CT finding
CT grade
Score
Normal pancreas
A
0
Focal or diffuse enlargement of the pancreas
B
1
Inflammatory changes in peripancreatic fat
C
2
Single fluid collection
D
3
≥2 collections and/or gas in/adjacent to pancreas
E
4
Necrosis (%) | Score | |
|---|---|---|
<30 | 2 | |
30–50 | 4 | |
>50 | 6 |
Imaging
When imaging is required, contrast-enhanced CT and ultrasound are both considered first-line imaging modality for the initial assessment of acute pancreatitis in patients with elevated amylase and/or lipase but no fever or evidence of fluid loss (Fig. 11.1). Ultrasound is primarily used to assess for gallstones, and contrast-enhanced CT is the most appropriate imaging modality for the assessment of pancreatic parenchyma in children and adults. For the assessment of pancreatitis in patients who are not improving after 48 h of presentation, contrast-enhanced CT and MRI with MRCP are both considered the equally appropriate first-line imaging modalities (Fig. 11.2).
Fig. 11.1
Acute edematous pancreatitis. (a) Ultrasound shows pancreatic enlargement (arrowheads) with hypoechogenicity of the pancreatic parenchyma caused by pancreatic parenchymal edema. (b) Ultrasound shows hypoechoic pancreatic parenchyma and small peripancreatic fluid (white arrow)
Fig. 11.2
Acute edematous pancreatitis. (a) Contrast-enhanced CT image shows fat stranding around the pancreatic tail (arrowhead) due to oedematous pancreatitis. (b) Contrast-enhanced MR shows heterogeneous inflammation (arrowhead) around the pancreatic tail with thickening of the lateroconal fascia
Ultrasound is often limited by technical factors such as obesity and bowel gas, thereby limiting its usefulness for purposes other than biliary assessment. The CT imaging findings of acute pancreatitis include pancreatic enlargement, ill definition of the peripancreatic fat planes, extrapancreatic fluid collection, dilated pancreatic duct, and pancreatobiliary calculus (Figs. 11.3 and 11.4). Interstitial edematous pancreatitis is seen on CT as localized or diffuse pancreatic enlargement with homogeneous or heterogeneous enhancement. Necrotizing pancreatitis is characterized by lack of pancreatic parenchymal enhancement. The extent of pancreatic necrosis is categorized as less than 30 %, 30–50 %, and more than 50 % of the pancreas. Areas of no or poor enhancement in less than 30 % of the pancreas categorized as necrosis may on a follow-up CT actually represent changes of edematous pancreatitis rather than necrosis.
Fig. 11.3
Pancreatic collections. (a) Contrast-enhanced CT shows pancreatic enlargment due to a dominant pancreatic head collection (arrow). (b) Contrast-enhanced CT shows pancreatic parenchymal necrosis with intrapancreatic fluid (arrowheads) and air
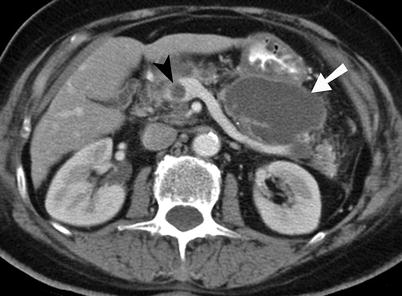
Fig. 11.4
Pancreatic collection. (a) Noncontrast CT obtained immediately after image-guided pigtail catheter placement demonstrates a large lesser sac fluid- and air-containing collection (white arrowheads). There are collections also seen in left posterior pararenal space and left paracolic gutter. (b) Follow-up contrast-enhanced CT image shows marked improvement in the lesser sac fluid collection (white arrowheads)
MRI is useful in stable patients because of the capacity of identifying as well as grading the inflammatory process and detecting ducts and their obstruction or disruption when present [2, 3, 7]. The detection of the type fluid composition is also possible on MRI in patients with complicated pancreatitis (e.g., hemorrhagic, necrotic) (Figs. 11.5 and 11.6).
Fig. 11.5
Acute pancreatitis on MRI. (a) TSE-T2-weighted sequence shows extensive hyperintense peripancreatic inflammatory process (arrowheads) in the left anterior pararenal space. (b) Post-gadolinium T1-weighted sequence in a patient with amylase level of 2,300 units per liter shows peripancreatic inflammation (arrowheads) and periportal edema (arrow). (c) Contrast-enhanced CT and corresponding FSE-T2-weighted MRI sequence shows pancreatic necrosis and large homogeneous fluid collection (arrows) within the pancreas
Fig. 11.6
Pseudocyst with bleeding. (a, b) Noncontrast-enhanced CT and T2-weighted MR image shows a large lesser sac pseudocyst (arrowheads) containing blood clots from recent bleeding
The complications of acute pancreatitis include hemorrhage, necrosis, abscesses, pseudocyst, and pseudoaneurysm [3] (Figs. 11.7, 11.8, 11.9, and 11.10). Symptomatic collections and pseudocysts are often best treated with image-guided catheter drainage. ERCP is used for diagnosis as well as treatment of stone-related pancreatitis and is often used when a stone is seen obstructing the pancreatobiliary duct on MRCP (Figs. 11.11 and 11.12).