Acute inflammatory and infectious soft tissue disorders are important conditions that affect nearly 2 million people in the United States every year. Inflammation versus infection of the skin, subcutaneous tissues, and muscles is often difficult to differentiate clinically, and early detection and accurate diagnosis have a significant impact on the immediate course of treatment and on the magnitude of any subsequent complication and morbidity. Although many of these conditions present with similar clinical symptoms, the recognition of key laboratory and constitutional findings can aid in the diagnosis of specific diseases and determine whether surgical intervention is required. In many situations, important differentiating characteristics on imaging enable diagnosis.
Cellulitis
Cellulitis is a localized infectious process that affects the dermal layers and subcutaneous fat. The infection often begins with minor disruption of the skin that allows the invasion of microorganisms into the subcutaneous tissues. There is an increased risk in patients with diabetes mellitus, peripheral vascular disease, human immunodeficiency virus (HIV) infection, immune deficiency from other disease processes, or a retained foreign body. The most common organism involved is Staphylococcus aureus . Typically patients present with fever, focal pain and swelling, erythema and warmth, and leukocytosis.
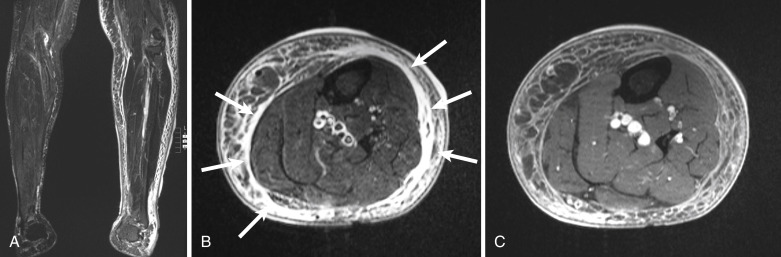
Radiographically cellulitis manifests with soft tissue swelling causing induration of the subcutaneous fat. On computed tomography (CT), swelling may focal or diffuse, with altered soft tissue attenuation that enhances variably with intravenous administration of iodinated contrast. Skin thickening can accompany the underlying inflammation. Although magnetic resonance imaging (MRI) rarely is required for diagnosis of cellulitis, this modality is indicated when the character of the disease is atypical, either because of suspected abscess formation, neoplastic disorder, or a rapidly progressive nature that can compromise a limb or become life threatening. Foreign bodies are frequently the nidus of infection in the foot and hand. Ultrasonography is the preferred modality for identifying retained foreign bodies, particularly those of wooden composition.
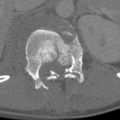
On MRI, cellulitis is characterized by focal or diffuse regions in the subcutaneous fat of low signal intensity on T1-weighted images with corresponding striated high signal intensity on fluid-sensitive sequences ( Fig. 17-1 ). Enhancement occurs after administration of intravenous gadolinium, differentiating these findings from nonspecific soft tissue edema. The adjacent fascia may also enhance.
Abscess
A focal soft tissue infection may become diffuse and evolve into a phlegmon or become more localized into an abscess. A phlegmon is a purulent inflammatory process that may either spread or become walled off into an inflammatory mass, often occurring without a bacterial infection. An abscess is a well-demarcated collection of purulent fluid that has accumulated as a result of an infectious process. It is differentiated from a phlegmon by the formation of a capsule in an attempt to contain the infected fluid from adjacent structures. The clinical presentation of both processes may be similar to that of cellulitis. An abscess, however, requires drainage in addition to appropriate antibiotic treatment. Frequently S. aureus is isolated as the infectious agent, and as many of 51% of infections may be methicillin resistant.
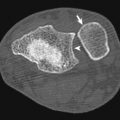
Unless gas is conspicuous, an abscess may be difficult to identify on radiographs. An abscess has a distinctive appearance on contrast-enhanced CT, with a brightly rim-enhancing fluid collection with an irregularly thickened wall ( Fig. 17-2 ). Internal attenuation is variable and influenced by the amount of cellular debris and protein in the fluid. The hallmark of an abscess is gas within the fluid collection. On MRI an abscess is characterized by a localized fluid collection with intermediate to low signal intensity on T1-weighted images and bright signal intensity on fluid-sensitive sequences. The developed wall is often irregular and thick and enhances peripherally after intravenous administration of gadolinium contrast material.

Necrotizing Fasciitis
One of the most serious complications of a soft tissue infection is necrotizing fasciitis, an infectious process that has spread to the deep fascial layers. This rare disorder is a life-threatening condition characterized by progressive necrosis of the subcutaneous tissue and fascia and frequently accompanied by severe systemic toxicity. Clinically, early necrotizing fasciitis mimics cellulitis with fever, pain, tenderness, swelling, and erythema. An important observation is severe pain at onset that is out of proportion to local findings. It may be difficult to discern between necrotizing fasciitis and diffuse cellulitis, but necrotizing fasciitis is a rapidly progressive infection that requires surgical débridement of the infected tissues. Intermediate skin changes include a serous-filled blister or bullae formation with skin fluctuance and induration. Late findings include hemorrhagic bullae, skin anesthesia, crepitus, and skin necrosis with discoloration.
The prevalence of necrotizing fasciitis is increasing owing to a larger population of patients with immune deficiency, including HIV infection, diabetes, organ transplantation, cancer, alcoholism, and chronic liver or renal disease. Intravenous drug abusers particularly are at risk for developing necrotizing fasciitis in the upper extremity. Necrotizing fasciitis is classified into four categories according to the causative microorganism. Type 1 necrotizing fasciitis is a polymicrobial infection with both aerobic and anaerobic bacteria occurring in individuals with chronic diseases. Type 2 necrotizing fasciitis is usually a monomicrobial infection with group A β-hemolytic streptococcus. It can affect people at any age and with no preexisting medical condition. Type 3 necrotizing fasciitis is an infection with a gram-negative monomicrobial infection with a marine-related organism or Clostridium species and is most prevalent in patients suffering from liver cirrhosis and alcoholism. Type 4 necrotizing fasciitis is a fungal infection usually affecting immunocompromised patients.
Early surgical intervention has been associated with improved survival. The current recommendation is wide, extensive débridement of all tissues that can be easily elevated off the fascia with gentle pressure, a characteristic of necrotic and poorly perfused tissue. Hyperbaric oxygen may be a useful adjunctive therapy. Today the reported mortality rate ranges from 22% to 30%, although some studies still report a mortality rate as high as 80%. High mortality rate is directly related to delayed diagnosis, as well as the type of necrotizing fasciitis. Common causes of death are sepsis, respiratory failure, renal failure, and multiorgan failure.
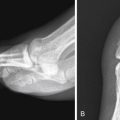
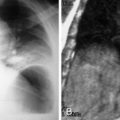
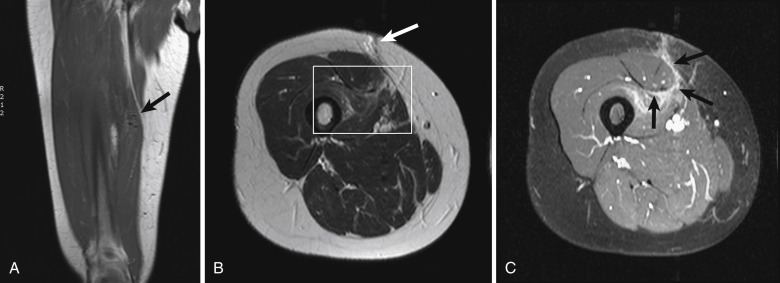
The diagnosis of necrotizing fasciitis is difficult on radiographs because only 13% of patients present with soft tissue gas. Computed tomography demonstrates induration of the subcutaneous fat, but when there is fluid and gas dissecting along the fascial planes, the diagnosis is apparent. Magnetic resonance imaging is the preferred modality for diagnosis, but it should not delay treatment if it is not readily available. The early findings of necrotizing fasciitis are similar to cellulitis ( Fig. 17-3 ). On T1-weighted images, necrotizing fasciitis is depicted by areas of soft tissue edema and enhancement with administration of intravenous gadolinium. Infected deep and intramuscular fascia is characterized by increased signal intensity on both sides of the fascia on fluid-sensitive images, representing purulent perifascial fluid (liquefaction necrosis) and edema, and this finding is not typical of uncomplicated cellulitis. The appearance of a thickened fascia greater than 3 mm thick should increase the index of suspicion ( Fig. 17-4 ). Early in the disease there is enhancement of the deep fascia, but as necrosis progresses, diminished enhancement of the fascia is observed. Low signal intensity on fat-saturated T2-weighted images is characteristic of necrotizing fasciitis, indicating formation of gas ( Fig. 17-5 ). Bandlike edema in the periphery of adjacent muscles indicates progressive disease. Loculation into an abscess indicates progression of the disease. A lack of fascial enhancement is associated with frank necrosis and is a manifestation of advanced necrotizing fasciitis, characteristically involving three or more compartments in the affected extremity.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree