2Great Ormond Street Hospital, London, UK
- The common types of paediatric emergency differ with the age of the presenting child
- Paediatric fractures exhibit different types and patterns to adults
- Ultrasound is often the first line investigation of paediatric abdominal emergencies
- Be vigilant for possible non-accidental injury
- Minimise radiation exposure wherever possible
Children make up about one-third of all patients who attend emergency departments (Box 16.1). Skeletal injuries in infants (<1 year), children (>1 year), adolescents and adults all differ greatly.
- Premature infant: ≤37 weeks’ gestation
- Neonate: birth to 28 days old
- Infant: 1 month–1 year old
- Toddler: 1–3 years old
- Child: ≥3 years old
Children are more agile, more flexible and lighter than adults. When they fall, the forces generated are smaller. Boys sustain more injuries than girls, and most injuries occur at home or playing sport at school (Box 16.2).
- Children often present at accident and emergency departments
- Boys present more commonly than girls
- Seasonal variations in the type of injury occur
- Children have different problems to adults
Fractures in infants are rare. Toddlers tend to sustain skull and tibial fractures, whereas distal forearm, ankle and foot injuries are often seen in schoolchildren.
Minimising radiation exposure is an important principle in medical imaging. Children have an increased sensitivity to the risk posed from X-ray radiography. As such, any request for radiographs should give a clear indication and ask a relevant question.
This chapter gives an overview of common paediatric fractures and other radiological emergencies (Figure 16.1). It outlines a systematic approach of how to interpret the relevant radiographs. Common fractures in the paediatric population will be discussed, followed by a list of common abdominal and other childhood emergencies.
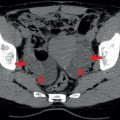
Figure 16.1 Anteroposterior view of the right knee in a child.
Fractures
Fractures in children are different to those in adults because of anatomical, biomechanical, and physiological differences. In addition, a range of fractures is caused in children, because paediatric bones are softer and more pliable than adult bones.
Anatomy
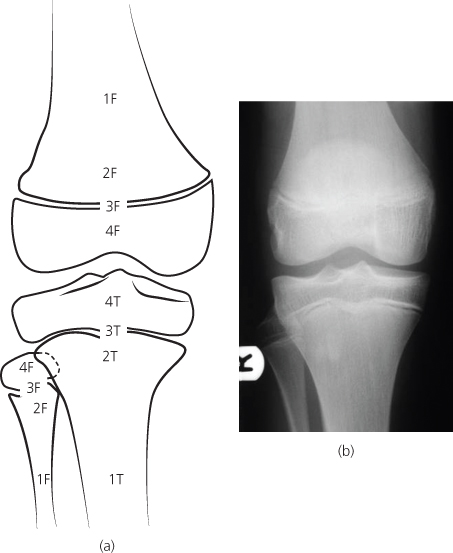
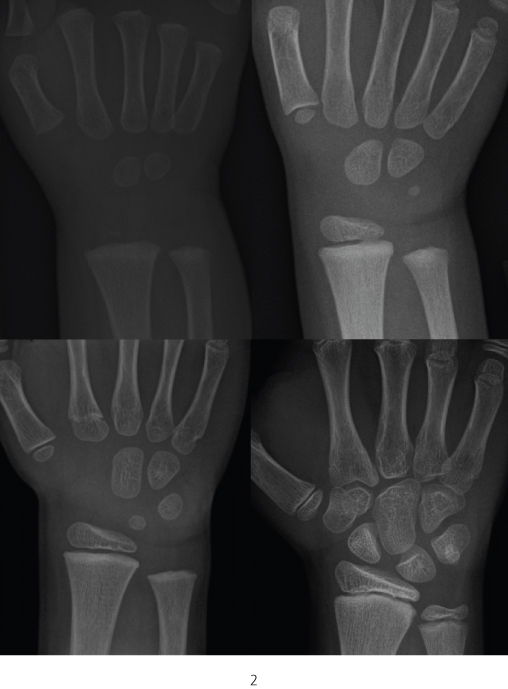
At birth, many bones or the ends of bones are not visible. In time, ossification centres appear (sometimes several); they enlarge and coalesce, eventually fusing to the adjacent bone. The time interval between these changes varies from bone to bone. Predictable timescales vary slightly between boys and girls, and between different ethnic origins (Figure 16.2).
Figure 16.2 Radiographs of the wrist in children at 18 months (top left), 3 years (top right), 6 years (bottom left), and 12 years (bottom right).
The physis (growth plate) is avascular after infancy. Damage to this area is shown radiographically by changes in its width or changes in adjacent bone. Damage to the epiphyseal vessels leads to death of the physeal chondrocytes and growth arrest.
The periosteum in the paediatric population is thick and strong. The attachment of the periosteum to the shaft of the bone is loose in children, and so periosteal reactions and subperiosteal collections are common.
Biomechanical differences
Paediatric bones are more porous than adult bones, and they can bend more without breaking. The weak point lies at the physis, and so physeal fractures are common before bony fusion. The thick, strong periosteum resists displacement of the fracture (unless it is torn).
Physiological differences
Fractures heal faster in children than in adults, and remodelling is quicker because children have rapid bone turnover. Normal alignment occurs in the plane of motion of the adjacent joint. Fracture healing results in longitudinal overgrowth, therefore in long bone diaphyseal fractures, overlap (up to 2 cm of bone) is accepted. The fracture should be described like an adult fracture—for example, transverse, oblique, comminuted, or compound. After the age of 12 years, fractures are treated more like those in the adult population due to slower remodelling.
Types of fracture
Types of fracture are shown in Figure 16.3.
Figure 16.3 Types of fracture.
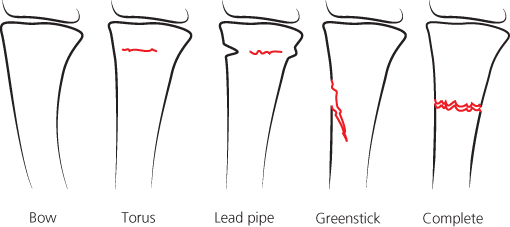
Complete diaphyseal fractures—The fracture site should be examined for an underlying bony abnormality, such as a bone cyst or generalised demineralisation. For infants and the non-ambulant, a careful history should be taken to exclude non-accidental injury.
Torus or buckle fractures—Failure on the compression side of a bending bone causes a torus or buckle fracture—an outward buckling of the cortex margin (torus is a latin term for bulge or swelling). Torus fractures usually occur near the metaphysis, where the cortex is thinnest. They often occur at the distal radius due to a fall on an outstretched hand (Figure 16.4).
Figure 16.4 Lead pipe fracture of the distal radius (arrow) and complete fracture of the distal ulna.
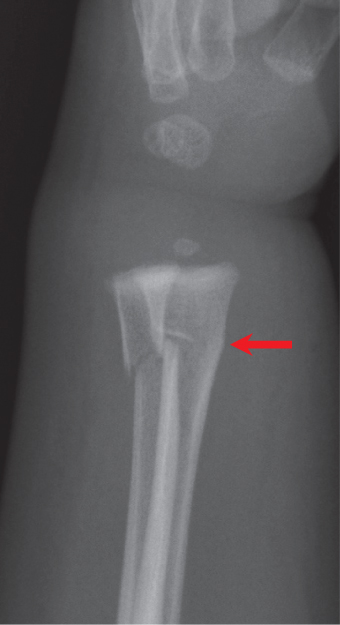
Greenstick fracture—When a bone is bent beyond its limits, a greenstick fracture is produced. It is caused by the bone bending on the compression side, with complete failure on the tension side of the bone. The fracture may later hinge open because of muscle pull (Figure 16.5).
Figure 16.5 Greenstick fracture of the mid radius (arrow).

Bowing injuries—caused by acute plastic deformation of the bone secondary to longitudinal stress. An increase in longitudinal compression leads to bowing, buckle fractures, lead pipe fractures (Figure 16.6), greenstick fractures, and complete fractures.
Figure 16.6 Torus fracture of the distal radius (arrow).

Physeal fractures
Salter–Harris classification
The standard classification for physeal injuries is that of Salter and Harris (Box 16.3; Figure 16.7). This classification divides the common types (I–IV) according to the course of the fracture through the physis and the adjacent epiphyseal and metaphyseal bone. Type V injuries are rare, may be occult radiographically, and are caused by compression of the physeal cartilage (Box 16.4).
Figure 16.7 Salter–Harris classification for physical injuries.
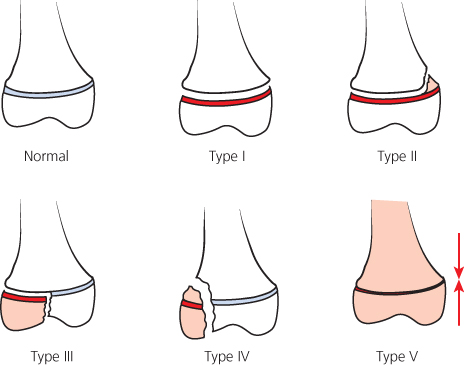
- Type I—Slipped or separated
- Type II—Above
- Type II—Lower
- Type IV—Through
- Type V—Evenly rammed
Figure 16.8 Salter–Harris type I fracture of the distal phalanx of the ring finger. Compare this with the normal epiphysis of the neighbouring digit.

Type I (incidence 6% of Salter–Harris fractures)
- Common locations—proximal humerus, distal humerus, proximal femur, distal tibia, and distal fibula
Type II (incidence 75% of Salter–Harris fractures)
- Common locations—distal radius, distal tibia, distal fibula, distal femur, distal ulna, and phalanges
Type III (incidence 8% of Salter–Harris fractures)
- Common locations—distal tibia, proximal tibia, and distal femur
Type IV (incidence 10% of Salter–Harris fractures)
- Common locations—distal humerus, and distal tibia
Type V (incidence 1% of Salter–Harris fractures)
- Common locations—ankle and knee
Type I
These are caused by a shearing stress through the physis (Figure 16.8). Most apophyseal injuries and slipped upper femoral epiphyses are type I fractures. Neonates may sustain these fractures at the proximal humerus. In the prepubertal child, a supination-inversion injury of the ankle may result in a type I fracture through the distal fibula. Invariably, this fracture will be reduced at the time of presentation and radiographical assessment. Type I fractures have a good prognosis.
Type II
These are the most common physeal fractures (75% of physeal fractures). The avulsion or shearing force fractures the physis and extends into the metaphysis (Figure 16.9). Radiographs show a triangular metaphyseal fracture known as the Thurston–Holland fragment. Between one-third and one-half of all type II injuries involve the distal radius. Reduction of the fracture is usually uncomplicated, and these injuries have a good prognosis.
Figure 16.9 Salter–Harris type II fracture of the distal tibial metaphysis (arrow). There is also a transverse fracture of distal fibula.

Type III
Type III injuries are partly intra-articular, with splitting of the epiphysis and a transverse fracture through the physis (Figure 16.10). As they involve all layers of the physis, they cause growth arrest. Type III injuries occur in adolescents about the time of closure of the physis and they often require operative reduction to prevent displacement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree