2The London Independent Hospital, London, UK
- The only imaging modality that is portable and real-time
- Can be used for diagnosis and treatment/intervention
- Quick, easy and safe—no radiation, so therefore safe for children and pregnancy
- MUST BE ADEQUATELY TRAINED BOTH FOR DIAGNOSIS AND INTERVENTION
- NB Clinicians must therefore be aware of their limitations
Ultrasound (US) is the only imaging modality that is portable and real-time (Figure 15.1). US is now readily available to all clinicians and used widely in all clinical settings. The absence of ionising radiation makes it safe for all patient groups, in particular in children and pregnancy. US offers a quick and easy evaluation to diagnosis and to assist interventions.
Due to its portability, US is the only imaging modality that can be used at the emergency scene and—in addition to plain films—can be used in the emergency room (ER) without needing to move the patient.
US can be used in virtually any clinical setting, BUT operators need to be suitably trained and in particular need to understand their limitations and the limitations of US.
Short, focused training is sufficient for a novice to do a focused assessment with sonography for trauma (FAST), further directed training is necessary to detect aortic abdominal aneurysms (AAA), but specialist training is necessary for its general use in the abdomen, chest and in particular for intervention.
All patient groups presenting to ER can benefit from ultrasound, from the diagnosis of a deep vein thrombosis (DVT) to checking viability of a foetus, to aiding intervention in major trauma (insertion of arterial lines, central lines or chest drains).
Knowledge of the basic principles of US, artefacts and ‘knobology’ (where the buttons are and what they do!) is invaluable, but beyond the scope of this chapter (Box 15.1).
- Selection of probes
- Selection of setting (abdomen, vascular, soft tissues…)
- Depth
- Focal zone
- Freeze/cine review
- Imaging—print or video
Figure 15.1 Ultrasound machine and probes.

- Low frequency—abdomen, pelvis and chest
- Medium/high frequency—children, vascular, MSK, neck and scrotum
ABCs systematic assessment—emergency uses
- A—appendicitis, AAA, ascites
- B—bladder
- C—calculi (gallbladder and kidneys), cardiac assessment (asystole), cysts
- D—DVT
- E—effusions/fluid (pleural, pericardial, peritoneal collections),
- F—FAST, foreign body (FB), foetus
- G—gallbladder
- S—soft tissues, skeleton
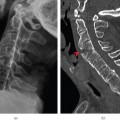
Appendicits
The classical appearances of appendicitis (Figure 15.2) are a blind ending, dilated thick-walled structure/viscus with an appendicolith. Ancillary features may suggest the diagnosis—aperistaltic small bowel loops, localised fluid and a positive provocation test (pain on direct palpation with the probe). Unfortunately, the normal appendix is rarely visualised in adults and even in children and therefore US cannot reliably exclude the diagnosis.
Figure 15.2 Appendicitis. Dilated blind-ending non-compressible thick-walled structure.
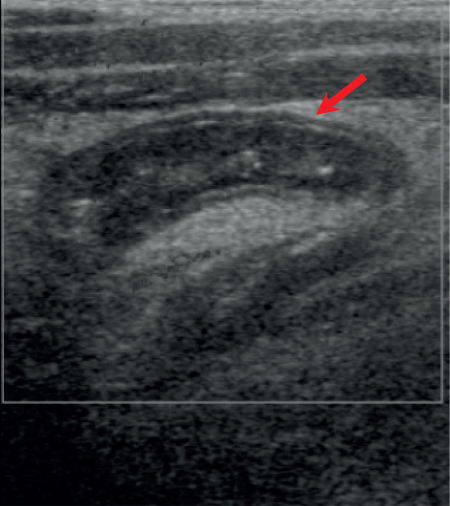
Figure 15.3 (a) TS and (b) LS ultrasound of abdominal aortic aneurysm. L, lumen; T, thrombus.
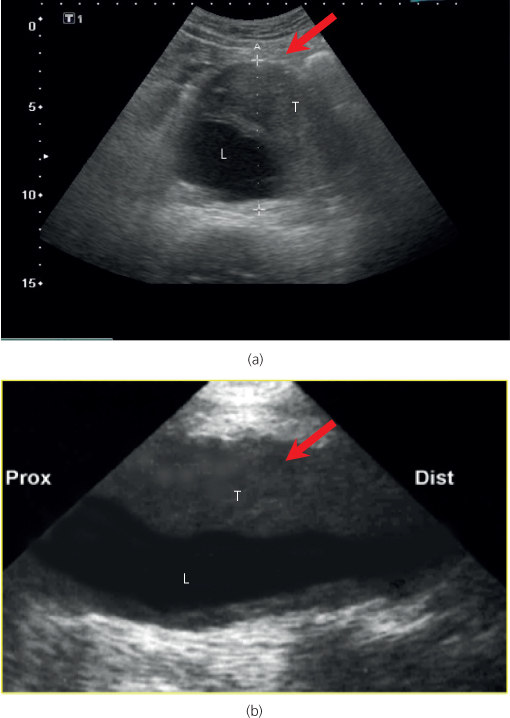
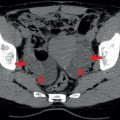
Abdominal aortic aneurysm
US reliably detects AAA (Figure 15.3), but cannot be reliably used to exclude a leak. Therefore in the correct clinical setting, CT should be performed if the patient is haemodynamically stable.
Ascites
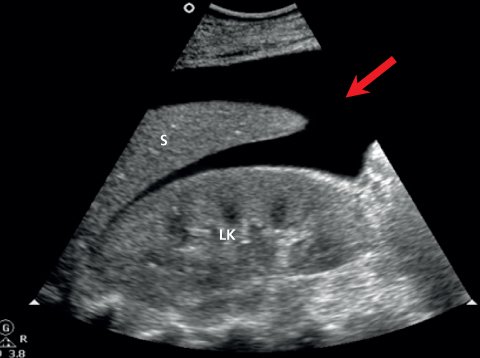
US can detect even small volumes of intraperitoneal fluid, but is poor at determining the nature of the fluid (blood, pus, fluid) (Figures 15.4 and 15.5).
Figure 15.4 Left upper quadrant: ascites with normal spleen (S) and left kidney (LK).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree