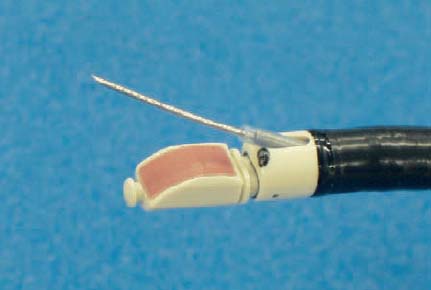
29 Endobronchial Ultrasound Pathological evaluation of mediastinal lymph nodes in lung cancer is essential for accurate staging and planning of effective treatment.1 Locoregional spread involves mediastinal lymph-node involvement, and this is a major determinant of surgical resectability. Despite the advances in surgical treatment and multimodality treatment, lung cancer is still the leading cause of death from malignant diseases worldwide. Accurate staging of the disease is important not only in order to determine the prognosis, but also to decide on the most suitable treatment plan for both operable and inoperable patients with non-small cell lung cancer (NSCLC). During the staging process, accurate mediastinal lymph-node staging is one of the important factors that affect the management of patients. Conventional imaging methods available for evaluating the mediastinum, such as computed tomography (CT), are inaccurate in the diagnosis of mediastinal lymph-node metastasis.2 Positron-emission tomography (PET) has been reported to increase the diagnostic yield.3 The increasing use of minimally invasive techniques and day-case procedures has renewed interest in the use of transbronchial needle aspiration (TBNA) for mediastinal lymph-node staging. Conventional TBNA relies on “blind” needle puncture, guided by static CT scans. The technique is highly operator-dependent, and reported sensitivities vary widely, between 15% and 78%.4 Higher yields are noted from the subcarinal station and when lymphadenopathy is present. However, due to the discouraging results that many operators obtain during their initial experience with the technique, recent surveys have shown that only 25% of pulmonologists use TBNA.5,6 Endobronchial ultrasound (EBUS) using a radial probe is an imaging technique capable of detecting even small mediastinal lymph nodes.7 However, imaging alone is inaccurate. Tissue confirmation of suspected malignant lymphadenopathy is therefore required, especially before surgical resection. Various invasive and noninvasive methods have been used to obtain tissue confirmation. In particular, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is a well-known modality with a high yield for tissue sampling of the mediastinum. In favorable conditions, lymph nodes can be detected with EBUS down to a size of 2–3 mm, and the internal structure (sinuses and folliculi) as well as small lymph vessels can be analyzed. The results of transbronchial needle aspiration (TBNA) can be significantly improved using endosonographic localization of lymph nodes, with a sensitivity of up to 85%.8 This is especially true for positions in which reliable landmarks on the CTare missing—for example, in high and low paratracheal locations. Herth et al.9 investigated the results of EBUS-guided TBNA in comparison with conventional TBNA. In this randomized study, the authors confirmed that the yield of EBUS-guided TBNA is higher than that of conventional TBNA (85% versus 66%). In an additional analysis of the lymph-node stations, they showed that particularly in locations that lack endoscopic landmarks (lymph-node stations 2, 3, and 4 in the Mountain and Dresler scheme10), the detection technique is helpful for increasing the yield. On the other hand, it was also demonstrated that when there are enlarged subcarinal nodes, conventional TBNA has the same yield as TBNA after EBUS detection.7 Since the development of the EBUS-TBNA scope, the use of miniprobes for TBNA guidance has dramatically declined. Description of the EBUS-TBNA Endoscope and Needle The flexible ultrasonic bronchoscope (Olympus XBF-UC40P; Olympus, Tokyo, Japan) (Fig. 29.1) has an outer diameter of the insertion tube of 6.7 mm, with a working length of 550 mm (total length 870 mm). The instrument has a small, curved linear-array electronic transducer 10 mm long located at the distal end of the endoscope in front of a 30° oblique forward viewing fiberoptic lens (with an angle of view of 80°) (Fig. 29.2). The diameter of the distal end of the endoscope with the transducer is 6.9 mm. The angulation range of the distal end of the endoscope is 160° upward and 90° downward. The endoscope has a biopsy channel of 2 mm. The ultrasonic frequency is 7.5 MHz, with a penetration depth of 4–5 cm. The depth of imaging can be adjusted from 2 to 9 cm at 1-cm intervals. The scanning direction is parallel to the longitudinal axis of the endoscope, with a scanning angle of 50°. This allows full ultrasonic monitoring of a needle when inserted via the biopsy channel during scanning. The endoscope can either be connected to an Olympus ultrasound processor (Olympus EU-121 C2000) or to an Aloka ultrasound scanner. A balloon, which can be filled with water, can be mounted around the transducer for better ultrasonic coupling with the bronchial wall. The ultrasound images can be frozen, and the size of lesions can be measured in two dimensions by placing cursors. The system also has a Doppler mode. Fig. 29.1 The linear-array ultrasound bronchoscope (Olympus BF-UC40F-OL5; Olympus Ltd., Tokyo, Japan). A dedicated 22-gauge needle (Olympus NA-201SX-4022) was developed for carrying out transbronchial aspiration (Fig. 29.3). The inner diameter of the needle is nearly equal to that of a conventional 21-gauge needle, which allows sampling of histological cores in some cases. The needle is also equipped with an internal sheath, which is withdrawn after the bronchial wall has been passed, avoiding contamination during EBUS-TBNA. The needle can be visualized through the lenses and on the ultrasound image. The ultrasonic bronchoscope is introduced to the area of interest via an endotracheal tube under visual guidance and with the patient under local anesthesia, usually as an outpatient procedure. The bronchoscope is inserted orally, with additional sedation usually with 2mg midazolam. Patients have to be monitored for electrocardiography, pulse oximetry, and blood pressure if an anesthesiologist is not present. Images can be obtained by directly contacting the probe or by attaching a balloon to the tip and inflating it with saline. Since the balloon is designed not to overinflate, it will not occlude the central airway. No experiences of technical difficulties using the balloon have been reported. Fig. 29.2 The needle is extended through the working channel and exits obliquely. Fig. 29.3 The 22-gauge needle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree