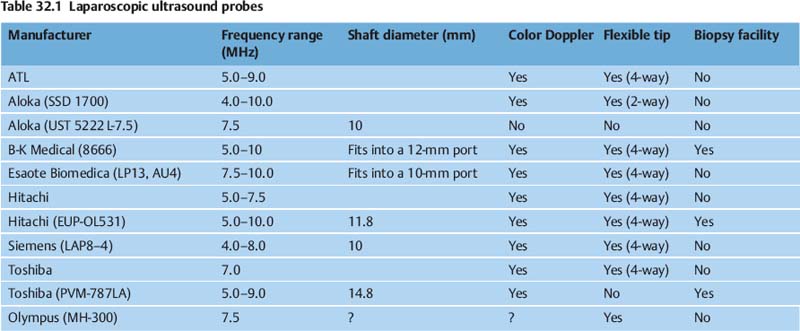
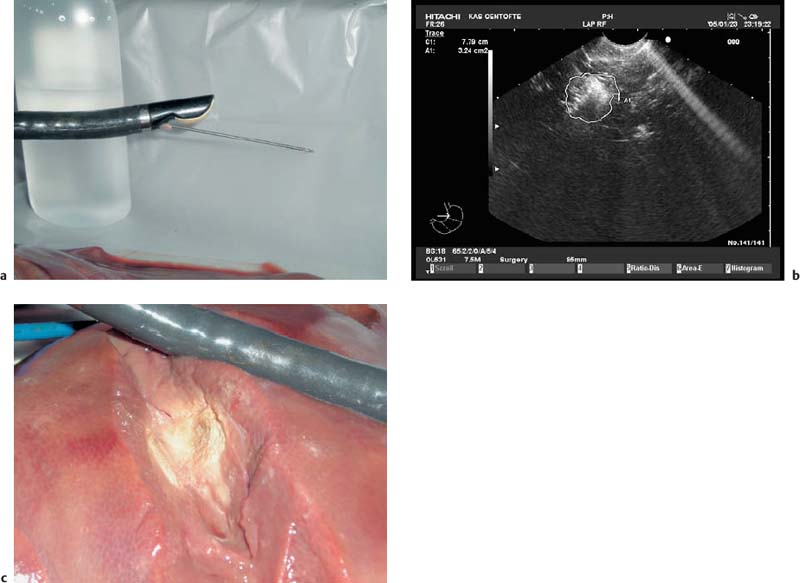
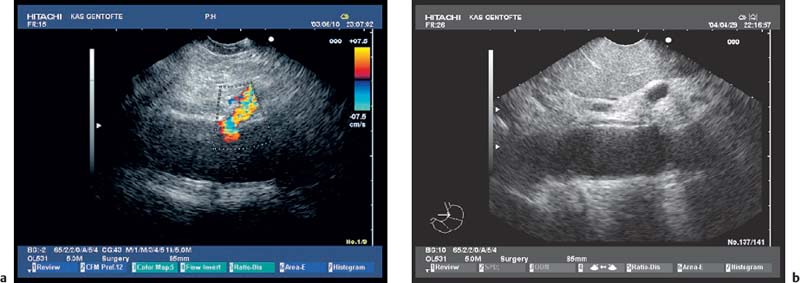
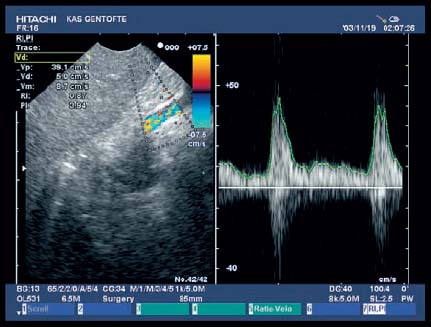
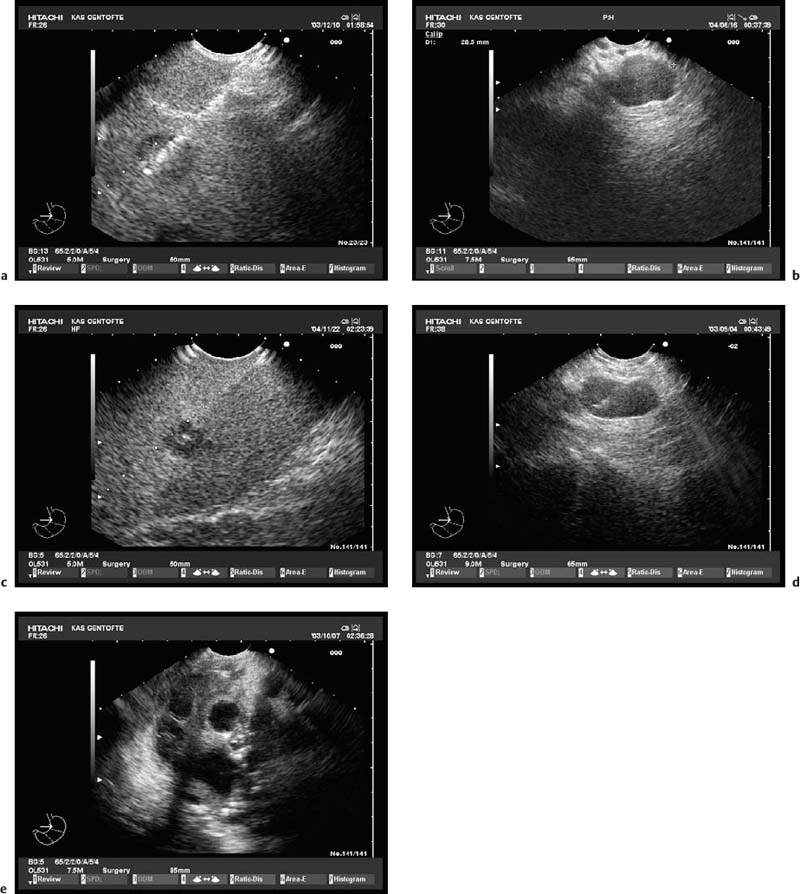
32 Laparoscopic Ultrasound Scanning Intraoperative ultrasound scanning has been in use for more than 40 years, and its value for detecting lesions in the pancreas, liver, and retroperitoneum is well documented. During the past 10–15 years, diagnostic laparoscopy and laparoscopic surgery have replaced many of the open procedures. This has led to an increasing need to find a substitute for the tactile feedback that manual palpation provides during open surgery. Recent technology has provided specially designed ultrasound probes that can pass through standard laparoscopic trocars in order to perform intra-abdominal as well as intrathoracic examinations and ultrasound-guided interventions (Table 32.1). Laparoscopic ultrasound scanning (LUS) represents a significant technical improvement in diagnostic laparoscopy and therapeutic laparoscopic interventions. This chapter provides a description of the procedure and the instruments used for LUS, with special focus on a new-generation LUS probe designed for LUS-guided interventions, as well as a review of the literature. The dedicated LUS probes currently available use electronic transducers with a linear or convex array mounted on a rigid or a flexible tip on the instrument. Movement of the flexible tip is controlled by a steering wheel located on the instrument’s shaft. Depending on the manufacturer, the tip can be moved in either two or four directions (Table 32.1). The frequency is either fixed at 5.0–7.5 MHz or variable, ranging from 4or5 MHz to 10 MHz. The new laparoscopic probes have additional features such as power Doppler and color Doppler. This is especially valuable for differentiating between vascular structures and tubular structures in which there is no flow, such as the common bile duct. Only one manufacturer (B-K Medical, Herlev, Denmark) offers an ultrasound unit that can be fully integrated into the laparoscopic rack. A remote control that operates the different ultrasonic functions is also available from the company. It is of course important for the operator to be able to control the ultrasound features personally instead of having a second person manipulating the ultrasound console. The laparoscopic image and the ultrasound image should preferably be superimposed (picture-in-picture). This option is important, because the movement of the transducer has to be coordinated with the real-time ultrasound image. Adequate sterilization has been one of the limitations of laparoscopic LUS. The transducers do not tolerate heating to more than 50–55 °C. Until recently, cleaning has therefore either been carried out using disinfection with glutaraldehyde or similar detergents, or alternatively, gas sterilization. Others have used sterile plastic coverings. However, none of these methods has been perfect. Recently, materials have been developed for the probes that allow Sterrad or Sterris sterilization (Advanced Sterilization Products, Irvine, California, USA) without damaging the transducers. Fig. 32.1 The laparoscopic ultrasound probe without its biopsy covering (Hitachi OL-531). Fig. 32.2 The transducer is electronic, with a scanning angle of 60° and a lateral and slightly oblique forward view. Fig. 32.3a, b Mounted at the flexible tip of the instrument, the transducer can be moved 90° up or down and left or right. The diameter of the probes is up to 1 cm, so that they can be introduced into the abdominal cavity through a standard trocar with a diameter of either 10 mm or 12 mm. There are at present only three manufacturers that provide biopsy facilities with the laparoscopic probe. The B-K probe was the first on the market. The biopsy channel is not fully integrated into the shaft of the probe. A flexible channel passes outside parallel to the probe, ending in a hole near the transducer.1,2 This means that a needle has to pass a flexible sheath that is not supported by the probe and that the tip of the needle has to be directed into an inlet near the transducer when a biopsy is needed. This maneuver is somewhat cumbersome, and this may be the reason why this procedure has not come into widespread use. The second company offering biopsy facilities with their probe is Toshiba (PVM-787LA). However, this probe is stiff, with a forward-viewing transducer and a diameter of 24 mm.3 The probe is primarily produced for radiofrequency ablation (RF) of liver lesions. Only one company has the biopsy channel fully integrated into a probe (Hitachi OL-531), with the probe being introduced via a standard trocar (Fig. 32.1). This probe was recently developed by the present author (P.V.) and the Hitachi company in collaboration. It has a diameter of 11.8 mm and fits into a 12-mm port. The total length of the instrument is 67 cm and the length of the insertion tube is 42 cm. The transducer is electronic, with a scanning angle of 60° and a lateral and slightly oblique forward view (Fig. 32.2). The curve radius is 10 mm. The central frequency is 7.5 MHz, with a bandwidth of 5–10 MHz. The transducer mounted at the flexible tip of the instrument can be moved 90° up or down and left or right (Fig. 32.3). A removable metal needle cover case around the body of the probe shaft forms a biopsy channel with a diameter of 3.2 mm (Figs. 32.4 and 32.5). The biopsy channel can be reduced to 2.4 mm with a mountable inner plastic tube (Figs. 32.6 and 32.7), allowing use of a modified 22-gauge or 19-gauge aspiration biopsy needle (SonoTip II, Medi-Globe Ltd., Achenmuhle, Germany) (Fig. 32.8). When it is not reduced, the biopsy channel allows the introduction of a standard-sized radiofrequency needle. The probe can be connected to a Hitachi ultrasound scanner (EUB-6500 or EUB-8500) with power and color Doppler facilities. The probe can be fully sterilized with Sterrad (H2O2 plasma) and ethylene oxide (ETO) gas sterilization. Laparoscopic ultrasound-guided biopsy has hitherto been a difficult and cumbersome procedure using the probes available on the market. The biopsy procedure with the new probe can be performed without difficulty during routine laparoscopic scanning. The probe also allows radiofrequency ablation of hepatic lesions during laparoscopic ultrasound scanning. A needle is at present under construction (the HiTT-Flex monopolar radiofrequency needle, compatible with the Elektrotom HiTT 106 ablation system; Berchtold Ltd., Tuttlingen, Germany) (Fig. 32.9). The construction of the new laparoscopic probe for guided interventions is a fresh advance toward minimally invasive procedures for primary diagnosis, staging, and treatment guided by laparoscopic ultrasound scanning. Fig. 32.4 A removable metal needle cover case around the body of the probe shaft forms a biopsy channel with a diameter of 3.2 mm. The image shows a proximal and oblique image of the metal cover, with a view into the biopsy channel inlet. Fig. 32.5 The metal cover is locked onto the probe shaft, and the transducer is ready for a laparoscopic ultrasonic examination with biopsy of a lesion. Fig. 32.6 The biopsy channel can be reduced to 2.4 mm with an inner plastic tube. Fig. 32.7 The inner plastic tube being introduced via the inlet on the metal cover. Fig. 32.8a–c a A prototype modified 22-gauge aspiration biopsy needle (SonoTip II, Medi-Globe Ltd., Achenmuhle, Germany). b The needle is introduced via the biopsy inlet of the laparoscopic probe. c The needle is now mounted on the laparoscopic probe, ready for a biopsy to be taken. Fig. 32.9a–c The probe also allows radiofrequency ablation of hepatic lesions during laparoscopic ultrasound scanning. a The radiofrequency needle (HiTT-Flex) has been introduced. b The image shows the burning effect visible during radiofrequency ablation of the liver in a swine model. c The necrosis seen after laparoscopic ultrasound-guided radiofrequency ablation in the liver. The procedure is carried out with the patient under general anesthesia. Several examination procedures have been described. The presetting of the image direction is, as usual, with distal to the right and proximal to the left in the ultrasound image. This provides images very similar to the endoscopic ultrasound (EUS) images obtained with linear transducers. The access site for the laparoscope and probe is selected depending on the indications for the examination. Most frequently, a supraumbilical or infraumbilical access site is chosen for the laparoscope itself. Some authors favor access via the right upper abdominal quadrant for the second port when the liver and hepatobiliary region have to be examined. Others use a port in the left upper quadrant. The aim is to obtain good access and to examine the region or organ in question in two directions. This can be accomplished by switching ports between the laparoscope and the probe. For the staging of upper gastrointestinal cancer, the present authors prefer the left upper quadrant and the supraumbilical port (Fig. 32.10). This provides good access to the left liver lobe, the region of the cardia, the hepatoduodenal ligament in a longitudinal scanning direction, and the pancreas in horizontal section. The aorta and the celiac vessels can be seen from the umbilical port, and the right liver lobe can be examined as well. LUS has to be conducted in a systematic way, including all segments of the liver, the hepatoduodenal ligament, and the celiac trunk and superior mesenteric artery. The intra-abdominal examination follows the same principles as transcutaneous ultrasonography. The images obtained during LUS are frequently excellent, with optimum scanning conditions, due to the close proximity to the intra-abdominal organs (Fig. 32.11). Generally, the contact technique is used to scan solid organs such as the liver. In the upper abdomen, the liver is usually also used as an acoustic window for more deeply located structures. Better image quality is sometimes obtained with indirect scanning through a saline solution. This method improves discrimination of individual wall layers and offers higher resolution in the transducer’s focal zone. When the liver is scanned, the transducer is placed directly on the left or right liver lobe. The liver is scanned systematically by moving the probe over all segments while simultaneously following it optically with the laparoscope, manipulated by an assistant (Fig. 32.12). The caudal parts of the liver should be examined from both the anterior and posterior surface. This is important, as small lesions just under the liver capsule can easily be missed due to their close proximity to the transducer. The location, number, and size of hepatic lesions must be documented. Relevant anatomic structures such as the portal and hepatic veins and bile ducts can be visualized. The segmental anatomy of the liver can be delineated and the relation of the tumor to these structures allows assessment of the extent of resection and the amount and function of the remaining liver tissue. The structures of the porta hepatis can be best assessed (in longitudinal section) when the probe is introduced through the left subcostal trocar and placed on segment IV of the liver. The distal part of the common bile duct is identified by positioning the transducer directly on the hepatoduodenal ligament. The stomach can be visualized by direct-contact scanning, or using the liver as an acoustic window. Acoustic shadowing of the posterior wall of the stomach and the pancreas can be avoided by aspiration of air and if necessary instillation of 300–500 mL saline solution through a nasogastric tube into the stomach. The branches of the celiac axis, portal vein, superior mesenteric artery, and aorta are displayed in transverse sections from the left subcostal trocar. Lymph nodes along these vessels are classified in accordance with the TNM classification (Fig. 32.13). Fig. 32.10 A typical working situation. The laparoscopic probe and the laparoscope have been introduced via two ports. The ultrasound scanner and the laparoscopic rack are seen, and the images are visible simultaneously. Fig. 32.11a, b The images obtained during laparoscopic ultrasonography are frequently excellent, with optimum scanning conditions due to close proximity to the intra-abdominal organs. a A laparoscopic ultrasound image of the aorta with the celiac trunk, seen with color Doppler. b A view of the aorta with the celiac trunk and the left gastric artery just below part of the left liver lobe. Fig. 32.12 A hepatic metastasis ≈ 10 mm in size in the right liver lobe. Fig. 32.13 A 14.5-mm hypoechoic lymph node in the retroperitoneum in a patient with gastric cancer. Fig. 32.14 Color Doppler examination is extremely valuable. The image shows a duplex scan of an abdominal vessel with color Doppler, pulsed Doppler, and B-mode scanning. Metastatic lymph-node involvement is characterized by a hypoechoic pattern, round shape, and well-delineated boundaries. Color Doppler examinations can be helpful in delineating the vascular anatomy and distinguishing vessels from lymph nodes (Fig. 32.14). Biopsy of lymph nodes is always relevant if a biopsy confirming malignancy will alter the management of the patient. Until recently, LUS-guided biopsy was if not impossible, then at least cumbersome. The needle had to be introduced through the anterior abdominal wall, and freehand guidance of the transducer had to be used.4–6 Alternatively, as with the B-K probe, the needle has to pass through an exterior floppy biopsy sheath before the biopsy maneuver is started.2,7 With the new LUS probe from Hitachi, the procedure has become simple and easy. After a lesion is outlined, the needle is simply introduced via the biopsy inlet of the probe and firmly connected to the Luerlock biopsy inlet (see Fig. 32.8b, c). The stylet is withdrawn a few millimeters. The needle can then be advanced under ultrasound guidance directly into the lesion (Fig. 32.15a). The stylet is removed completely, and avacuum is applied to the needle. To-and-fro movements are made, still with ultrasound guidance (Fig. 32.15b–e). The entire biopsy instrument is then removed, and the material is expelled onto glass slides and smeared for cytological evaluation. At present, only needles for fine-needle biopsy have been developed for this probe, but a Tru-Cut histological needle is commercially available for the B-K probe. It is only a matter of time before a histological needle becomes available for the Hitachi probe as well. In a single case in which fine-needle biopsy was not sufficient, the authors used the Tru-Cut needle designed for the B-K probe together with the OL-531 probe (Fig. 32.16). However, it should be emphasized that for safety reasons this is not at present recommended before a dedicated histological needle has been manufactured (the main risk being transducer damage). Fig. 32.15a–e The biopsy needle is introduced and a guided biopsy of a hepatic metastasis is taken. a Note the deflections from the needle just below the needle guide line. b A suspicious hypoechoic lesion in the left adrenal gland in a patient with gastric cancer. The laparoscopicultrasound (LUS)-guided biopsy revealed malignant cells, and the patient was ultimately staged as having incurable disease (M1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree