and Siddharth P. Jadhav2
(1)
Department of Radiology, University of Texas Medical Branch Pediatric Radiology, Galveston, TX, USA
(2)
The Edward B. Singleton Department of Pediatric Radiology, Texas Children’s Hospital, Houston, TX, USA
Abstract
This chapter deals with injuries of the knee and leg. Various types of fractures and other injuries are presented. MR is discussed where it significantly adds to evaluation of these injuries.
Normal Fat Pads and Soft Tissues
There are a number of normal fat pads around the knee, and all can be useful. On frontal view, these fat pads are seen adjacent to the distal femur (Fig. 10.1a) and can become obliterated with deep edema. On lateral view, similar fat pads are seen posterior to the distal femur (Fig. 10.1b). Other fat pads include the prefemoral fat pad just over the anterior surface of the distal femur, the infrapatellar or Hoffa’s fat pad inferior to the patella, and the suprapatellar fat pad which exists between the insertion of the quadriceps tendon and the neck of the suprapatellar joint bursa (Fig. 10.1b). The infrapatellar fat pad commonly is obliterated by the edema associated with Osgood–Schlatter and Sinding–Larsen–Johansson disease. With prepatellar cellulitis, the soft tissues anterior to the quadriceps tendon, patella, and infrapatellar tendon become thickened and trabeculated. In the normal knee, the infra- and suprapatellar tendons usually are clearly identified (Fig. 10.1b).
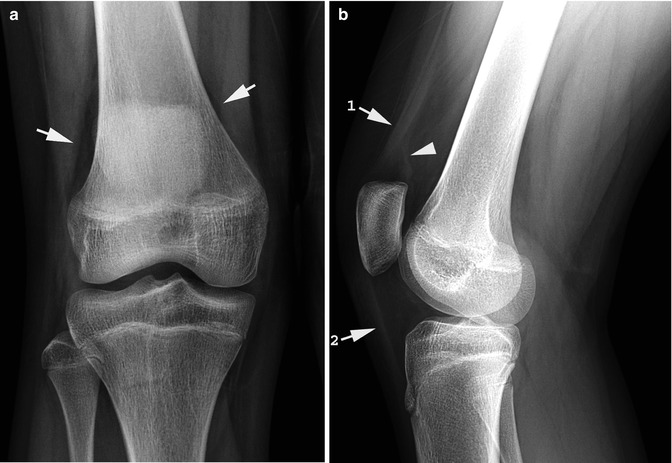
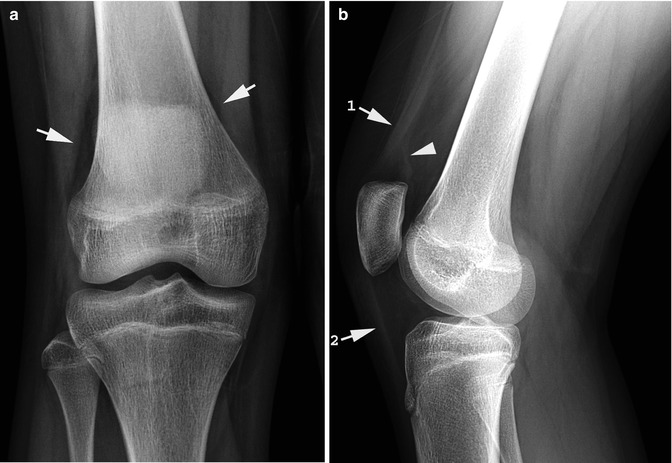
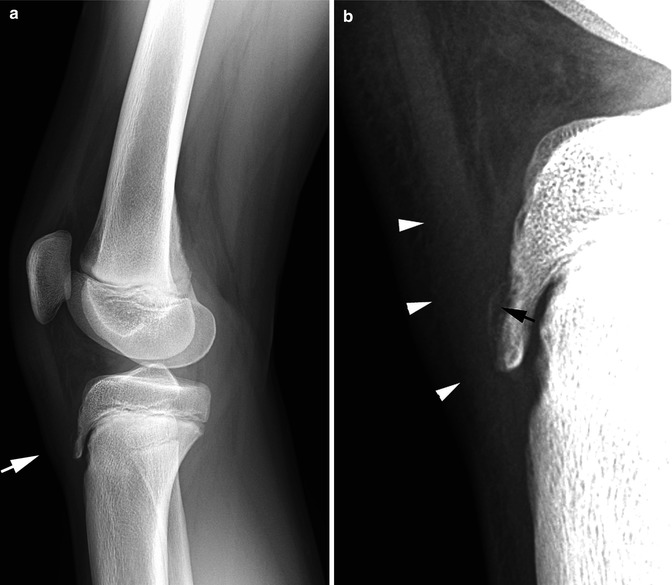
Fig. 10.1
Normal fat pads and soft tissues. (a) Note the normal fat pads (arrows) along the distal femur. (b) Lateral view. Note the quadriceps tendon (1), the infrapatellar tendon (2), and the neck of the suprapatellar bursa (arrowhead). Also note the fat pads anterior and posterior to the distal femur. The infrapatellar or Hoffa’s fat pad lies directly behind the infrapatellar tendon. The small triangular-shaped suprapatellar fat pad lies between the insertion of the quadriceps tendon and the neck of the suprapatellar bursa
Detection of Fluid in the Knee Joint
The knee joint does not widen significantly with accumulations of fluid, and thus one must depend on surrounding soft tissue and fat pad changes for the detection of fluid in the knee joint [1]. In this regard, it is the lateral view of the knee that is most useful. On this view, fluid almost always first visibly accumulates in the suprapatellar bursa, which lies behind the quadriceps tendon and in front of the prefemoral fat pad. If this occurs, the quadriceps tendon is displaced anteriorly and the fat pad posteriorly, and the fluid-filled suprapatellar bursa blends with the quadriceps tendon to make it look thicker than normal (Fig. 10.2).


Fig. 10.2
Joint fluid: suprapatellar bursa. Note the distended suprapatellar bursa (arrows) compressing the anterior femoral fat pad. It blends with the quadriceps tendon making the tendon appear thicker than normal
Fluid in the knee also is detectable with ultrasound, CT, and MR imaging. Ultrasound, however, is noninvasive and easily demonstrates the presence of knee joint fluid. However, because plain films are so dependable, seldom is there need for any of these studies to be performed for the sole purpose of detecting fluid in the knee joint.
Injuries of the Distal Femur and Proximal Tibia and Fibula
Cortical buckle (torus) fractures around the knee are uncommon in older children because the cortices of both the distal femur and proximal tibia are sturdy. However, in infants and young children, they are common both in the distal femur and proximal tibia (Fig. 10.3). These fractures can result from simple axial loading injuries but also commonly are seen with hyperextension injuries. In this regard, in the upper tibia, buckle fracturing of the anterior tibial cortex along with an associated posterior diastatic hairline fracture is common [2–5] and often due to a trampoline-induced injury [6]. In such cases, when one falls off the trampoline, the fall is braced with the hyperextended lower extremity and stresses are placed on the upper tibia (Fig. 10.4a, b). On AP view of the knee, one may see a transverse (Fig. 10.4c) or slightly oblique fracture which often is hairline. In addition, visualizing this fracture on the AP view probably occurs in less than 50 % of cases. In some cases, an associated cortical buckle fracture is seen (see Fig. 10.5c).

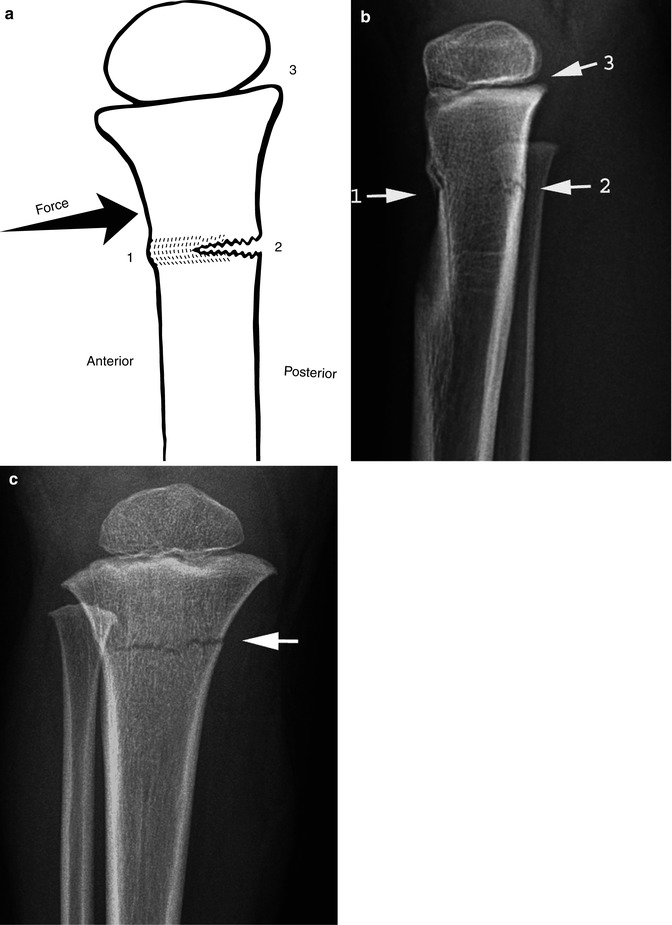
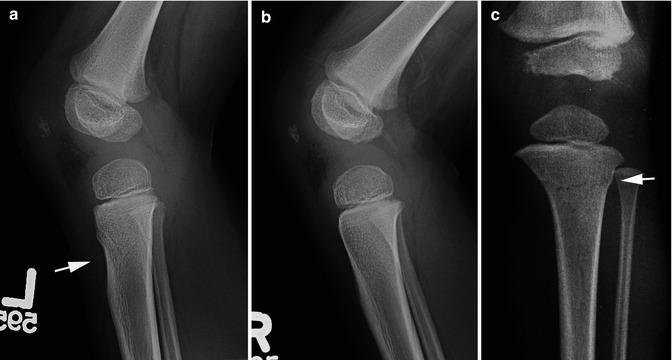

Fig. 10.3
Distal femoral and proximal tibial buckle fractures. (a) Note the typical impacted buckle through the distal femur (arrows) with early healing. (b) Lateral view demonstrates the same impacted fracture (arrow). (c) Note the very subtle angled buckle fracture through the posterior cortex (arrow) of the proximal tibia. (d) Normal side for comparison. Note the smooth curving appearance of the posterior tibial cortex
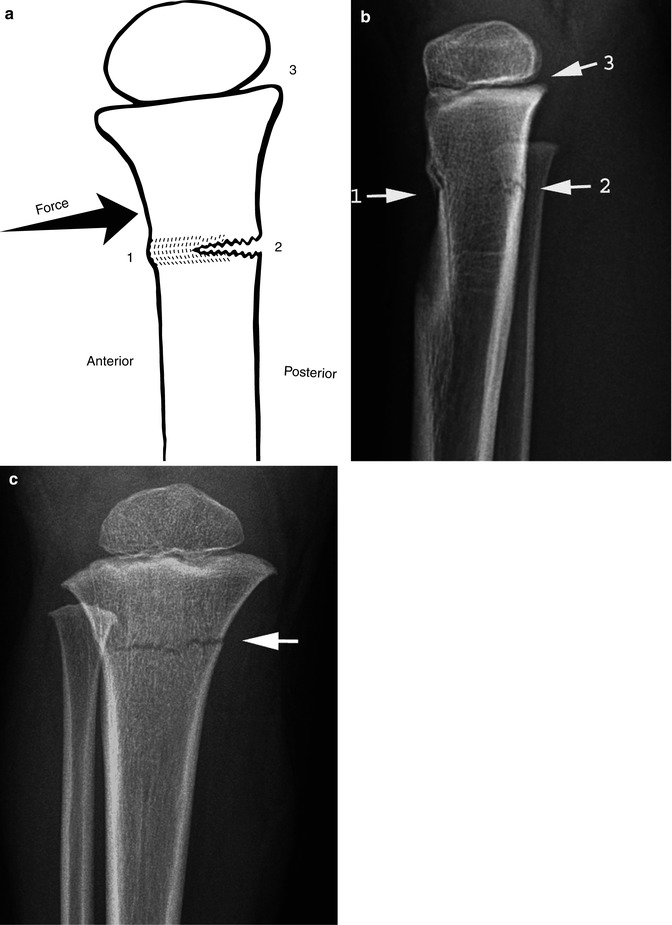
Fig. 10.4
Upper tibial impaction fracture: toddler II fracture. (a) Anterior compressive force is exerted on the upper tibia with hyperextension of the knee to produce: (1) an anterior buckle fracture, (2) a diastatic posterior fracture, and (3) anterior tilting of the epiphyseal plate. (b) Typical imaging findings. First note the anterior buckle fracture (1) and then note the subtle posterior diastatic fracture (2). Finally note anterior tilting of the epiphyseal plate (3). (c) Typical transverse upper tibial fracture line (arrow)
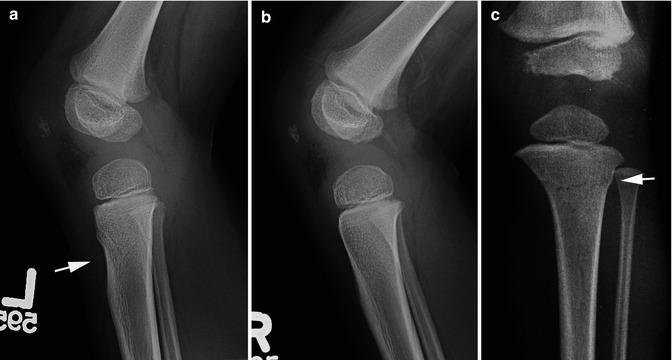
Fig. 10.5
Toddler II fracture: subtle findings. (a) In this patient, the main finding is increased scalloping of the concavity for the tibial tubercle (arrow). A minimal buckle fracture exists a little higher. (b) Normal side for comparison. Note the normal appearance of the cortex of the upper anterior tibia. (c) Another patient. Note the subtle hairline transverse fracture and the very minimal associated buckle fracture (arrow)
All of the foregoing notwithstanding, in most cases, it is the lateral view of the knee which is most informative with this fracture where the findings consist of (1) buckling of the anterior tibial cortex, (2) increased concavity of the notch for the tibial tubercle, (3) anterior tilting of the epiphyseal plate, and (4) posterior diastatic fracture (Fig. 10.4b). In many cases, these findings are very subtle and comparative views are invaluable (Fig. 10.5a, b). This fracture is very common in infants and young children, and we have arbitrarily named it the toddler II fracture and the spiral fracture described by Dunbar (see Fig. 10.28) as the toddler I fracture.
Upper tibial transverse fractures also can result from lateral forces applied to the knee, and both this fracture and the toddler II fracture can result in a valgus deformity of the tibia [7–10]. This deformity, often initially minimally present, can become more pronounced and persistent as time goes by (Fig. 10.6). For the most part, this is believed to result from the fact that there is overgrowth of the medial aspect of the proximal tibia. In this regard, it has been noted that normally there is a greater blood supply to the upper medial tibia and that, with the hyperemia associated with fractures, the growth accelerated and overgrowth occur [8, 9].
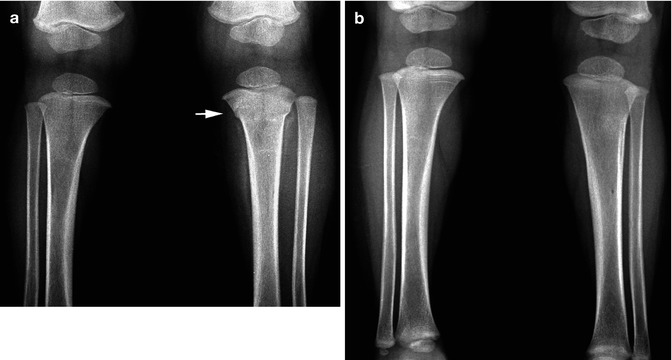
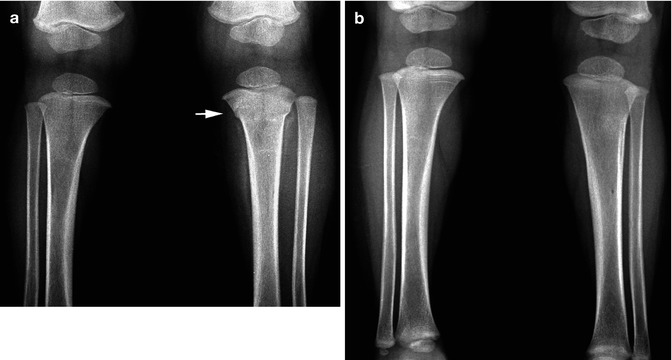
Fig. 10.6
Upper tibial fracture: valgus deformity. (a) Note a typical impacted buckle tibia fracture (arrow). (b) With healing, the fracture becomes obliterated, but a valgus deformity of the tibia is present
Epiphyseal–metaphyseal injuries are not that common about the knee but do occur. In gross form, they are not difficult to detect, but the more subtle, nondisplaced Salter–Harris type I and II injuries frequently elude initial observation. In these cases, one should be suspicious of the slightest degree of widening of the epiphyseal plate (Fig. 10.7a). Comparative views are very helpful and it must be emphasized that positioning must be accurate for the slightest malpositioning of the knee may erroneously suggest a wide epiphyseal plate.
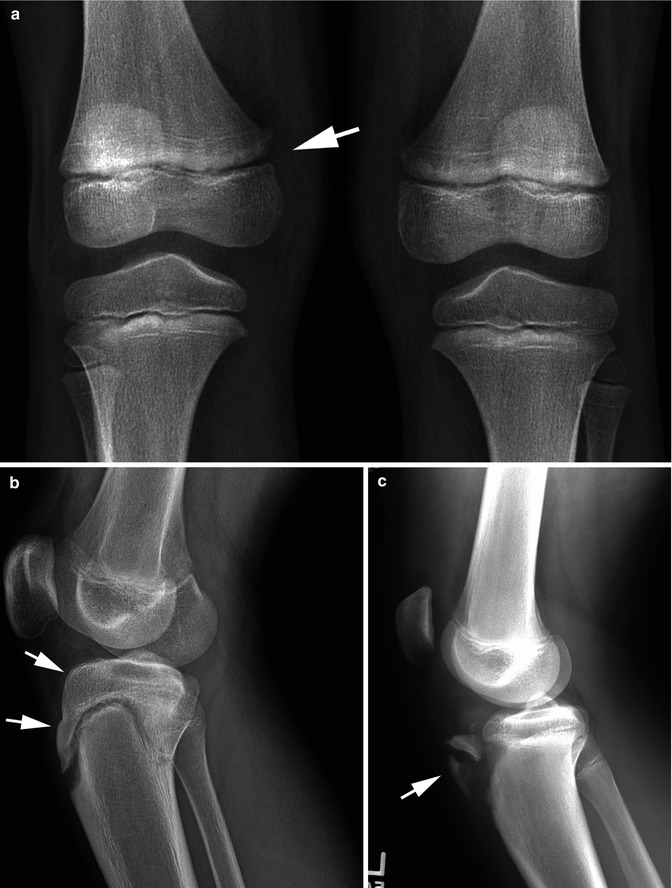
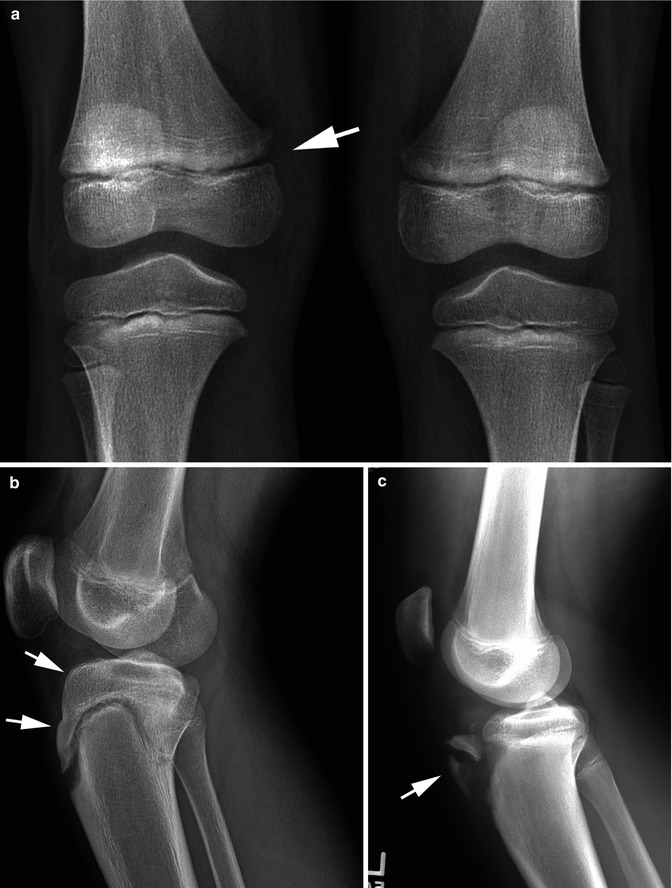
Fig. 10.7
Epiphyseal–metaphyseal fractures. (a) Note subtle widening of the epiphyseal plate in the right distal femur (arrow) constituting a minimal SH I fracture. (b) Tibial epiphyseal avulsion. Note the avulsed tibial epiphysis along with that portion which extends over the anterior tibia (arrows). There is a posterior compression fracture present also. (c) In this patient, only partial avulsion of the tibial epiphysis (arrow) has occurred
A variation of the usually Salter–Harris fracture is the one which occurs when the proximal tibial epiphysis is totally or partially avulsed (Fig. 10.7b, c) and finally MR imaging is especially useful in detecting epiphyseal metaphyseal injuries which are occult or invisible on plain films (Figs. 10.8 and 10.9). MRI has been shown to change management in cases of epiphyseal–metaphyseal injuries by better defining the extent of the fracture and in some cases by diagnosing unsuspected fractures [11].
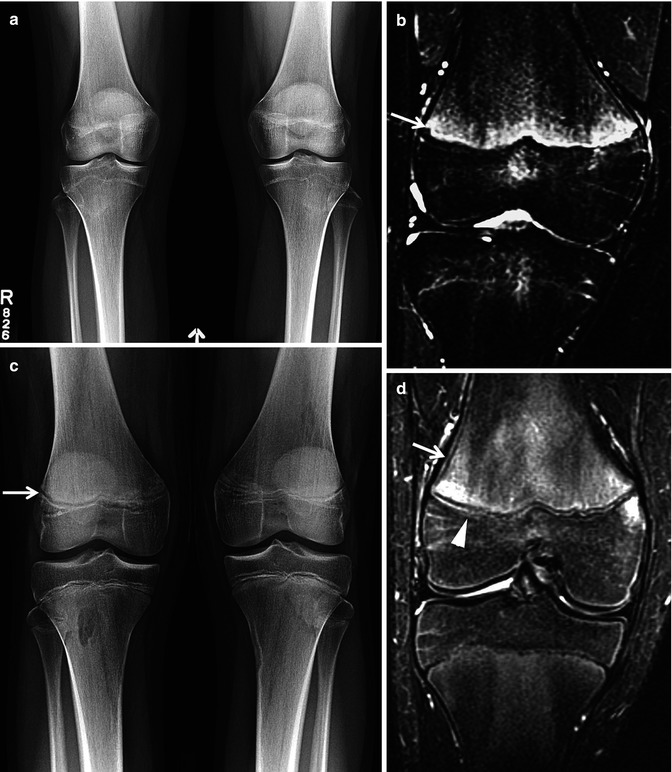
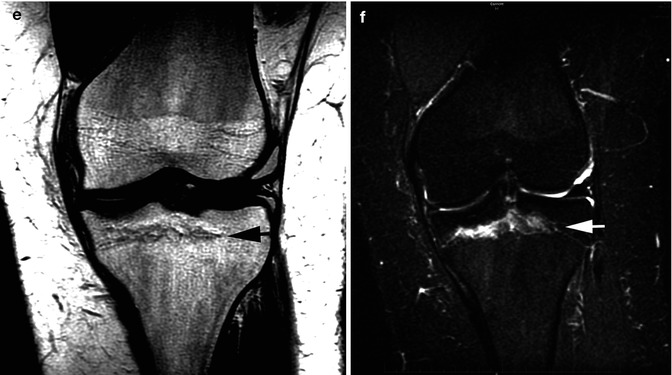
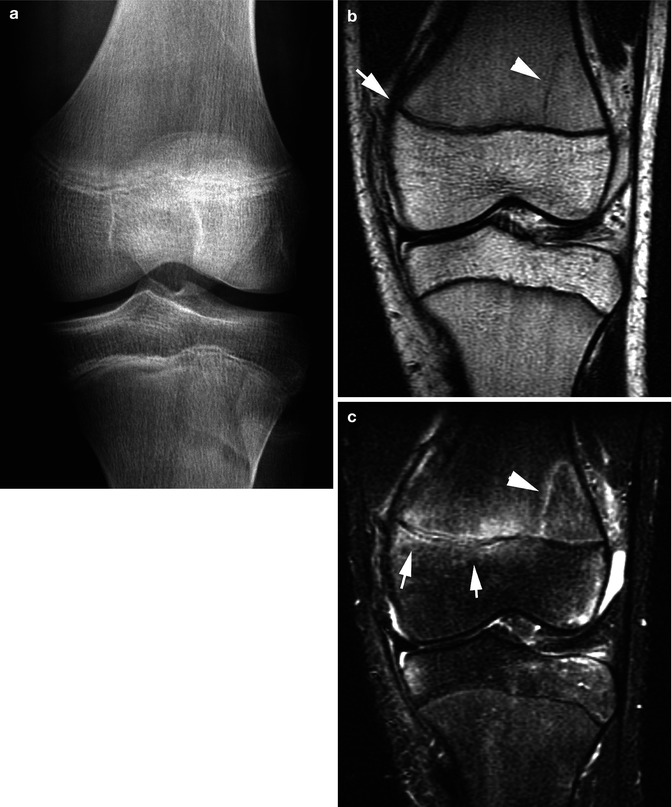

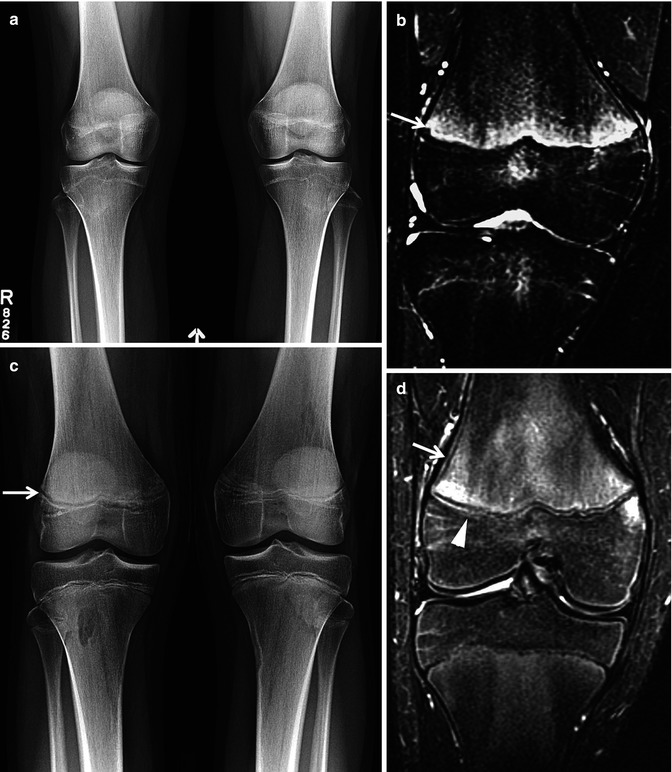
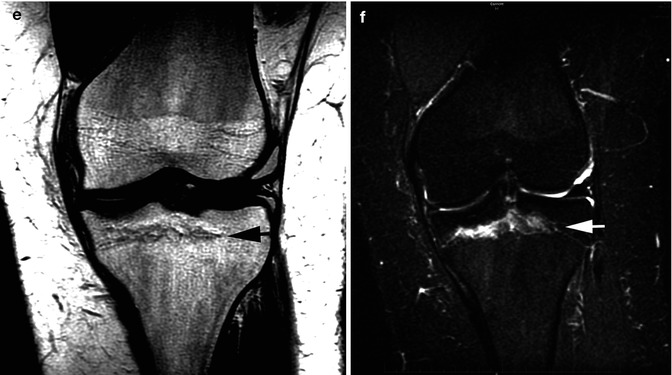
Fig. 10.8
Occult epiphyseal–metaphyseal fractures: value of MR. (a) Frontal radiograph of both knees is normal with no evidence of physeal widening. The patient had pain in the right knee. (b) Coronal STIR image in the same patient shows edema in the physis which extends into the metaphysis (arrow) consistent with a nondisplaced Salter–Harris I injury. (c) Another patient with frontal radiographs suggesting mild physeal widening in the right distal femur (arrow). MRI was obtained for confirmation and to exclude internal derangement of the knee. (d) Coronal STIR image confirms the finding of widening of the growth plate (arrowhead). Also note high-signal metaphyseal edema adjacent to the widening epiphyseal plate and fluid/hemorrhage extending subperiosteally along the lateral aspect of the metaphysis (arrow). (e) In this patient, the epiphyses basically were closed and the plain films were normal. On the T1-weighted image, there is irregularity along the old epiphyseal plate region (arrow). (f) Coronal STIR image demonstrates increased epiphyseal plate signal indicating a mild Salter–Harris fracture
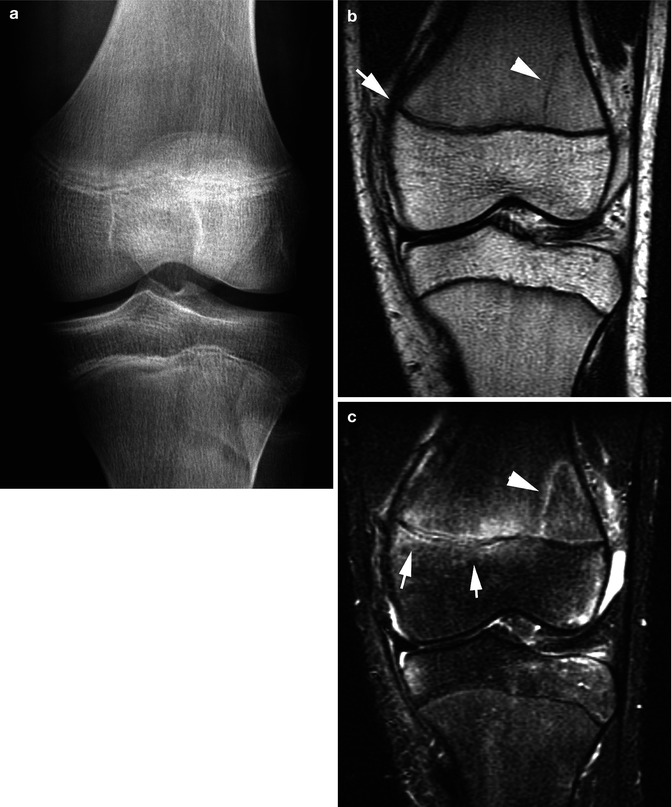

Fig. 10.9
Occult epiphyseal–metaphyseal fractures: value of MR. (a) Left knee pain. AP view of the left knee is normal. (b) Coronal T1-weighted image demonstrates a subtle Salter–Harris II fracture (arrowhead) and subtle widening of the epiphyseal plate medially (arrow). (c) Coronal STIR image. Note the high signal in the fracture line (arrowhead) of the Salter–Harris II fracture. In addition, note increased signal in the medial part of the epiphyseal plate and high signal (bone bruises) in the adjacent metaphysis and epiphysis (arrows). (d) Another patient with knee pain. Frontal and lateral views of the knee show no evidence of fracture. A small joint effusion is seen on the lateral view (arrow). (e) Sagittal T1W image shows a Salter–Harris II fracture of the distal femur (arrow). (f) Coronal STIR image shows widening of the lateral aspect of the physis (arrow) and adjacent high-signal metaphyseal edema. Also note metaphyseal extension of the fracture (arrowhead)
Stress fractures around the knee most commonly occur in the upper tibia in older children. A fracture line usually is not visible but with healing typical sclerosis and periosteal new bone deposition are seen posteriorly (Fig. 10.10a). In the early stages, these changes can be subtle, but later periosteal new bone deposition is profound, and often a more serious lesion such as a bone tumor is erroneously suggested. Less commonly stress fractures occur in the upper anterior tibia, and both of these fractures are the equivalent of the toddler II fracture seen in infants and young children. The findings in the latter fracture usually consist of focal sclerosis in the upper anterior tibia (Fig. 10.10b–d). All of these findings also can be demonstrated with CT and MR where the occult fracture line often becomes visible. MR is valuable in differentiating stress reaction from stress fracture which has therapeutic implications with stress fractures requiring longer activity modification and rest.

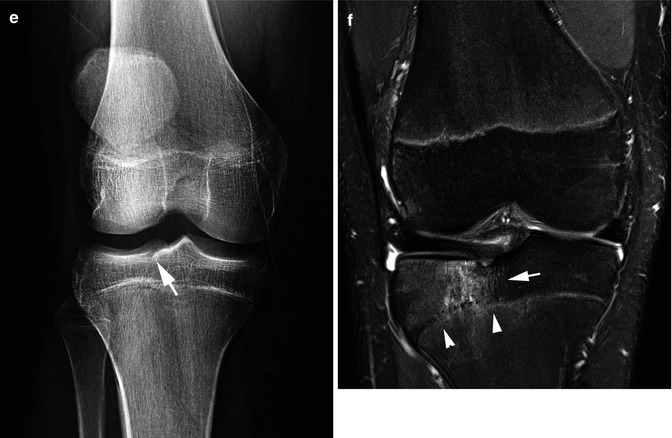

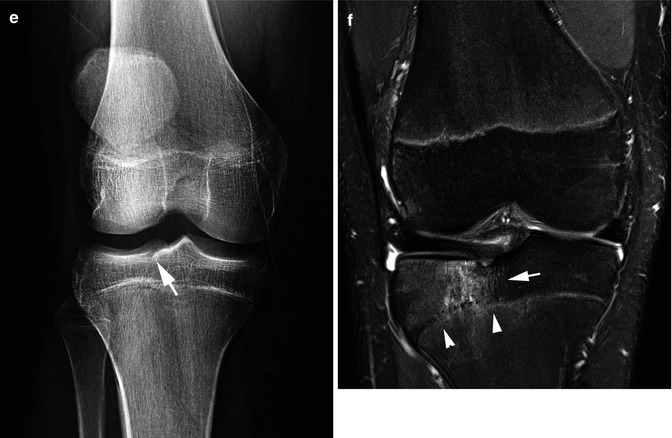
Fig. 10.10
Stress fracture. (a) Typical upper tibial stress fracture manifesting in cortical thickening and periosteal new bone deposition over the upper posterior tibia (arrow). Note that subtle sclerosis extends to the anterior cortex. (b) In this patient, a vague crescentic sclerotic line (arrows) is noted in the upper tibia. (c) Lateral view demonstrates that the line is secondary to an impaction stress fracture (arrow) of the upper anterior tibia. (d) Normal side for comparison. Note the normal appearance of the upper tibia with no visible sclerosis. (e) Compression tibial plateau. AP view of the knee is basically normal. There is minimal suggestion of a fracture (arrow). (f) Coronal T2 fat-saturated image demonstrates the compression fracture (arrow) of the tibial epiphysis and associated disruption of the epiphyseal plate (arrowheads)
Although not true stress fractures, impaction fractures of the distal femurs and proximal tibia can be considered within the ball park of stress fractures. In this regard, it is the tibia more often than the femur which is involved. Most often an axial loading force is exerted on the knee, and in most cases, the plain films are basically are normal. However, MR usually demonstrates the area of impaction (Fig. 10.10e, f).
Patellar Fractures and Dislocations
Patellar fractures and dislocations are common. Overt fractures usually occur from direct blows to the patella and occasionally from acute quadriceps tendon stress-induced injuries (Fig. 10.11). In these latter cases, the proximal half or third of the patella is avulsed from the remainder of the patella, and the findings are readily recognizable.


Fig. 10.11
Patellar fractures. (a) Note the linear fracture (arrow) through the patella. (b) In this patient, two linear fractures (arrows) are visualized. (c) Patellar bone bruise. With a direct hit to the patella, increased signal in the inferior patella (arrow) is seen on this STIR image. (d) Coronal STIR image demonstrates the same increased signal (arrow)
In terms of patellar dislocations, both acute and chronic repetitive dislocations of the patella are common in childhood, but in most cases, the patella relocates before radiographs are obtained. Patellar dislocations usually result from twisting of the knee wherein the medial ligamentous stabilizers (retinacula) rupture and the medial margin of the patella strikes against the lateral femoral condyle [12]. In some cases of patellar dislocation, an avulsed fracture fragment is seen along the medial aspect of the patella (Fig. 10.12a). Transient patellar dislocation often results in a large hemarthrosis making clinical examination difficult. Often an ACL rupture is erroneously suspected clinically, and an MRI is ordered which reveals the correct diagnosis. With MR imaging the retinacular injury, the avulsed bony fragment, and bone bruises involving the medial margin of the patella and lateral femoral condyle are readily demonstrable (Fig. 10.12b–d). Finally, it should be noted that the avulsed medial patellar fracture fragment is not mobile and usually stays in one position. In addition, it often is the only finding seen in cases of patellar dislocation with subsequent relocation.
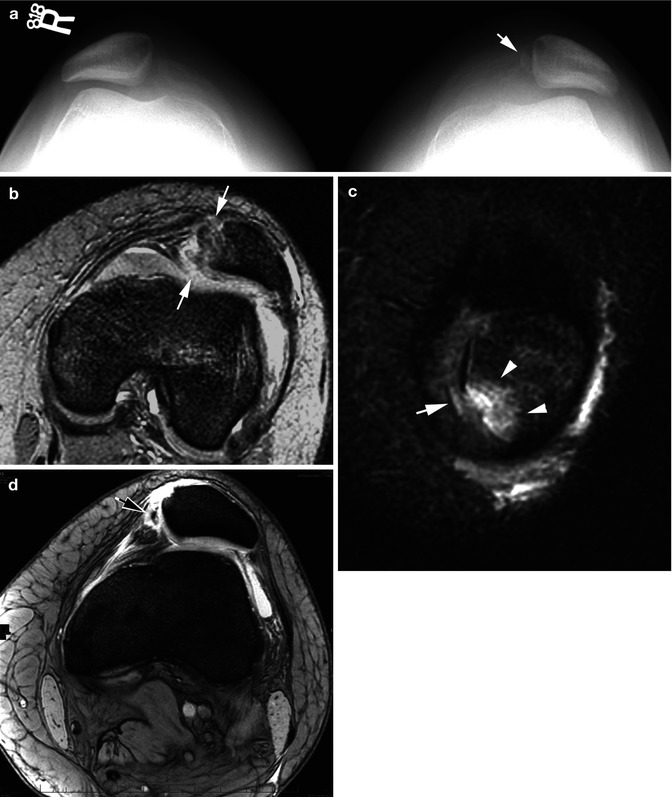
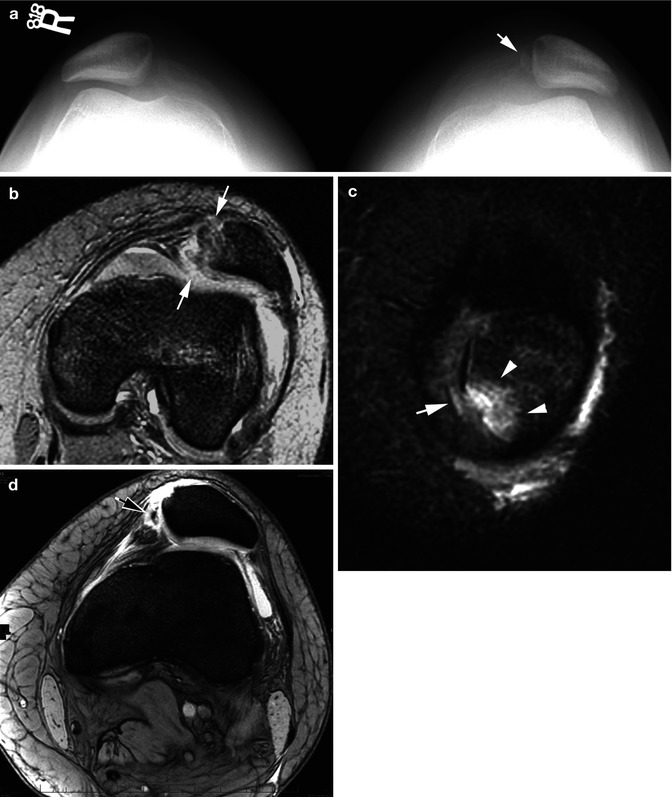
Fig. 10.12
Patellar dislocation: medial retinacular tear and fracture. (a) On this skyline view, note that both patellae are subluxed and that the intercondylar notches are shallow on both sides. In addition, there is a subtle avulsed medial fracture fragment (arrow) on the left. There also is surrounding swelling. (b) Axial T2 GRE study demonstrates the disrupted medial retinaculum (arrows). (c) Coronal STIR image through the patella demonstrates the avulsed fracture fragment (arrow) and a bone bruise in the medial patella (arrowheads). (d) Another patient. Coronal T2 view of the knee. Note the avulsed medial patellar fracture fragment (arrow) and the slightly disrupted medial retinaculum. The patella is subluxed
Lateral condylar fractures resulting from patellar dislocation are less well appreciated on plain films, but in some cases, one may see the fracture donor site (Fig. 10.13a). In other cases, the avulsed bony fragment, as opposed to the medial patellar fragment, can be very mobile and can be seen anywhere within the knee joint (Fig. 10.13b, c). On subsequent MR imaging, one usually can see the fracture site and the associated bone bruise of the lateral condyle (Fig. 10.13d, e).
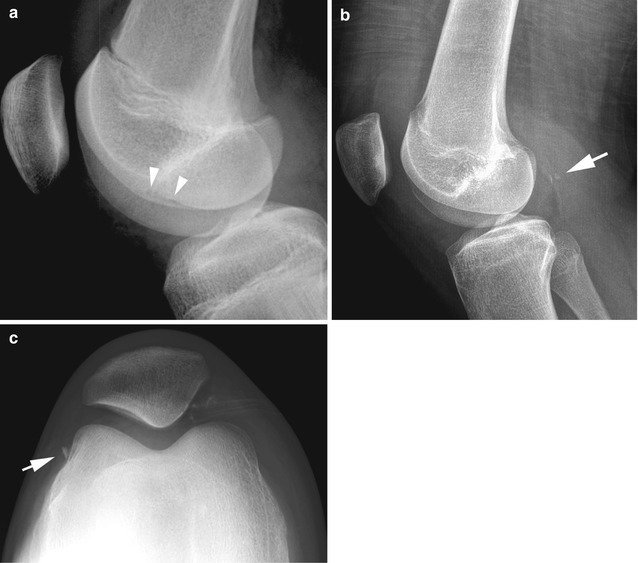
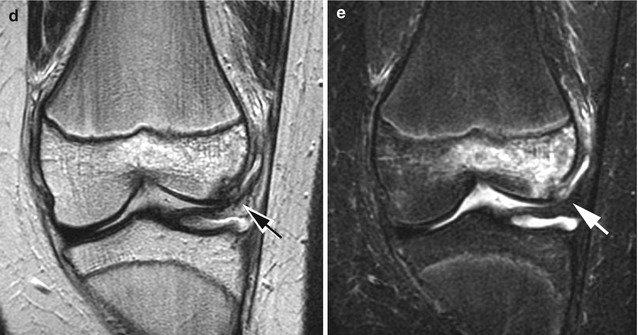
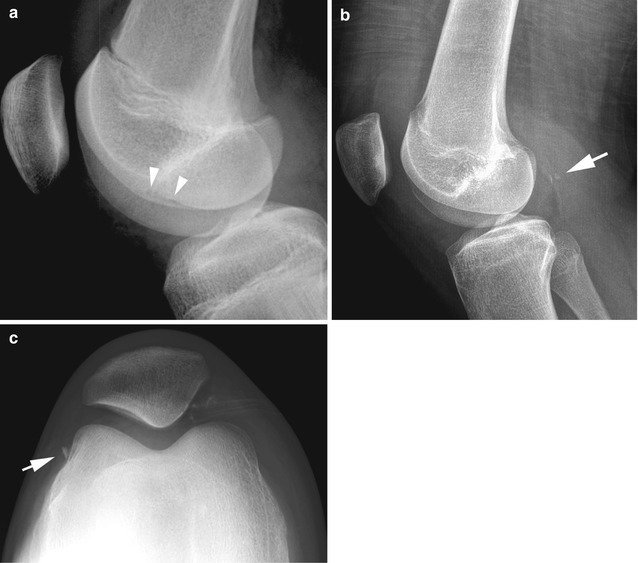
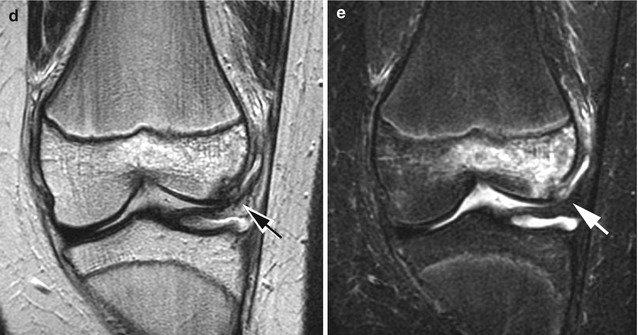
Fig. 10.13
Patellar dislocation with lateral condylar fracture. (a) Donor site. Note the subtle defect in surface of the lateral condyle (arrowheads) representing the donor site of a lateral condylar avulsion fracture. (b) Another patient demonstrates an avulsed fracture fragment in the popliteal bursa (arrow). (c) In this patient, the avulsed fracture fragment (arrow) is in the lateral joint recess. (d) Coronal T2 MR image demonstrates the avulsed lateral condylar fracture fragment (arrow). A bone bruise also is present in the lateral condyle. (e) Coronal STIR image demonstrates the avulsed fracture fragment (arrow) with surrounding edema along with a bone bruise in the lateral condyle
Patients with chronic recurrent patellar dislocation often have associated patella alta, a condition in which the patella is higher in position than normal. Abnormal tracking of the patella results, and the patellofemoral groove becomes shallow [13]. Patella alta is best seen on lateral view, but the shallow groove and associated flattening of the lateral condyle are best seen on skyline views (with 30 % flexion) of the patella. Most dislocations, whether acute or chronic, are lateral dislocations.
The role of MRI is not only to diagnose unsuspected transient patellar dislocations but also to evaluate for patellofemoral dysplasia, osteochondral fractures [14], and presence of osteochondral loose bodies. Patellar dislocations with loose bodies are usually treated surgically. Patients without loose bodies are treated non-operatively with bracing and rehabilitation.
Other avulsion fractures around the knee [15] included suprapatellar quadriceps tendon avulsions. These usually are fairly straightforward as the avulsed fracture fragment is clearly obvious. They are not nearly as common as the other two avulsion fractures/tendon injuries, that is, Sinding–Larsen–Johansson disease [16] and Osgood–Schlatter disease [17–19].
With Osgood–Schlatter disease, the infrapatellar tendon, as it inserts on to the tibial tubercle, can avulse part of the tubercle, or the tendon may simply undergo a tendon injury. Clinically, findings consist of pretubercular swelling and pain, and on imaging, swelling is present over the tibia tubercle. In addition the insertion of the infrapatellar tendon is edematous, and tendon itself appears swollen (Fig. 10.14a). In many cases but not all, an avulsed fracture fragment can be seen (Fig. 10.14b). With healing, one can see considerable hypertrophic bone formation (Fig. 10.15) and eventually a small acquired exocytosis. All of these configurations are virtually pathognomonic of Osgood–Schlatter disease but occasionally can be mimicked by the very rare periosteal chondroma of the tibial tubercle [20]. This lesion is more bulky, mostly lytic, and associated with destruction of the upper tibia under the tibial tubercle.