate (arrows) due to juxta bony resorption without any significant metaphyseal destruction. (b) This patient demonstrates typical permeated metaphyseal bone destruction (arrows). (c) Less common presentation. Note the focal, relatively distinct area of bony destruction (arrows) extending into the epiphysis. (d) Low-grade osteomyelitis (arrows) mimicking a nonossifying fibroma or cyst. (e) Low-grade diaphyseal osteomyelitis. Note bony expansion, widespread destruction, and loss of cortex (arrows) in this patient with low-grade diaphyseal osteomyelitis. The findings mimic Ewing’s sarcoma or eosinophilic granuloma
If one suspects the presence of osteomyelitis clinically but plain film changes do not support the diagnosis, one should turn to nuclear scintigraphy or MR. With nuclear scintigraphy, the findings are nonspecific but helpful. It should be remembered, however, that the pyrophosphate bone scan measures reactive (healing) bone activity and not bone destruction or the development of a purulent exudate. It is for this reason that in some cases imaging with gallium- or indium-labeled white blood cells [4] may be required to determine whether an infection is present. Finally it should be remembered that in many cases, the technetium bone scan, in the very early stages of the infection, may appear falsely normal [5]. The reason for this is that in such early stages of infection (osteomyelitis), there is so much congestion of the bone marrow by the developing infection that blood flow, and hence the delivery of isotope to the bone (marrow), is impaired. Usually within 24–48 h the bone scan becomes positive. Because of this, if one can make the presumptive diagnosis of osteomyelitis on the basis of clinical and plain film roentgenographic (deep edema) findings, one should assume that such infection is present and begin therapy. The bone scan, delayed a day or two, then will become positive [6].
Ultrasonography also has been used to detect osteomyelitis [7], but the changes demonstrable with ultrasound are usually late changes. They consist of purulent exudate elevating the periosteum from the cortex of the involved bone (Fig. 2.3). They are not very easy to demonstrate, and so overall, MR is becoming more and more popular for the evaluation of occult osteomyelitis where the normal high signal of marrow fat on T1-weighted images is lost, and on the proton-density and T2-weighted images, increased signal is seen (Fig. 2.4).
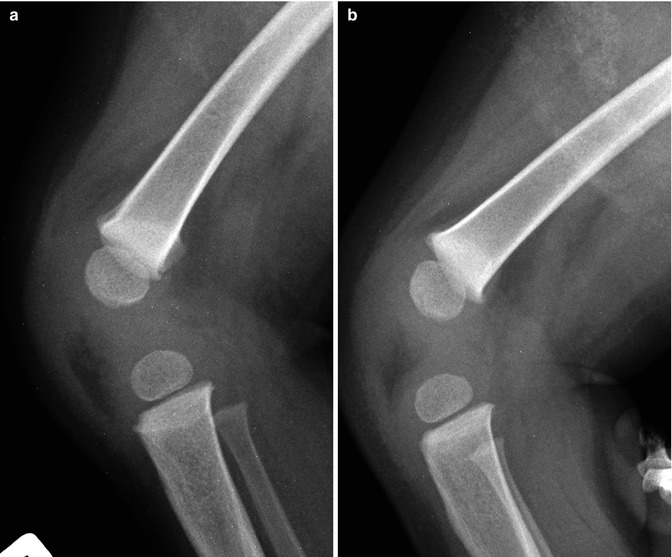


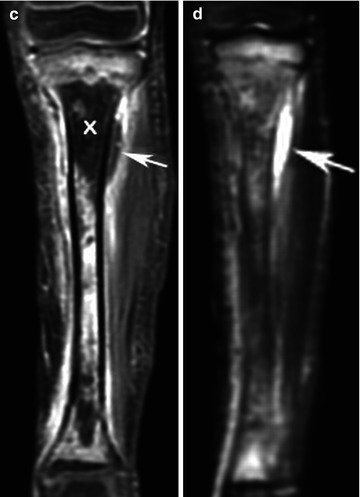
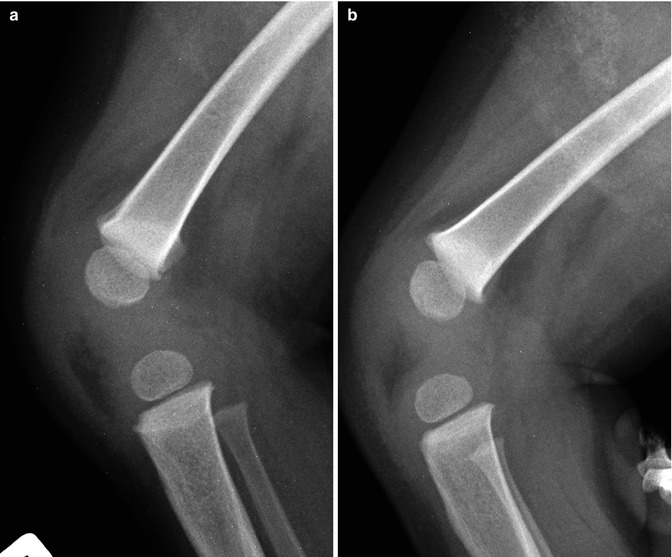

Fig. 2.3
Acute osteomyelitis. Note indistinct fat/soft tissue planes both anterior and posterior to the distal femoral metaphysis. This signifies deep edema. (b) Normal side. Compare the normal distinct fat pads with those in (a). (c) Ultrasound through the distal femur demonstrates a defect in the metaphysis (arrow) just above the epiphyseal plate. Also note the subperiosteal purulent material/abscess anterior to the distal cortex (arrowheads). (d) Later radiograph demonstrates typical bony destruction (arrow)

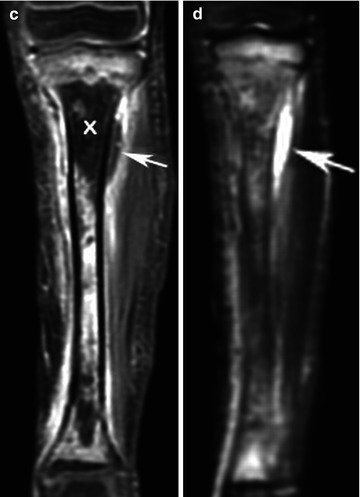
Fig. 2.4




Acute osteomyelitis, MR findings. (a) In this patient, there is subtle permeative bony destruction (arrow) in the distal tibia. (b) Coronal STIR MR image demonstrates increased signal in the distal tibia (arrowhead) and increased signal in subperiosteal fluid/exudate accumulation medially (arrows). (c) Coronal MR, gadolinium-enhanced image. Note high signal in the femoral shaft and in the surrounding soft tissues. The proximal epiphysis also has high signal all of which indicates inflammation. Loss of signal in the proximal tibia (X) indicates bone infarction and the arrow points to the early collection of associated subperiosteal purulent exudate. (d) Coronal MR, STIR image. Note high signal (arrows) in the purulent exudate collection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree