Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
5.1 Embryology []
5.2 Anatomy [, ]
5.2.1 Description
5.3 Histology []
5.3.1 The Ovary in Adulthood
5.3.2 The Ovary in Menopause
5.2 Anatomy [2, 3]
5.2.1 Description
The ovary lies in the peritoneal cavity behind the broad ligament linked to the junction of the mesometrium and the mesosalpinx by a thin double leaf of peritoneum the mesovarium (Fig. 5.1).
Fig. 5.1
(a) Posterior view of the left adnexa (The infundibulo pelvic ligament is drawn downward). 1 uterus, 2 tube: Intramural segment (1 cm in length), 3 tube: 3′ Isthmic segment (2 cm in length) and 3″ ampullary portion (6 cm in length), 4 Fimbriae, 5 Fimbria ovarica (Ovarian Fimbria), 6 Ovary, 7 Infundibulopelvic ligament (attachment), 8 Ovarian ligament, 9 Broad ligament: Mesometrium, 10 Broad ligament: External part, 11 Broad ligament: Mesosalpinx. (b) Lateral view of the left adnexa. 1 Broad ligament: Mesometrium, 2 Broad ligament: Mesosalpinx, 3 Tube, 4 Broad ligament: Mesovarium containing blood vessels to the ovarian hilum, 5 Ovary: Stroma, 6 Ovary: Surface Epithelium, 7 Ovary: Hilus (From Testut [3])
During reproductive age, the normal ovary is oval in shape, measures about 3 cm length, and has a cross-sectional surface <6 cm2 and a volume <8 cm3. Its surface is smooth in young women.
After menopause, size decreases gradually and becomes more flattened usually with a slightly nodular surface.
The ovary has two lateral and medial faces, superior and inferior poles, and anterior and posterior borders.
The lateral face contacts a depression of the parietal peritoneum, the ovarian fossa. On the extraperitoneal side, this fossa is limited in front by the posterior border of the external iliac vein and at the back by the uterine artery and the companion pelvic ureter (Fig. 5.2).
Fig. 5.2
1 uterus, 2 tube, 3 ovary, 4 ovarian fossa, 5 ureter, 6 ovarian artery, 7 internal iliac artery, 8 uterine artery, 9 obturator artery, 10 obturator nerve, 11 external iliac artery, 12 parietal peritoneum, 13 douglas, 14 rectum, 15 parietal peritoneum, 16 aorta, 17 inferior vena cava
The medial face is in relationship with the infundibulum of the tube.
The superior pole is in relation with the fimbriae.
The inferior pole points downward toward the pelvic floor.
The anterior border faces the mesovarium.
The posterior border is free.
5.2.2 Peritoneal Attachments (Fig. 5.1)
1.
Infundibulopelvic ligament: It is a peritoneal fold that is attached to the upper part of the lateral surface of the ovary. It contains the ovarian vessels and nerves. It passes superiorly over the external iliac vessels and genitofemoral nerve and passes between the posterior parietal peritoneum and the lumbar portion of the ureter. On the right side, the ligament is attached to a fold of peritoneum posterior and inferior to the caecum and the appendix. On the left side, the ligament is higher than on the right and is lateral to the junction of the descending and sigmoid colon.
2.
Ovarian Ligament
Embryology: Definition of the gubernaculum: As the mesonephros degenerates, a ligament the gubernaculum develops on each side of the abdomen from the caudal pole of the gonad. The gubernaculum passes obliquely through the developing anterior abdominal wall at the site of the future inguinal canal and attaches caudally to the internal surface of labioscrotal swellings. It will give rise to the ovarian ligament and to the round ligament of the uterus.
Anatomy: The ovarian ligament attaches the inferomedial extremity of the ovary to the lateral angle of the uterus posteroinferior to the uterine tube. It lies in the posterior leaf of the broad ligament.
The ovarian ligament is continuous with the medial border of the round ligament.
3.
Mesovarium
The mesovarium attaches the anterior border of the ovary to the back of the broad ligament. It carries blood vessels and nerves to the ovarian hilum.
The uterine tube arches over the ovary and ascends in front of the anterior border of the ovary, then curves over its tubal end and passes down on its medial surface.
5.2.3 Vascular Supply and Lymphatic Drainage
5.2.3.1 Arteries (Fig. 5.3)
Fig. 5.3
1 uterine artery, 2 ureter, 3 artery of the fundus, 4 medial tubal artery, 5 middle tubal artery, 6 lateral tubal artery, 7 ovarian artery and suspensory ligament of the ovary, 8 artery of the round ligament, 9 anastomose between the uterine artery and its terminal portion
1.
The Ovarian Artery
It descends behind the peritoneum crosses in front the lumbar ureter, crosses in front and medially the external iliac pedicle, and passes behind the external iliac vein. Here the artery turns medially in the ovarian suspensory ligament, continues in the mesosalpinx, and passes back in the mesovarium.
2.
The tuboovarian branch of the uterine artery originates at the end of the uterine artery (close to the origin of the tube) where the artery bifurcates in the artery of the fundus of the uterus and the tuboovarian artery. This artery lies in the mesosalpinx and anastomoses with the ovarian artery (sometimes forming a plexus) before entering the mesovarium or enters separately into the mesovarium.
5.2.3.2 Veins
The ovarian veins emerge from the ovary as a plexus in the mesovarium and the suspensory ligament. Two veins issue from the plexus which merge further in a single vein. The right one enters the VCI and the left one the left renal vein.
5.2.3.3 Lymphatic Drainage
Lymphatic drainage is via three main routes:
Lomboaortic following the ovarian artery to pre- and lateral aortic nodes below the origin of the renal arteries
Iliac nodes situated behind the external iliac artery, in front of the uterine artery
More rarely, inguinal nodes
5.3 Histology [4]
5.3.1 The Ovary in Adulthood
5.3.1.1 Surface Epithelium (Figs. 5.4 and 5.5)
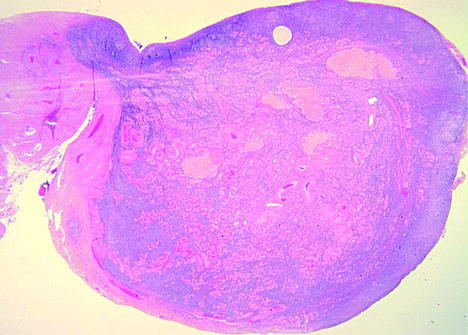
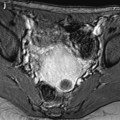
Fig. 5.4
Low magnified showing view the entire ovary. Cortical stroma that appears with a purple color is much more dense in the cortex than in the medulla. The outer cortex contains an antral follicle (at the top). On the left lies the hilum of the ovary
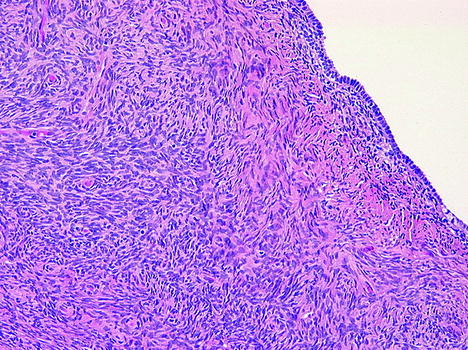
Fig. 5.5
Histology of the epithelium and adjacent stroma. Surface epithelium has a single layer of cuboidal or cylindric cells and in some areas has a double layer. Stroma is made of fusiform cells with a storiform pattern. In the outer cortex, there is an area of fibrosis (pink portion contrasting with purple adjacent stroma), which is quite common with increasing age
It consists of a simple layer of modified mesothelial cells. The cells vary from flat to cuboidal to columnar, and several types may be seen in different areas in the same ovary. The surface cells are separated from the underlying stroma by a distinct basement membrane.
Epithelial inclusion glands and their cystic counterparts arise from cortical invaginations of the surface epithelium and have lost their connection with the surface. They measure usually from 2 to 5 mm. An epithelium-lined cyst greater than 1 cm is designated a cystadenoma.
Histochemical studies have demonstrated glycogen, as well as acid and neutral mucopolysaccharides within surface epithelial cells. Unlike extraovarian mesothelial cells, surface epithelial cells have 17-beta-hydroxysteroid-deshydrogenase activity.
Surface epithelial cells are immunoreactive:
For cytokeratin, Ber-EP, desmoplakin, vimentin, and TGF-alpha
For receptors of estrogen, progesterone, and epidermal growth factor
Several antigens associated with ovarian tumors of surface epithelial origin have been demonstrated including CA 125, CA19-9, and MH99.
5.3.1.2 Stroma (Figs. 5.4 and 5.5)
The stroma starts beneath the basal membrane and occupies the majority of the ovary, surrounding follicles and their derivates (corpus luteum and corpus albicans). The boundary between cortical and medullar stroma is arbitrary.
The stroma is composed of spindle-shaped cells and a network of reticulin and collagen fibers. Other types of cells may be present.
Spindle-Shaped Cells
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree