Fig. 2.1
Imaging appearance of gallstones on plain radiograph and ultrasound. (a) Plain radiograph demonstrates laminated radiopaque gallstones in the right upper quadrant. Up to a fifth of the gallstones can be seen on plain radiograph of the abdomen. (b and c) Noncontrast CT of the gallbladder shows gallstones with Mercedes-Benz sign (arrows). Mercedes-Benz sign is due to nitrogen collection in triradiate configuration, within fissures of a gallstone. (d) Ultrasound shows multiple echogenic gallstones with distal acoustic shadowing, within the gallbladder lumen. (e) Ultrasound shows wall echo shadow sign in a patient with multiple gallstones and chronic cholecystitis. The outer echogenic line (straight arrow) represents the gallbladder wall, while the inner echogenic line (curved arrow) represents the outer edge of gallstones
Typically, gallstones are seen as echogenic foci with clean distal acoustic shadowing (Fig. 2.1d). Wall echo shadow sign refers to the parallel echogenic lines produced by a combination of the gallbladder wall, echogenic stone, and associated distal acoustic shadowing (Fig. 2.1e). The hypoechoic line seen between the two echogenic lines represents interposed bile. This sign is seen in gallbladder filled with either a single large gallstone or multiple small gallstones. Ultrasound has higher sensitivity than CT in diagnosing gallstones and is therefore the screening modality of choice. Although ultrasound remains the exam of choice for suspected cholecystitis, there are ever more cases of acute cholecystitis being detected today with CT in the evaluation of abdominal pain than in the past.
Majority of the patients with gallstones are asymptomatic. Sometimes the gallstone can cause transient gallbladder outflow obstruction, leading to biliary colic. Biliary colic patients present with transient pain for 1–3 h with nausea and vomiting. The symptoms subside when the gallstone falls back into the gallbladder or passes distally into the biliary tree.
Acute Cholecystitis
Acute cholecystitis usually is caused by the gallstone obstruction of the cystic duct or the gallbladder neck (one-third of cases). Acute cholecystitis without stones (5–10 % of cases) can be seen in patients with adenomyomatosis, gallbladder polyp, and malignant neoplasm [1, 2]. The predisposing factors for acute acalculous cholecystitis include history of trauma, mechanical ventilation, hyperalimentation, postoperative/postpartum state, diabetes mellitus, vascular insufficiency, prolonged fasting, and burns [2].
The clinical presentation includes right upper quadrant pain for more than 6 h (vs. biliary colic), nausea, vomiting, and fever in a patient with history of gallstones. No clinical or lab finding provides high enough positive predictive value in making the diagnosis of acute cholecystitis.
Imaging
Ultrasound is the first-line imaging modality in diagnosing acute cholecystitis because of wide availability, ability to detect gallstones as well as biliary ducts, and accuracy in diagnosing acute cholecystitis. The ultrasound findings of acute cholecystitis include gallbladder wall thickening (>3 mm), gallbladder distension (>5 cm transverse dimension), and positive Murphy’s sign (Fig. 2.2) [1, 3]. Sonographic Murphy’s sign by itself does not have a high positive predictive value and can be falsely negative in patients who have received analgesic medication. Another imaging finding of acute cholecystitis is the presence of a pericholecystic fluid collection, sometimes extending to the perihepatic space [2, 4].
Fig. 2.2
Ultrasound imaging of acute cholecystitis. (a) Ultrasound in a patient with acute cholecystitis demonstrates multiple gallstones and striated thickening of the gallbladder wall (arrow). (b and c) Ultrasound in a patient with gangrenous cholecystitis demonstrates striated thickening of the gallbladder wall, intraluminal sludge, and sloughed mucosa (arrowhead). Focal thinning of the necrotic gallbladder is indicated by the straight arrow and appears to represent the donor site for the sloughed-off mucosa. (d) Ultrasound in a patient with acute cholecystitis shows gallbladder wall thickening (arrowheads) and complex fluid, which represented pus during cholecystostomy tube placement
Gallbladder wall thickening is a finding of acute cholecystitis which can also be seen in other conditions such as hypoproteinemia, ascites, pancreatitis, right heart failure, renal failure, liver failure, and hepatitis. Striated gallbladder wall thickening is no more specific for acute cholecystitis than the observation of gallbladder wall thickening from other causes. In the clinical setting of acute cholecystitis, the presence of striated gallbladder wall thickening suggests gangrenous cholecystitis.
Cholescintigraphy (HIDA scan) is considered second-line imaging modality which can be used after equivocal ultrasound study. Cholescintigraphy has a sensitivity and specificity which is superior to ultrasound. Although it may take more than 2 h to complete the study, the use of morphine (0.04 mg/kg) allows cholescintigraphy to be completed in 1.5 h. The classic findings on cholescintigraphy include nonvisualization of the gallbladder 30 min after morphine injection and presence of a curvilinear area of increased radiotracer activity (rim sign) in the liver adjacent to the gallbladder (Fig. 2.3). Rim sign is most commonly seen in patients with gangrenous cholecystitis and is due to extension of inflammation beyond the gallbladder.
Fig. 2.3
Gangrenous cholecystitis on cholescintigraphy. Cholescintigraphy study (HIDA scan) demonstrates nonvisualization of the gallbladder and a curvilinear area of increased radiotracer activity (rim sign) in the pericholecystitic liver parenchyma (arrowheads)
If ultrasound and/or cholescintigraphy show no evidence of acute cholecystitis or any other cause for the right upper quadrant pain, a contrast-enhanced CT is considered the next most appropriate imaging modality. The CT findings include gallstones, gallbladder wall thickening, gallbladder wall enhancement, increased bile attenuation (possibly indicative to empyema), distended gallbladder, and pericholecystic fluid collection (Table 2.1; Fig. 2.4) [5]. CT has lower sensitivity than US in detecting gallstones and can miss noncalcified gallstones.
Table 2.1
CT findings of acute cholecystitis
Thickening of the gallbladder wall (normal wall thickness is up to 3–4 mm) |
Gallstones |
Gallbladder distention (>5 cm in transverse dimension) |
Pericholecystic fluid |
Indistinct interface between the gallbladder wall and the liver |
Pericholecystic inflammatory changes |
Transient focal attenuation difference |
Increased density bile |
Fig. 2.4
CT findings of acute cholecystitis. (a) Contrast-enhanced CT shows distended gallbladder with wall thickening (arrows) and pericholecystic inflammatory changes. (b) Contrast-enhanced CT shows small calculus (arrowhead) causing cystic duct obstruction
MR imaging is not a frontline imaging modality for acute cholecystitis and can be used after equivocal US study. The advantage of MR over CT is its ability to reliably study common bile duct and the lack of ionizing radiation which is especially important in pregnant population. Although, gadolinium is useful in making the diagnosis of acute cholecystitis, it should not be used in pregnant population. The important findings of cholecystitis on MR imaging are described in Table 2.2 (Fig. 2.5).
Table 2.2
MR findings of acute cholecystitis
Gallbladder empyema | Low-signal intensity on T2 and high-signal intensity on T1 WI |
Gallstones | Signal void on MRCP and low signal on T1–T2 WI |
Gallbladder wall thickening | Enhancing wall and high signal on T1 and low to high on T2 WI |
Gas within the gallbladder wall | Signal void in the wall |
Pericholecystic inflammation | High intensity on T1 and T2 WI |
Hemorrhage | High intensity on T1 and T2 WI |
Fluid collection | High intensity on T1 and T2 WI |
Fig. 2.5
MR findings of acute cholecystitis. (a and b) HASTE sequence shows gallbladder wall thickening (arrowheads), increased signal intensity (curved arrows), and multiple small gallstones. HASTE is a high-speed, heavily T2–weighted sequence with partial Fourier technique which has high sensitivity for fluid and a fast acquisition time (<1 s/slice)
The complications of acute cholecystitis include gallbladder empyema, gangrenous cholecystitis, emphysematous cholecystitis, gallbladder perforation, Mirizzi syndrome, and gallstone ileus.
Mirizzi Syndrome
The obstruction of the common bile duct or common hepatic duct by calculus impacted in the Hartmann’s pouch or cystic duct constitutes Mirizzi syndrome (Fig. 2.6). Mirizzi syndrome or choledocholithiases should be suspected whenever there is elevated bilirubin level along with clinical symptoms of acute cholecystitis.
Fig. 2.6
Mirizzi syndrome. (a) ERCP demonstrates narrowing of the proximal CBD (arrowhead) due to extrinsic impression produced by calculus in the gallbladder neck. (b) Contrast-enhanced CT shows the calculus (curved arrow) in the gallbladder neck with secondary inflammation causing intrahepatic biliary ductal dilatation (arrows)
Empyema
It is also called suppurative cholecystitis and occurs typically in diabetic patients, when the bile becomes infected and pus fills the distended gallbladder [1]. On imaging, gallbladder empyema is manifested as gallbladder distension, wall thickening, pericholecystic fluid accumulation, intraluminal sludge/pus, and intraluminal air (Fig. 2.7).
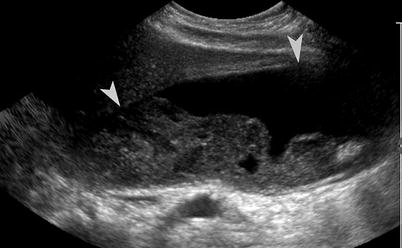
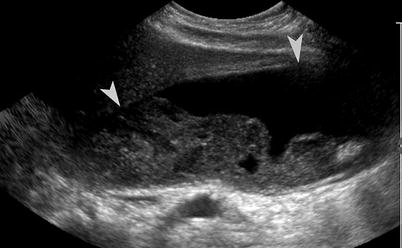
Fig. 2.7
Gallbladder empyema. Ultrasound shows marked distention (arrowheads) of the gallbladder lumen and intraluminal debris in a patient with gallbladder empyema
Gangrenous Cholecystitis
It is an advanced form of acute cholecystitis, most frequently seen in elderly men. It is characterized by increased intraluminal pressure, gallbladder distension, gallbladder wall necrosis, intramural hemorrhage, and abscess formation (Fig. 2.8) [1, 2]. There is an increased association of gangrenous cholecystitis with cardiovascular disease and leukocytosis of more than 17,000 WBC/mL. Although CT is highly specific (>90 %) in identifying patients with acute gangrenous cholecystitis, it is not very sensitive (Table 2.3).
Fig. 2.8
Gangrenous cholecystitis. (a and b) Contrast-enhanced CT scan in two patients with gangrenous cholecystitis shows irregularity (arrows) of the gallbladder wall, gallbladder wall thickening, and pericholecystic inflammation
Table 2.3
CT findings of gangrenous cholecystitis
Gas in the gallbladder wall or lumen |
Intraluminal membranes |
Irregularity of wall |
Pericholecystic abscess
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|