Fig. 20.1
Clavicle fracture. AP view of the clavicle shows a comminuted fracture at the distal third of the clavicle (arrowhead)
Complications
Clavicle fracture can be associated with injury to the subclavian artery, subclavian vein, or brachial plexus. There may be associated sternoclavicular or acromioclavicular subluxation, as well as pneumothorax. Malunion and nonunion can lead to shortening of the shoulder girdle and chronic pain [3].
Sternoclavicular Dislocation
Sternoclavicular dislocation accounts for only 2–3 % of shoulder girdle dislocations and can occur after indirect blunt trauma to the shoulder [4]. The dislocation allows for free rotation of the head of the clavicle with the intact costoclavicular ligament serving as a fulcrum. Anterior dislocation from an anterolateral blow is significantly more common than posterior dislocation from a posterolateral blow.
Imaging
Sternoclavicular dislocation can result in asymmetry of the clavicular heads. Compared to plain radiography, CT can better distinguish anterior from posterior dislocation. It is also able to detect associated injury to mediastinal structures such as great vessels, recurrent laryngeal nerve, trachea, and esophagus, in patients with posterior dislocation (Fig. 20.2).
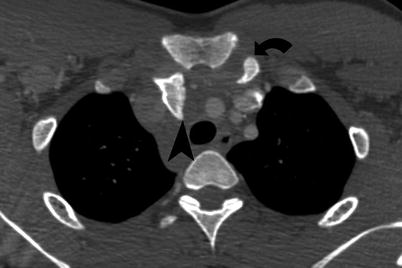
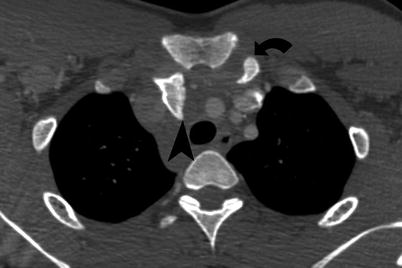
Fig. 20.2
Posterior dislocation of clavicle. Axial CT image depicts posterior dislocation of the right clavicle head (arrowhead) which is now situated within the superior mediastinum. The left sternoclavicular articulation (curved arrow) is normal
Acromioclavicular Dislocation
Acromioclavicular dislocation is a common injury usually resulting from direct trauma in contact sports, such as football or hockey. Dislocation can also result from a fall on an outstretched hand.
AP radiographs with a 10–15° cephalic tilt (Zanca view) are recommended for assessment of the acromioclavicular region. Dislocations are classified into the following types:
Type 1: Isolated sprain of the acromioclavicular ligament (AC). Plain films are normal aside from soft tissue swelling.
Type 2: Subluxation with rupture of the AC ligament and sprain of the coracoclavicular ligament (CC). The distal clavicle will typically be situated less than 5 mm superiorly to the acromion.
Type 3: Complete rupture of AC and CC ligaments with superior migration of the clavicle greater than 5 mm above the acromion (Fig. 20.3). Coracoid fracture and injuries to the insertion of the trapezius or deltoid muscles can occur as a result of type 3 dislocations.

Fig. 20.3
Acromioclavicular dislocation. AP view shows a type III acromioclavicular injury with elevation of the acromion more 5 mm from its normal position (arrowhead). This degree of displacement indicates rupture of both CC and AC ligaments
Glenohumeral Joint Dislocation
Because of its inherent instability, the glenohumeral joint is the most commonly dislocated joint in the body. Anterior dislocation is far more common than posterior and often results from an anterior blow to an abducted arm and less frequently from a direct injury to the shoulder. Posterior dislocation may be a consequence of electric shock or seizure and can therefore be bilateral. Inferior glenohumeral dislocation, known as luxatio erecta, results from hyperabduction of the arm and is suspected in a patient with an abducted arm, with the wrist resting on the head. Superior dislocation from an upward blow on an adducted arm represents the rarest type and is almost always associated with rotator cuff tear.
Imaging
In the setting of anterior glenohumeral dislocation, the AP radiograph will show the humeral head situated medial and inferior with respect to the glenoid, such that it lies directly inferior to the coracoid process (Fig. 20.4a). If posteriorly dislocated, the AP view will depict an increased distance between the humeral head and the glenoid and loss of the normal overlap of the humeral head and glenoid. However, it should be noted that a large effusion may have an identical appearance. The axillary projection (45° posterior oblique with 45° of inferior angulation) and scapular Y projection (60° anterior oblique) afford an excellent appraisal of the congruence of the glenohumeral joint (Fig. 20.4b). These latter views are often best for distinguishing between an anterior and posterior dislocation when the AP view is confusing.




