The classification of elbow instability has been a debated and ill-understood concept in the literature for numerous reasons. Although elbow instability has been documented for decades, the mechanism whereby instability occurs has only recently been described in detail. Clinical tests to establish the diagnosis of elbow instability have only recently been described. Finally, in the past, elbow instability was believed to be rare, although it is currently realized that this injury is not uncommon.
No simple classification for elbow instability exists, but rather a set of criteria are considered for diagnosis and treatment. These include: (a) the timing of the injury (acute, chronic, or recurrent); (b) the articulations involved; (c) the direction of displacement (valgus, varus, anterior, posterolateral rotatory); (d) the degree of displacement (subluxation or dislocation); and (e) the presence or absence of associated fractures.
The timing of the injury can be ascertained from the patient’s presenting history and can be corroborated by MRI findings. The elbow is a trochoginglymoid joint with two articulations within one capsule. Hence, injury can involve the hinge joint of the elbow (the radius and ulna articulating as a unit with the humerus) or the proximal radioulnar joint. The direction and degree of displacement can generally be inferred by the astute radiologist based on pattern of injury because the majority of patients with severe subluxation or dislocation of the elbow present for imaging with the articulation reduced.
Although elbow instability is clearly a complex entity that requires an integrated approach for complete characterization, the discussion of elbow instability in the literature has primarily focused on direction of displacement. This Chapter reviews the MRI anatomy of ligamentous stabilizers of the elbow, diagnostic imaging considerations for ligament injuries, and resultant directional instability patterns concentrating on those most commonly encountered in clinical practice, valgus and posterolateral rotatory instability as well as elbow dislocation.
Ulnar Collateral Ligament Complex Anatomy
Ligamentous structures of the elbow are comprised of focal condensations of the fibrous joint capsule, thus forming a capsuloligamentous complex similar to that encountered in the shoulder. The ulnar collateral ligament (UCL) originates from the inferior aspect of the medial epicondyle slightly posterior to the center axis of elbow rotation; thus, it is under greater tension with elbow flexion (1). The humeral origin of the UCL corresponds to approximately two-thirds of the width of the inferior aspect of the medial epicondyle and has no insertion on the adjacent medial condyle (2). The humeral origin of the UCL has a wider insertion than its ulnar counterpart. In a cadaveric study, Nakanishi et al. (3) showed that this was the result of the combined proximal attachment of both the anterior and posterior bundles.
In general, the collateral ligament complexes are best demonstrated on oblique coronal images. Axial and sagittal images are useful to confirm suspected pathology. As is the case elsewhere in the musculoskeletal system, ligaments are generally uniformly low in signal intensity on all pulse sequences except where magic angle effects or volume averaging may occur.
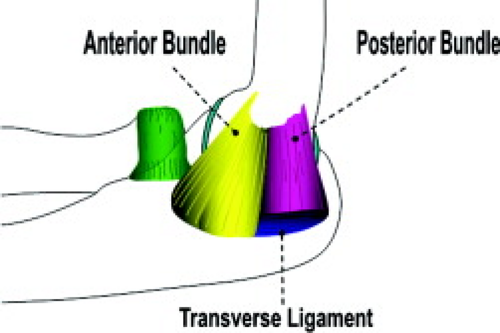
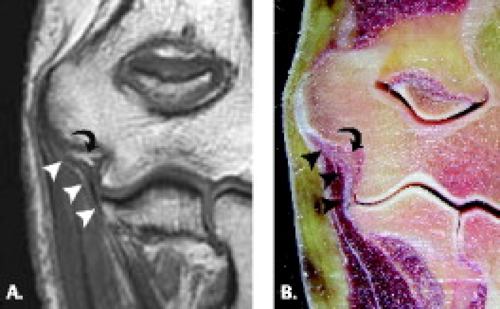
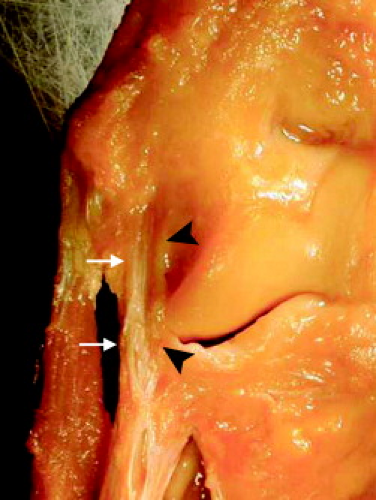
Three components of the UCL are classically described, the anterior, posterior, and transverse bundles (Fig. 10.1). The largest and most important component of the UCL is the anterior bundle, a discrete focal thickening of the medial capsule arising from the inferior margin of the medial epicondyle that inserts at the sublime tubercle of the proximal ulna (Fig. 10.2). Timmerman and Andrews (4) have demonstrated two histologic components of the anterior bundle, a deep layer between the two fibrous layers of the capsule and a superficial layer external to the medial capsule (Fig. 10.3). The superficial or extracapsular layer may in fact represent deep fibers of the ulnohumeral head of the flexor digitorum superficialis (5). Although the ulnar insertion of the anterior bundle is classically described as being flush with the articular margin of the medial coronoid, there may in fact be some variability of the ulnar insertion at the sublime tubercle. Timmerman and Andrews (6) have reported the ulnar insertion of the anterior bundle is in close proximity (1 mm) of the joint line. In contradistinction, Munshi et al. (5) found the anterior bundle may insert either at the articular margin or approximately 3 mm distally (Fig. 10.4). The more distal insertion may create a small recess on arthrograms simulating a partial undersurface tear of the anterior bundle. Therefore, differentiating partial undersurface tears of the UCL from a normal distal insertion of the anterior bundle may be clinically important.
On oblique coronal images, the anterior bundle of the UCL is seen as a uniformly low-signal structure. The proximal fibers of the anterior bundle may appear indistinct and lax (7). Typically the anterior bundle insertion at the sublime tubercle is flush with the articular margin. However, as previously mentioned, caution is warranted because variations in attachment may occur in this region.
The posterior bundle is a focal thickening of the medial capsule, which, unlike the anterior bundle, lacks
a distinct superficial component. The posterior bundle originates from the inferior aspect of the medial epicondyle and inserts at the posteromedial margin of the trochlear notch, forming the floor of the cubital tunnel (Fig. 10.5). On oblique coronal MR images, the humeral origin of the posterior bundle is seen posterior to a plane bisecting the epicondyles and extends to the posteromedial aspect of the olecranon. MRI identification of the posterior band is most facile in the axial plane when localizing the floor of the cubital tunnel at the joint line.
The transverse bundle, also termed the ligament of Cooper, extends between the ulnar insertions of the anterior and posterior bundles and plays little, if any, functional role. It is not readily visualized on routine MRI.
a distinct superficial component. The posterior bundle originates from the inferior aspect of the medial epicondyle and inserts at the posteromedial margin of the trochlear notch, forming the floor of the cubital tunnel (Fig. 10.5). On oblique coronal MR images, the humeral origin of the posterior bundle is seen posterior to a plane bisecting the epicondyles and extends to the posteromedial aspect of the olecranon. MRI identification of the posterior band is most facile in the axial plane when localizing the floor of the cubital tunnel at the joint line.
The transverse bundle, also termed the ligament of Cooper, extends between the ulnar insertions of the anterior and posterior bundles and plays little, if any, functional role. It is not readily visualized on routine MRI.
Variants of the UCL complex have been described and include a strong oblique pattern in which the transverse bundle flares in a fan-like configuration as it inserts on the anterior bundle and coronoid (8). In nearly one-fourth of specimens, Beckett et al. (8) identified a fourth component of the UCL termed the accessory or extra bundle. The accessory bundle originates from the posteromedial aspect of the capsule and inserts on the
transverse bundle. Importantly, there is little or no variation of the anterior or posterior bundles of the UCL.
transverse bundle. Importantly, there is little or no variation of the anterior or posterior bundles of the UCL.
Lesion Classification and MRI Characterization of the Ulnar Collateral Ligament
The visualized components of the UCL complex are seen as thin linear bands extending along the medial aspect of the elbow joint on MR images. For the purposes of MRI, the transverse ligament is not visualized nor is it considered a clinically important structure with regard to medial elbow stability. The MRI appearance of the UCL is characterized not only by its morphology, but also its signal intensity. The normal UCL has uniform low signal intensity attributable to its highly ordered structure and collagenous composition (9, 10). It has also been noted
that the normal UCL should also have fat signal intensity visible just beneath its fibers (Fig. 10.2). This finding represents the intra-articular fat that is seen in all normal elbow joints (3). The fat would be effaced in the setting of surrounding edema, joint effusion, or with contrast introduced into the articulation for arthrography.
that the normal UCL should also have fat signal intensity visible just beneath its fibers (Fig. 10.2). This finding represents the intra-articular fat that is seen in all normal elbow joints (3). The fat would be effaced in the setting of surrounding edema, joint effusion, or with contrast introduced into the articulation for arthrography.
MRI findings in the abnormal UCL vary with the severity of the injury. Diffuse increased signal intensity on T1- and T2-weighted images in the periligamentous soft tissues is consistent with the presence of edema and hemorrhage (11). One study also characterized high signal intensity within the periligamentous soft tissues as scar formation (3). With conventional MRI techniques, ligament sprains have been characterized by alterations in morphology, either thinning or thickening, as well as alterations in signal intensity. With regard to the latter, high signal intensity on T1- and or T2-weighted images within the substance of the ligament in the absence of discontinuity have been characterized in the literature as ligament sprain (9, 12–14). Although it has not been addressed in the literature, it is the belief and practice of the author that high T2-weighted signal within the substance of the ligament that parallels the signal intensity of joint fluid is more accurately described as a partial intrasubstance tear of the ligament fibers.
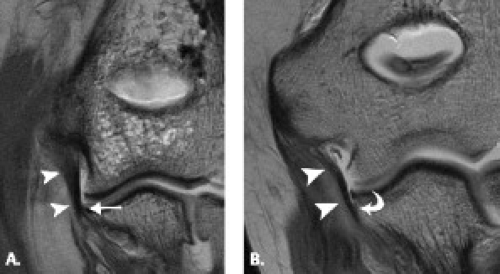
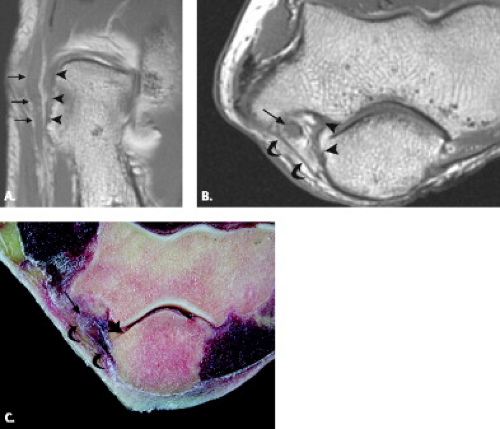
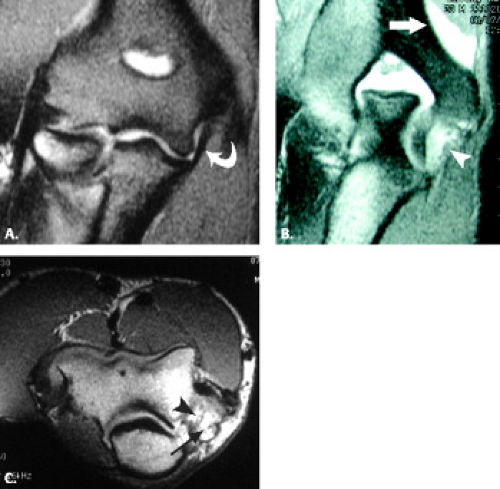
Partial tears of the UCL have been reported, but these reports have focused on pathology of the undersurface, or articular side of the ligament, primarily at either the humeral or ulnar attachments (6, 13). One of the earliest descriptions of this entity compared standard MRI and computed tomographic (CT) arthrography in a series of collegiate and professional baseball players who presented with persistent medial-sided elbow pain with throwing (6, 15). In this small series of patients (n = 7), CT arthrography showed abnormal leakage of contrast around the humerus, and more commonly the ulna, without gross extracapsular extravasation. CT arthrography correctly identified surgically proven lesions in six of seven patients, whereas standard MRI studies identi
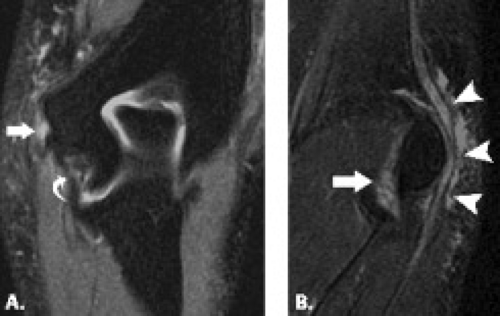
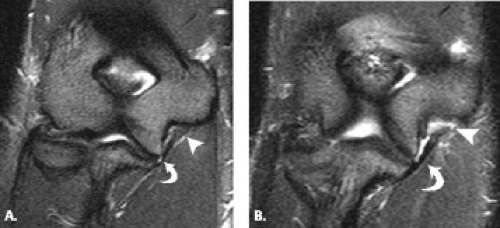
fied an abnormality in a single patient. The abnormal collection of contrast extending along the proximal aspect of the ulna, in contiguity with the normal contrast distribution along the ulnar articular surface and along the humeral condyle, were described as the T-sign (Figs. 10.6 and 10.7). Caution should be exercised when making the diagnosis of a partial detachment of the UCL from its attachment to the sublime tubercle, however, because variations in the distal attaching fibers have been described (Fig. 10.4) (5). Correlation with the clinical history, patient presentation, and physical examination findings should prevent falling prey to such a pitfall in imaging diagnosis. When pathologic, it is the belief of the author that this injury may represent a peelback phenomenon in which the ligament is stripped from its osseous attachment as described in anterior labral ligamentous periosteal sleeve avulsion in the glenohumeral joint (16). The role of MR arthrography in the detection of partial undersurface tears of the UCL was subsequently explored (17). The sensitivity, specificity, and accuracy for the detection of undersurface tears of the UCL by MR arthrography were 86%, 100%, and 86%, respectively (Figs. 10.8 and 10.9). Although scarcely addressed in the imaging literature, intrasubstance and superficial partial tears of the UCL should be considered in the imaging assessment of this structure. In applying the general principles for interpretation of signal intensity and morphology abnormalities in tendons and liga
ments, high T2 signal intensity within the substance of the ligament that rivals that of joint fluid would be consistent with an intrasubstance tear, and superficial surface irregularity and high T2 signal that parallels joint fluid would be consistent with a partial superficial ligament tear (Figs. 10.10 and 10.11). The latter should be suspected in cases of common flexor tendon abnormalities.
fied an abnormality in a single patient. The abnormal collection of contrast extending along the proximal aspect of the ulna, in contiguity with the normal contrast distribution along the ulnar articular surface and along the humeral condyle, were described as the T-sign (Figs. 10.6 and 10.7). Caution should be exercised when making the diagnosis of a partial detachment of the UCL from its attachment to the sublime tubercle, however, because variations in the distal attaching fibers have been described (Fig. 10.4) (5). Correlation with the clinical history, patient presentation, and physical examination findings should prevent falling prey to such a pitfall in imaging diagnosis. When pathologic, it is the belief of the author that this injury may represent a peelback phenomenon in which the ligament is stripped from its osseous attachment as described in anterior labral ligamentous periosteal sleeve avulsion in the glenohumeral joint (16). The role of MR arthrography in the detection of partial undersurface tears of the UCL was subsequently explored (17). The sensitivity, specificity, and accuracy for the detection of undersurface tears of the UCL by MR arthrography were 86%, 100%, and 86%, respectively (Figs. 10.8 and 10.9). Although scarcely addressed in the imaging literature, intrasubstance and superficial partial tears of the UCL should be considered in the imaging assessment of this structure. In applying the general principles for interpretation of signal intensity and morphology abnormalities in tendons and liga
ments, high T2 signal intensity within the substance of the ligament that rivals that of joint fluid would be consistent with an intrasubstance tear, and superficial surface irregularity and high T2 signal that parallels joint fluid would be consistent with a partial superficial ligament tear (Figs. 10.10 and 10.11). The latter should be suspected in cases of common flexor tendon abnormalities.
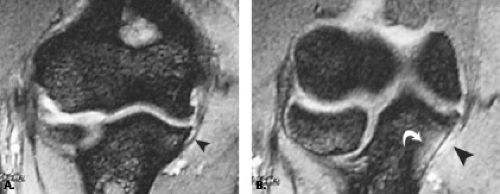
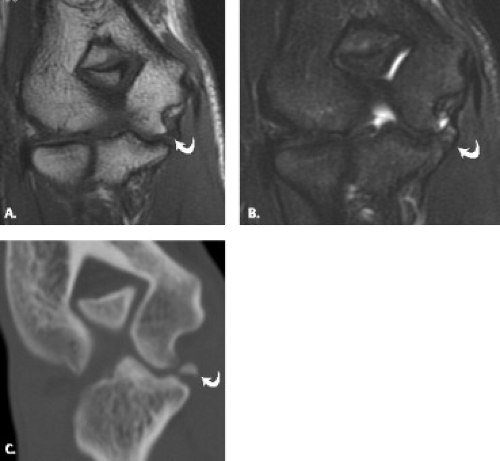
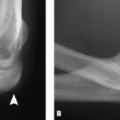
Full-thickness tears of the UCL are diagnosed by discontinuity along the course of the ligament (Figs. 10.12–10.14) (15, 18). A secondary sign that some authors have used to indicate the presence of full-thickness tear of the
UCL is an abnormal distribution of joint effusion along the course of the ligament with extravasation of fluid into the adjacent soft tissues (19). Whereas standard MRI has a suboptimal performance for detection of partial-thickness tears of the UCL, in the setting of full-thickness tear, most studies show a sensitivity, specificity, and accuracy that approaches 100% (9, 15, 18, 19). Similarly, MR arthrography has been shown to be sensitive, specific, and accurate in the characterization of the anatomy of the UCL in cadaveric studies as well as in the detection of full-thickness tears of this structure (3, 13, 17, 20–23). The imaging criteria for the diagnosis of UCL full-thickness tear are the same as described for standard MRI. The detection of discontinuity of the ligament and abnormal distribution of contrast material at the point of ligament insufficiency is noted.
UCL is an abnormal distribution of joint effusion along the course of the ligament with extravasation of fluid into the adjacent soft tissues (19). Whereas standard MRI has a suboptimal performance for detection of partial-thickness tears of the UCL, in the setting of full-thickness tear, most studies show a sensitivity, specificity, and accuracy that approaches 100% (9, 15, 18, 19). Similarly, MR arthrography has been shown to be sensitive, specific, and accurate in the characterization of the anatomy of the UCL in cadaveric studies as well as in the detection of full-thickness tears of this structure (3, 13, 17, 20–23). The imaging criteria for the diagnosis of UCL full-thickness tear are the same as described for standard MRI. The detection of discontinuity of the ligament and abnormal distribution of contrast material at the point of ligament insufficiency is noted.
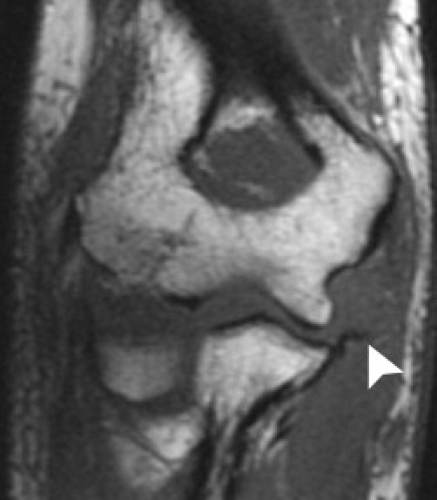 Figure 10.13 Ulnar collateral ligament rupture. T1-weighted coronal MR image shows a full-thickness rupture of the proximal attachment of the ulnar collateral ligament (arrowhead). |
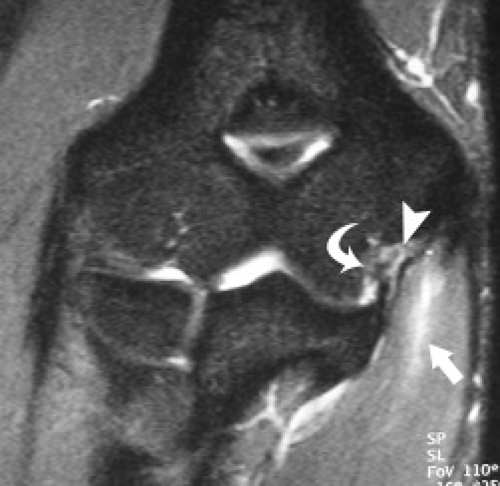
A description of injury to the UCL complex would be incomplete without localization of the imaging abnormality. In the setting of partial tears of the ligament, reported cases have discussed only the anterior band of the UCL complex (6, 13, 15, 17). Because the fibers of the anterior and posterior bands of the UCL are continuous and fan-like in nature, it can be difficult to localize pathology between these two components of the UCL complex (Figs. 10.15 and 10.16). It can be helpful to carefully assess the axial images in the region of the cubital tunnel, because this anatomic landmark isolates the posterior band. As previously noted, the undersurface as opposed to intrasubstance and superficial pathology predominates (Fig. 10.17). Finally, ulnar attachment, rather than humeral and midsubstance partial tears, is more frequently encountered (6, 13, 15, 17, 24). Full-thickness tears of the UCL occur most frequently in the midsubstance of the ligament (13, 25). Avulsion injuries with failure at the humeral and ulnar attachment have also been described (3, 24). In skeletally immature patients, failure at the humeral side with an avulsion fracture of the medial epicondylar ossification center occurs most frequently (Fig. 10.18). In adults, if avulsion-type injuries occur, they do so at the ulnar attachment to the sublime tubercle (Fig. 10.19). This injury may or may not have a detectable osseous component on radiographs. MRI has been shown to be useful in treatment planning with regard to direct repair or reconstruction in the setting of avulsive injury (25).
Valgus Instability
History and Mechanism of Injury
When valgus forces generated at the flexed elbow exceed the load-to-failure strength of the UCL, damage to the ligament occurs and valgus instability can develop (26–30). Such instability can occur from a single traumatic event or, more commonly, chronically as a result of repetitive microtrauma as seen in repetitive overhead throwers. The diagnosis of valgus instability is based on the history, findings on physical examination, instability on dynamic radiography under valgus load, arthrography, and MRI (31).
Throwing athletes who sustain an acute injury to the UCL state they heard or felt a “pop” from the elbow. The rapid onset of pain and swelling will subsequently preclude the ability to continue throwing. The athlete with an acute on chronic injury can recall a specific episode of injury but will admit to having had prodromal episodes of intermittent elbow pain that were often related to repetitive, prolonged throwing. The athlete with chronic UCL instability reports vague medial elbow pain related to throwing activity but is capable of continuing to throw. Frequently, the athlete will elicit a history of a loss of velocity on a pitch or a lack of pitch control (26, 27, 31, 32).
Although the specific techniques of throwing vary slightly among different sports, the same basic throwing mechanism is common to all (33, 34). The baseball pitch is representative and exemplifies the five phases of throwing: windup, early cocking, late cocking, acceleration, and followthrough (Fig. 10.20). Windup starts when the thrower begins the movement and is completed when the front of the knee reaches its maximum height. The elbow is flexed throughout this phase. The arm-cocking phase starts when the front foot contacts the mound and ends when the arm reaches maximum external rotation. Shortly after the arm-cocking phase begins, the upper torso is rotated to face the batter (30). Elbow flexors are active during the early part of the arm-cocking phase (30, 35). Just before maximum external rotation, the triceps become active and elbow flexors become inactive, resulting in a decrease in flexion torque, and thus the elbow begins to extend. At the conclusion of the arm-cocking phase, the shoulder is abducted, extended, and externally rotated to approximately 130 degrees and the elbow flexed to approximately 90 degrees. In this position, the elbow begins to be subjected to severe valgus stress (30). During the arm-cocking phase, the arm rotates externally at the shoulder and varus torque is produced at the elbow to prevent the joint from going into valgus. In the transitional moment from arm cocking to arm acceleration, the shoulder rotates internally, the forearm is in near full supination, and the elbow flexes another 20 to 30 degrees increasing the valgus load on the medial side of the elbow. This moment is called the explosion or initiation of speed (30). The arm acceleration phase is the short time from maximum external rotation to ball release. During this phase, the elbow extends rapidly to 20 degrees of flexion at ball release with a maximum speed as high as 4500 degrees per second (30, 36). During arm acceleration, the need to resist valgus stress at the elbow can result in wedging of the olecranon against the medial aspect of the trochlear groove and the olecranon fossa. The arm deceleration phase begins from ball release and when the arm reaches its maximum internal rotation. Soon after ball release, high compressive forces are generated at the shoulder and the elbow to prevent distraction. During the later stages of acceleration, the triceps muscle contracts to
extend the elbow, placing tensile forces on the olecranon process. The followthrough phase begins at maximal internal rotation and ends when the pitcher attains a balanced fielding position.
extend the elbow, placing tensile forces on the olecranon process. The followthrough phase begins at maximal internal rotation and ends when the pitcher attains a balanced fielding position.
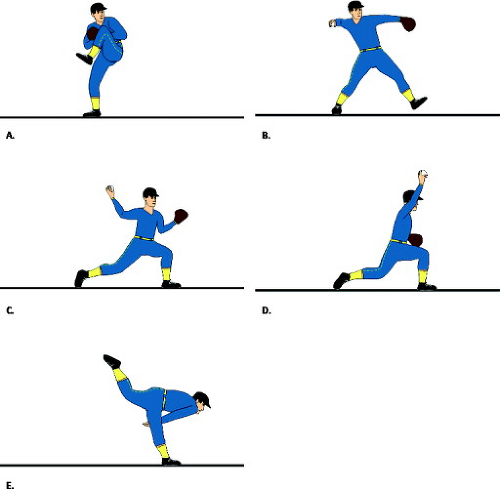 Figure 10.20 Phases of throwing. The baseball pitch exemplifies the five phases of throwing: (A) windup; (B) early cocking; (C) late cocking; (D) acceleration; and (E) followthrough. |
This description of the position changes that occur during the throwing motion expose the elbow to severe stress at several points in the action, each of which can result in serious injury. The large forces generated during the acceleration phase must be absorbed by the supporting structures on the medial side of the elbow, primarily the anterior band of the UCL complex. If the forces generated exceed the tensile strength of the ligament, microtears will occur. At the same time, considerable compression force is placed on the lateral side of the elbow; this force is primarily absorbed by the articular surface of the radiocapitellar joint (34).
Clinical Diagnosis
Tenderness with palpation of the UCL, particularly in chronic instability, is not uniformly present and should not be the determining factor in making the diagnosis of ligament insufficiency (26, 37). Provocative testing for
UCL instability is a reliable method of determining injury. The most common test is the manual valgus stress test, which stresses the anterior band of the UCL complex. This maneuver is performed with the patient in the seated or supine position with the elbow in approximately 30 degrees of flexion. The patient’s pronated forearm is secured between the examiner’s forearm and trunk. The examiner’s opposite hand stabilizes the distal humerus and provides a lateral post while controlling against external rotation. A valgus moment is then applied across the patient’s elbow. Bilateral comparison provides a baseline for physiological laxity. A positive test result is present if unilateral medial joint space widening is detected or if the maneuver reproduces the athlete’s symptoms of medial elbow pain (26, 30



UCL instability is a reliable method of determining injury. The most common test is the manual valgus stress test, which stresses the anterior band of the UCL complex. This maneuver is performed with the patient in the seated or supine position with the elbow in approximately 30 degrees of flexion. The patient’s pronated forearm is secured between the examiner’s forearm and trunk. The examiner’s opposite hand stabilizes the distal humerus and provides a lateral post while controlling against external rotation. A valgus moment is then applied across the patient’s elbow. Bilateral comparison provides a baseline for physiological laxity. A positive test result is present if unilateral medial joint space widening is detected or if the maneuver reproduces the athlete’s symptoms of medial elbow pain (26, 30
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree