Fig. 4.1
Duodenal diverticulum. Upper GI study demonstrates an incidentally detected solitary duodenal diverticulum arising from the third portion of the duodenum
Fig. 4.2
Small bowel diverticulosis. (a) Small bowel follow-through examination demonstrates innumerable round collections of contrast in small bowel diverticula. (b) Small bowel follow-through study demonstrates multiple duodenal and jejunal diverticula (arrowheads) seen arising from the mesenteric border of the small bowel
Congenital diverticula are true diverticula and are composed of all three intestinal layers and arise from the antimesenteric border of the small bowel. Meckel’s diverticula, for example, are true diverticula. By contrast, pathologic acquired diverticula are “pseudodiverticula”; that is, they lack a muscular layer and result from herniation of only the mucosa and submucosa through defects in the muscular layer. It is thought that acquired diverticula tend to form at the mesenteric border where vasa recta penetrate, creating areas of relative weakness [2]. Krishnamurthy et al. found histopathologic abnormalities in the wall of the jejunum of patients with jejunal diverticula, consistent with the notion that diverticula formation is associated with uncoordinated small bowel motility that results in increased intraluminal pressures [10].
Pathogenesis
Although most small bowel diverticula are of little clinical significance, approximately 10–20 % will develop complications [1]. Potential sequelae include inflammation, gangrenous change, perforation, peritonitis, bleeding, obstruction, and intestinal stasis leading to blind loop syndrome [11, 12]. Jejunoileal diverticula are more likely to have complications than duodenal diverticula [1, 13]. Of the diverticula that developed complications, jejunoileal diverticula were more likely to perforate and form abscesses, whereas duodenal diverticula were more prone to bleeding [1].
Diverticula in the small bowel are less likely to develop inflammation than those in the colon, probably due to the relative sterility of small bowel contents and the lesser degree of stasis that occurs in the larger diverticula of the small bowel [2]. Stasis of diverticular contents may be promoted by foreign bodies, enteroliths, inspissation of bowel contents, or a smaller diverticular ostium which can reduce the outflow of intestinal fluid from the diverticulum [2, 11, 14]. Because small bowel diverticulitis is more commonly found at the mesenteric side of the bowel, the mesentery can close off the localized inflammatory process from the rest of the peritoneal cavity. As a result, peritonitis and pneumoperitoneum may not be detected clinically or radiologically unless there is rupture of the mesenteric peritoneum that had previously sealed off the abscess [11].
Clinical Presentation
Small bowel diverticulitis presents a diagnostic challenge on clinical exam and can mimic a host of more common abdominal pathologies including acute appendicitis, cholecystitis, perforated peptic ulcer disease, and colonic diverticulitis [12, 15]. A patient with small bowel diverticulitis may present with intermittent abdominal discomfort, acute abdominal pain, fever, chills, and leukocytosis [4, 9, 16–21]. Peritoneal signs may be appreciated on abdominal exam [9, 18].
Imaging
In the setting of small bowel diverticulitis, barium study may allow detection of air- or contrast-filled diverticula along the mesenteric small bowel wall, thickening of the bowel wall, bowel lumen obstruction, or extraluminal flow of contrast (Fig. 4.3) [12].
Fig. 4.3
Acute small bowel diverticulitis in an acquired jejunal diverticulum. (a) A small bowel follow-through study demonstrates segmental irregularity of valvulae conniventes (curved arrows) in the proximal jejunum. A small collection of air due to the jejunal loop represents the inflamed jejunal diverticulum (straight arrows). (b) Coronal reformation (CT) demonstrates the inflamed jejunal diverticulum (straight arrow) in the left upper quadrant, with its neck (arrowhead) arising from the antimesenteric border of a jejunal loop. (c) Sagittal reformation (CT) demonstrates the inflamed true diverticulum (straight arrow) arising on the antimesenteric border of the jejunal loop (curved arrow)
The CT findings (Table 4.1) are typically a focal inflammatory mass containing air, fluid, or an air-fluid level adjacent to asymmetrically thickened small bowel wall, with the presence of surrounding inflammation and mesenteric fat stranding [3, 9, 12]. The small bowel wall thickening is most prominent on the mesenteric side. The inflamed diverticulum may be visible along the mesenteric border of the small bowel loop (Fig. 4.4). The differential diagnosis on CT may include a perforated neoplasm, perforation secondary to a foreign body, NSAID-provoked ulceration, intramural hematoma, and local inflammatory bowel disease [3].
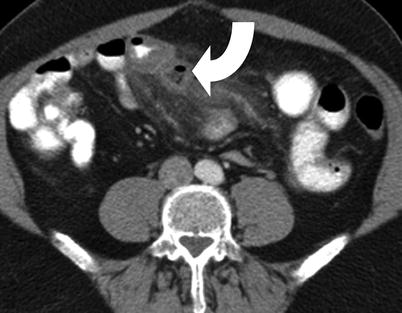
Table 4.1
Findings on plain radiograph of the abdomen
Up to two air-fluid levels in the bowel |
Small bowel caliber of less than 3 cm |
Psoas outline (visible in 80 %) |
Splenic outline (<15 cm in long axis) |
Renal outlines |
Gastric air |
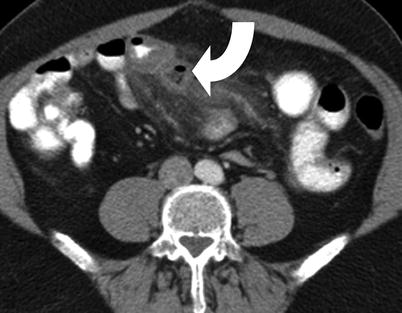
Fig. 4.4
Small bowel diverticulitis. Contrast-enhanced CT scan study of the abdomen demonstrates inflamed diverticulum (curved arrow) arising on the mesenteric aspect of the distal jejunal loop. There is inflammatory thickening of the adjacent small bowel wall along with inflammatory stranding in the small bowel mesentery
CT with multiplanar reconstruction can be employed to identify small bowel diverticula, with excellent visualization of the narrowed diverticular neck [2]. CT with coronal reformatting is especially useful for detecting single diverticula that are difficult to detect on axial views and can allow recognition of additional diverticula [3, 14].
CT Findings of Acute Small Bowel Diverticulitis
1.
Inflamed diverticulum or focal inflammatory phlegmon along the mesenteric border of small bowel.
2.
Asymmetrically thickened small bowel wall, more prominent along the mesenteric border.
3.
Mesenteric fat stranding.
Meckel’s Diverticulitis
Meckel’s diverticulum is the most common congenital anomaly of the GI tract, seen in approximately 2 % of the population. It is a true diverticulum and is therefore present on the antimesenteric border of the distal ileum. It is most commonly located within 100 cm of the ileocecal junction [22]. It contains hypertrophic gastric mucosa (in 25–50 %) and has a lifetime complication risk of up to 4 %. Heterotropic pancreatic tissue is present in approximately 10 % of the cases.
The majority of cases of symptomatic Meckel’s diverticulum are seen in the pediatric population. Hemorrhage is the most common complication and is most often painless. Bowel obstruction is the second most common complication and is usually seen in older children and adults. The bowel obstruction can be secondary to volvulus, intussusception, or hernia.
Meckel’s diverticulitis most often presents with abdominal pain and fever. It is secondary to obstruction of the mouth of the diverticulum most commonly by an enterolith, fecolith, or foreign body. Littre hernia represents Meckel’s diverticulum which has herniated in a hernia sac.
Meckel’s diverticulum can be seen on barium studies as a blind-ending tubular outpouching arising from the antimesenteric border of the ileum with a triradiate fold pattern at the junction of the diverticulum and ileum.
The heterotopic gastric mucosa present in a Meckel’s diverticulum accumulates and secretes pertechnetate anion and is therefore detected on technetium-99m pertechnetate scan as a focal area of increased radiotracer activity (Fig. 4.5). Technetium pertechnetate scintigraphy has high sensitivity of more than 80 % in the pediatric population and slightly lower sensitivity of 63 % in adult population [23]. CT may show changes of small bowel diverticulitis in the right lower quadrant or may show volvulus or intussusception (Fig. 4.6).
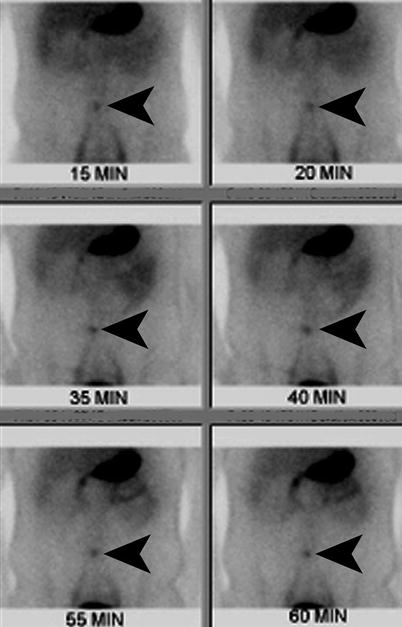

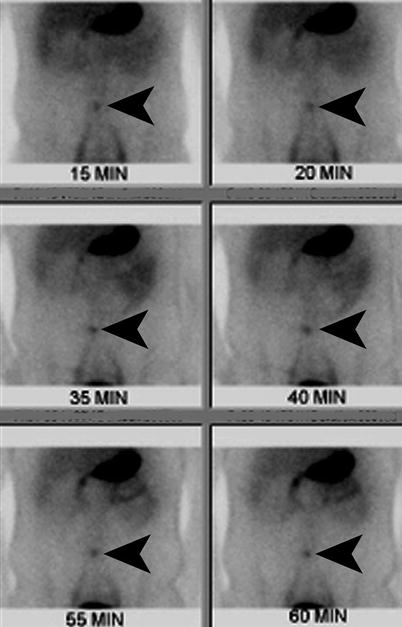
Fig. 4.5
Meckel’s diverticulitis. Technetium-99m pertechnetate scan demonstrates focal increased radiotracer activity (arrowheads) in the lower abdomen, corresponding to the site of ectopic gastric mucosa within the inflamed Meckel’s diverticulum

Fig. 4.6
Meckel’s diverticulitis. Contrast-enhanced CT demonstrates the inflamed congenital diverticulum with thickened wall arising from the antimesenteric border of the distal ileum
Treatment
Laparotomy or laparoscope-assisted surgery is typically undertaken in the setting of small bowel diverticulitis associated with perforation, abscess formation, massive GI bleed, small bowel obstruction, blind loop syndrome, or refractory abdominal pain [24, 25]. Surgical approaches include both segmental resection of the involved bowel with end-to-end anastomosis and less commonly diverticulectomy [8, 24]. Conservative management consists of antibiotic therapy, IV hydration, and bowel rest [2, 3]. However, cases have been described of patients who ultimately underwent segmental bowel resection for jejunal diverticulitis, after symptoms persisted following a period of conservative management [3].
Acute Mesenteric Ischemia
Acute mesenteric ischemia is characterized by inadequate blood flow to the bowel wall, leading to ischemia. Mesenteric arterial occlusion carries a high mortality, unless the patient undergoes emergent vascular surgery.
Clinical Presentation
Clinically the patients with arterial causes of acute mesenteric ischemia are elderly and most often present with severe dull abdominal pain and vomiting. The abdominal pain is out of proportion to the tenderness elicited on palpation. Mesenteric venous thrombosis is most often seen in younger population and present with less severe symptoms which may have been present for days or sometimes weeks. Lab studies often show metabolic acidosis, elevated lactate level, and low bicarbonate level.
Pathogenesis
Superior mesenteric artery occlusion is a far more common than superior mesenteric vein occlusion as the cause of acute mesenteric ischemia. Approximately one-third of the cases are secondary to embolic occlusion and one-third secondary to thrombosis. Approximately 25 % cases are caused by nonocclusive ischemia, while the remaining cases are secondary to venous occlusion [26].
Risk Factors
The risk factor for arterial occlusion is most commonly heart diseases, such as atrial fibrillation, endocarditis, and valvular heart diseases. Atrial fibrillation is the most common cause of embolism to the superior mesenteric artery. The nonocclusive bowel ischemia may be secondary to hypotensive shock, pancreatitis, bowel obstruction, dehydration, and dialysis. Mesenteric venous thrombosis is seen with hypercoagulable states, such as protein C or S deficiency, polycythemia vera, antithrombin three deficiency, sickle-cell disease, pregnancy, and oral contraceptive use.
Imaging
The plain radiograph may show no abnormality or show paralytic ileus. Contrast-enhanced CT is the imaging modality of choice as it has sensitivity of 93.3 % and specificity of 95.9 % in a meta-analysis of 6 studies published between 1996 and 2009 [27]. Although catheter angiography has been shown to have a sensitivity of 87.5 %, the introduction of multidetector CT has obviated the need for this invasive test as the first-line imaging modality.
Biphasic CT performed 25 and 65 s after initiating contrast injection at the rate of 4 mL/s is the optimal protocol to evaluate for vascular as well as bowel wall changes. The CT angiographic phase changes management in 19 % cases by showing vascular abnormality not visible on the portal venous phase [28].
The CT imaging findings include superior mesenteric artery thrombus, small-caliber superior mesenteric vein, bowel distension, and focal lack of bowel wall enhancement (Figs. 4.7 and 4.8). In the study by Kirkpatrick et al., pneumatosis intestinalis was seen in 43 % cases of acute mesenteric ischemia. Bowel wall thickening and mucosal enhancement were seen in 85 and 46 %, respectively [28]. Linear pattern of pneumatosis indicates more serious cause of pneumatosis and accounts for higher proportion of death from bowel infarction than cystic pattern of intramural gas (Fig. 4.9). The presence of portomesenteric venous gas favors more serious causes of pneumatosis intestinalis, such as mesenteric ischemia, and increases mortality to 50 % (Fig. 4.10) [29]. The secondary findings seen on CT include ascites and mesenteric edema.
Fig. 4.7
Superior mesenteric artery and venous pathologies leading to bowel ischemia. (a and b) Color Doppler ultrasound and contrast-enhanced CT shows dissection in the superior mesenteric artery (arrowhead). The adjacent superior mesenteric vein is patent. (c) Superior mesenteric arteriogram shows narrowing (arrowheads) of the superior mesenteric artery lumen, secondary to nonocclusive thrombosis. (d and e) Contrast-enhanced CT shows thrombosis of the superior mesenteric vein (arrowhead). There are edematous changes seen in the small bowel mesentery. Ischemia in the small bowel is indicated by bowel wall edema (arrow)
Fig. 4.8
Transmural infarction of bowel. (a) Plain radiograph of the abdomen demonstrates multiple air-fluid levels secondary to paralytic ileus. (b and c) Coronal CT reformation demonstrates fluid-containing, dilated small bowel loops (arrowheads) with no wall enhancement
Fig. 4.9
Pneumatosis intestinalis. (a) Plain radiograph of the abdomen demonstrates extensive linear pneumatosis (arrowheads) in the small bowel wall. (b) Contrast-enhanced CT shows pneumatosis (arrowheads) in the small bowel wall, secondary to bowel wall ischemia
Fig. 4.10




Portal vein and superior mesenteric venous air in bowel infarction. (a) Noncontrast CT shows extensive air in portal vein branches (curved arrows). (b) Contrast-enhanced CT shows air in a superior mesenteric vein tributary (arrowhead), in a patient with bowel ischemia and portal vein gas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree