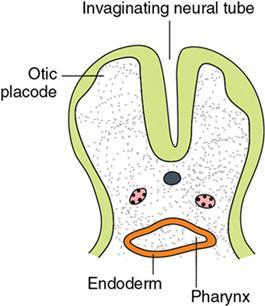
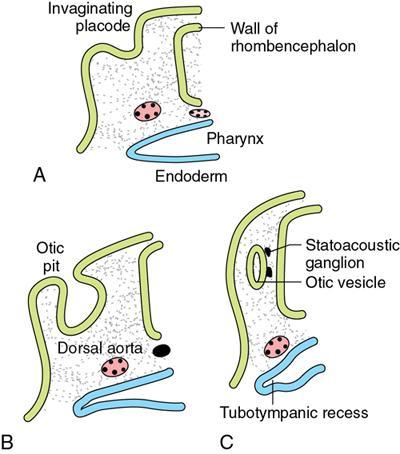
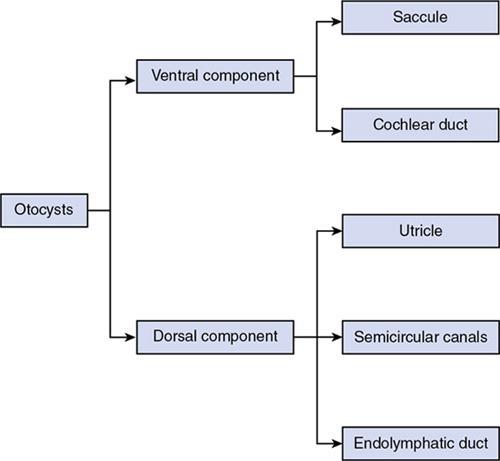
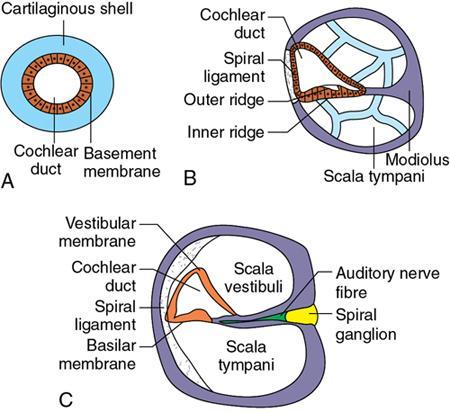
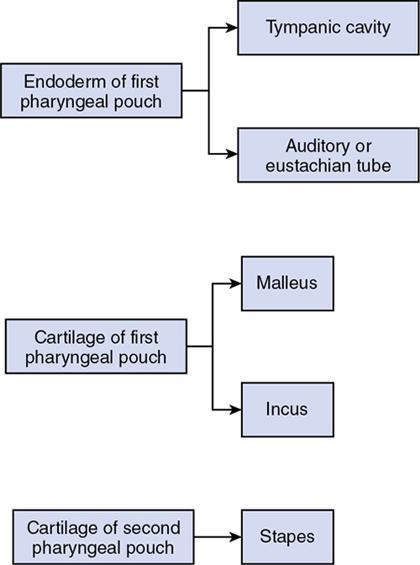
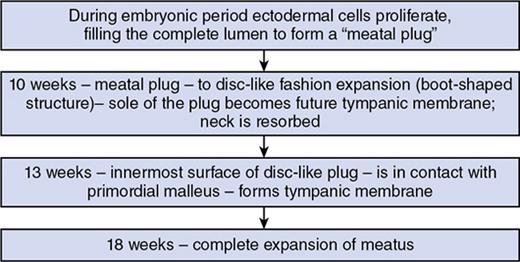
B.M. Ashwini, Padma Challa Ramprakash, A. Amritha The embryology of the human body is very vast including several intricate details and multiple sequential steps. Its thorough knowledge helps us to understand the pathophysiology and radiological imaging appearance of several variants and anomalies. So in this chapter, we will briefly go through the embryology of head and neck and its radiological importance. This is discussed under Paediatric Neck Chapter 3.7. First indication – at 22 days – thickening of surface ectoderm on each side of rhombencephalon – forms otic placodes (Fig. 3.6.1). Otic placodes invaginates – otic or auditory vesicles or otocysts formed. (Fig. 3.6.2A and B). The otocysts further give rise to the ventral and dorsal components. During formation of otic vesicle, a small group of cells split away and form the statoacoustic ganglion – which supply sensory cells of organ of corti, saccule, utricle and semicircular canals (Fig. 3.6.2C). Derivatives of ventral and dorsal components together constitute the membranous labyrinth. (Flowchart 3.6.1) shows the division of otocysts and their respective derivatives. Sixth week – saccule forms a tubular outpouching at its lower pole called cochlear duct – which in turn penetrates the surrounding mesenchyme in a spiral fashion and towards the end of eighth week – it completes 21⁄2 turns. Ductus reuniens – remains as a connection between saccule and cochlear duct. At seventh week – cells of cochlear duct differentiate into the spiral organ of corti – which serves to convert sound impulses to electric impulses. The mesenchyme surrounding the cochlear duct – differentiates into cartilage – which around 10th week – forms two perilymphatic spaces namely (Fig. 3.6.3A and B), Cochlear duct is separated from scala vestibuli by vestibular membrane (Fig. 3.6.3B and C). Cochlear duct is separated from scala tympani by basilar membrane (Fig. 3.6.3A–C). Lateral wall of the cochlear duct is attached to the surrounding cartilage by a spiral ligament and its median wall is connected to and supported by modiolus (future axis of bony cochlea). Epithelial cells of cochlear duct form two ridges namely the inner and outer ridge. During the sixth week the flattened outpouchings of the utricular part of the otic vesicle form the semicircular canals. One end of each canal dilates to form the crus ampullare; the other end, which does not dilate, forms the crus nonampullare. Cells in ampulla – form crista ampullaris, a crest – which contain sensory cells responsible for impulses generated by equilibrium. Similar sensory areas, called maculae acusticae, develop in walls of utricle and saccule. Impulses generated by change in position are then sent to the vestibular fibres of cranial nerve VIII. The distal part of the endoderm of first pharyngeal pouch expands in a lateral direction – forms a tubotympanic recess – which in turn widens – forms tympanic cavity. Proximal part of endoderm of the first pharyngeal pouch – narrows – forms auditory or Eustachian tube. Ossicles remain embedded in the mesenchyme till the eighth month. When the ossicles are free of surrounding mesenchyme – endodermal epithelium connects them in a mesentery-like fashion to the wall of the cavity. Tensor tympani, which is the muscle of malleus – is innervated by mandibular division of trigeminal nerve. Stapedius muscle, which is the muscle of stapes – is innervated by facial nerve (nerve to the second pharyngeal arch). During late fetal life – tympanic cavity expands dorsally by the vacuolization of surrounding tissues – forms tympanic antrum. After birth – epithelium of tympanic cavity – invades the bone of the developing mastoid process – forming epithelium-lined air sacs – pneumatization. (Flowchart 3.6.2) representing the origins of various parts of the middle ear. RADIOLOGICAL VIGNETTE Most important is to assess size and shape of middle ear cavity. If the middle ear cavity is air-containing, assessment of its size and shape are easy to make. But in congenital anomalies, middle ear contains undifferentiated embryological mesenchyme (thick glue-like substance), which cannot be radiologically differentiated from soft tissue, retained mucus or serous otitis media. It is derived from six auricular hillocks – three on each pharyngeal arch 1 and 2. Originally formed in the neck, it later migrates in cranial direction during development of mandible. (Table 3.6.1) shows the derivatives of the auricular hillocks. It develops as invagination of first pharyngeal arch tissue. (Flowchart 3.6.3) represents the development of the external auditory meatus. (Table 3.6.2) depicts a tabular column of the various degrees and components of the external auditory canal deformity. RADIOLOGICAL IMPORTANCE Estimate thickness of atretic plate from coronal section imaging. Determine position of abnormal auditory meatus in relation to surrounding structures such as the middle ear and the TMJ. It is important from surgical perspective – if pinna is low lying in relation to middle ear cavity – approach for surgery may change.
3.6: Embryology of head and neck
Overview
Branchial apparatus embryology
Embryology of ear (please also refer to temporal bone chapter for further reading): Internal ear
Saccule, cochlea and organ of corti
Utricle and semicircular canals
Middle ear
Tympanic cavity and auditory tube
Ossicles
External ear
Hillock
Auricle Component
1
Tragus
2
Helix
3
Cymba concha
4
Concha
5
Antihelix
6
Antitragus
External auditory meatus:
Slight (small EAC)
Moderate (absent EAC)
Severe (absent EAC)
Hypoplastic tympanic membrane
Small middle ear cavity
Hypoplastic middle ear cavity
Hypoplastic tympanic bone
Atretic plate
Severe ossicular deformity
Small middle ear cavity
Deformed malleus and incus
Poor mastoid aeration
Varying ossicular deformity
Well-aerated mastoid
Well-aerated mastoid
Thyroid gland
Radiological importance
Salivary glands
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Embryology of head and neck