Fig. 20.4
A. Glenohumeral dislocation. (a) AP view of the shoulder illustrates the typical appearance of anterior glenohumeral dislocation with the humeral head situated in a subcoracoid position (top). A postreduction AP view shows a wedge-shaped defect at the posterolateral aspect of the humeral head typical of a Hill-Sachs lesion (arrow). (b) Scapular Y view clearly demonstrates anterior dislocation of the humeral head which now lies under the coracoid process. (c) Axial CT shows wedge-shaped Hill-Sachs deformities on the posterolateral aspects of both humeral heads (arrows) after bilateral anterior dislocations. (d) MIP reconstruction of contrast-enhanced CT shows abrupt occlusion of the axillary artery (arrowhead) caused by anterior glenohumeral dislocation
Anteroinferior dislocation, or subcoracoid dislocation, can result in fracture of the posterolateral aspect of the humeral head (Hill-Sachs lesion), best seen as a linear or wedge-shaped defect that is evident on radiography (Fig. 20.4c). As the humeral head impacts against the glenoid rim, fracture of the anteroinferior glenoid (Bankart lesion) with avulsion of the labroligamentous complex can also occur. With nonoperative treatment, anterior dislocations will recur in approximately 50 % of cases [5].
Conversely, a reverse Bankart lesion, or posteroinferior fracture of the glenoid rim, can result from posterior dislocation. In evaluation of glenohumeral dislocation, CT is most appropriate for identifying bony fragments or associated vascular injury, while MRI can more clearly identify soft tissue damage (Fig. 20.4d).
Scapular Fracture
An isolated fracture of the scapula is uncommon and is usually the consequence of direct blunt trauma. It is usually accompanied by tenderness, fracture crepitus, and an adducted upper extremity.
Imaging
Fractures of the scapular body can be horizontal, vertical, or comminuted. CT is optimal for delineation of these fractures and identification of associated fractures.
Since scapular fractures are often accompanied by other injuries, they are frequently missed on AP chest radiographs as the associated injuries are either more clinically urgent (lung contusion, pneumothorax, widened mediastinum) or more obvious (clavicle and rib fractures).
Proximal Humerus Fractures
A fracture of the proximal humerus represents a common injury in the elderly population, most often occurring after a fall on an outstretched hand. Alternatively, a direct blow to the lateral shoulder can cause a head-splitting fracture by forcing the humeral head directly into the glenoid fossa. Most commonly, proximal humeral fractures occur at the surgical neck.
Imaging
The Neer classification system describes the severity of proximal humerus fractures according to the displacement of the four bone segments (greater tuberosity, lesser tuberosity, head, and surgical neck) [6]. Displacement is defined as greater than 1 cm or greater than 45° of separation from the anatomic position of the bone fragment. The majority of fractures are one-part fractures that are not associated with significant displacement of any segments.
Since the anterior circumflex humeral artery is closely associated with the surgical neck of the humerus, fractures may compromise the blood supply to the humeral head and result in avascular necrosis. Other complications of displaced fractures include rotator cuff tear and nonunion.
Supracondylar Fractures
Pediatric supracondylar fractures of the humerus are most frequently caused by axial loading on the elbow from a fall on an outstretched hand. Low impact falls can also result in supracondylar fractures in osteoporotic elderly patients.
Imaging
The radiographic findings include an elevated anterior or posterior fat pad, caused by hemarthrosis. A posterior fat pad sign may represent the sole finding in a patient with radiographically occult fracture [7]. Anterior displacement of the anterior humeral line which ordinarily transects the middle third of the capitellum is also a common finding (Fig. 20.5).
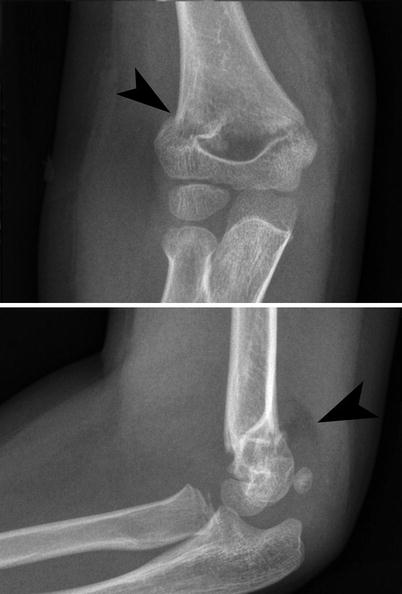
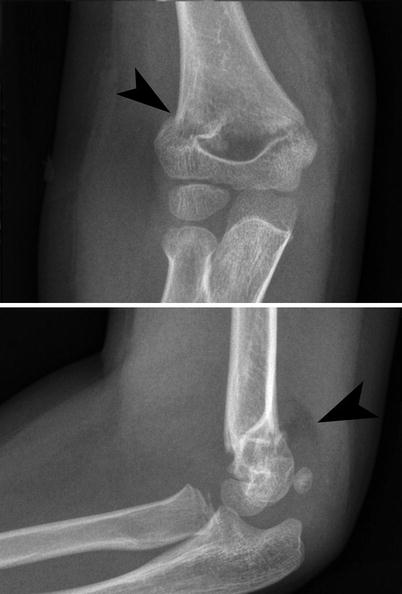
Fig. 20.5
Supracondylar fracture. AP projection of the elbow depicts a focal cortical step-off of the supracondylar humerus (arrowhead), indicative of supracondylar fracture (top). A lateral projection of the elbow shows the elevated posterior fat pad (arrowhead) which normally should not be seen and indicates an effusion. Also, the anterior humeral line passes through the anterior margin of the capitellum
Supracondylar fractures are traditionally classified by the Gartland system: class I is a non-displaced fracture; class II fractures have anterior cortical disruption; and class III fractures have both anterior and posterior disruption [8].
Radial Head Fractures
Radial head fractures are usually the result of axial loading from a fall on an outstretched hand where the radial head is forced into the capitellum. Less commonly, it occurs secondary to posterior elbow dislocation. Fractures are classified into four types: type I is non-displaced, type II is a displaced marginal fracture, type III fracture is comminuted, and type IV fracture is associated with elbow dislocation.
Imaging
On radiography, the fracture line may be subtle or radiographically occult. AP, lateral, and radiocapitellar views (angled 45° cephalad) may be obtained. Lateral radiographs may reveal or can reveal anterior and posterior fat pad signs which indicate hemarthrosis and are suggestive of an underlying radial head fracture. The radial head should be aligned with the capitellum in all views and any disruption of the radiocapitellar line indicates radial head dislocation.
Radial head fractures can be associated with elbow dislocation and fractures of the capitellum or coronoid process. Avulsion of the medial epicondyle may also result from excessive, valgus stress.
Medial and Lateral Condyle Fractures
Fractures of the humeral condyles represent a small fraction of elbow injuries with lateral fractures being more common than medial. Fractures of the condyles in the pediatric population are often Salter-Harris type IV fractures with involvement of epiphysis, physis, and metaphysis. Either condyle may be fractured as a result of a direct force applied to the elbow at an angle during flexion.
Radiographic findings may be subtle in the immature elbow, particularly distinguishing between condylar fractures and epicondylar fractures, which are extra-articular. Comparison with the contralateral extremity anatomy may be valuable. Stress views may be helpful with the application of valgus or varus forces under anesthesia. MRI, arthrography, or oblique radiographic views may also reveal slight displacement [9].
Associated injuries include elbow dislocation or associated fracture of the radial head. Additionally, fracture nonunion, valgus deformity, or ulnar neuritis can complicate recovery [10].
Medial Epicondyle Avulsion
Avulsion of the medial epicondyle of the humerus is a common sports-related injury in adolescents. It is the result of extreme valgus force on the apophysis secondary to contraction of the forearm flexors during pitching or arm wrestling.
If avulsion involves a bony fragment, it may be apparent on AP radiography. If bone is not fractured, then MRI or ultrasound is essential to assess for soft tissue injury.
Because of its close association with the medial epicondyle, damage to the ulnar nerve may occur.
Elbow Dislocation
Elbow dislocation is almost always caused by a fall on an outstretched hand triggering a posterior dislocation. Injury progresses in three stages: Stage 1 is associated with posterolateral ulnar subluxation with disruption of the lateral ulnar collateral ligament. A stage 2 injury is characterized by perching of the coronoid process inferior to the trochlea. When the coronoid rests posterior to the trochlea, the injury is classified as stage 3.
Ligamentous disruption can be best visualized on T2-weighted MR imaging and reveals complete tear of the lateral ulnar collateral ligament. The other findings may include disruption of the radial collateral ligament as well as injury to the brachialis muscle or tendon.
Complex dislocations may be associated with fractures (radial head, radial neck, coronoid process, or capitellum) or neurovascular injury (brachial artery or ulnar nerve). Late complications include myositis ossificans, leading to limitation of range of motion of the elbow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree