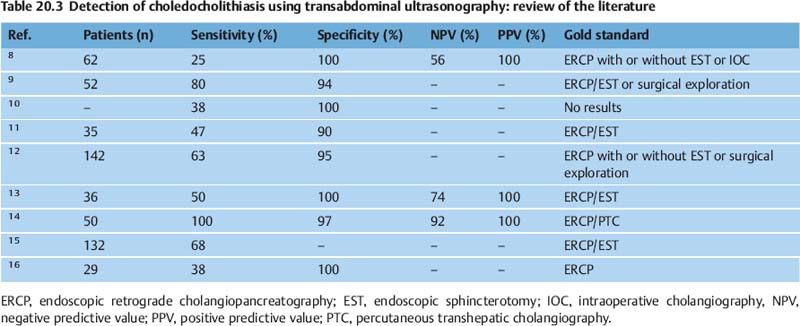
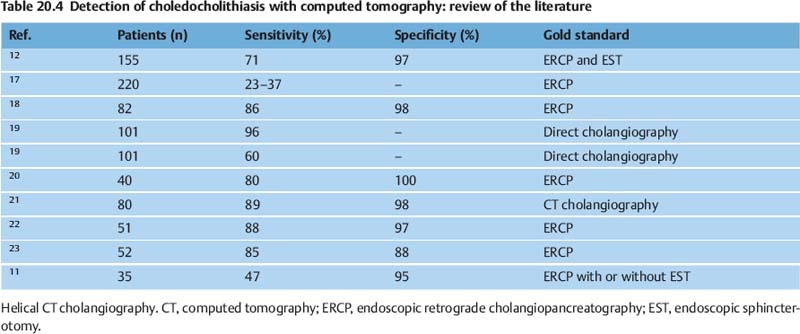
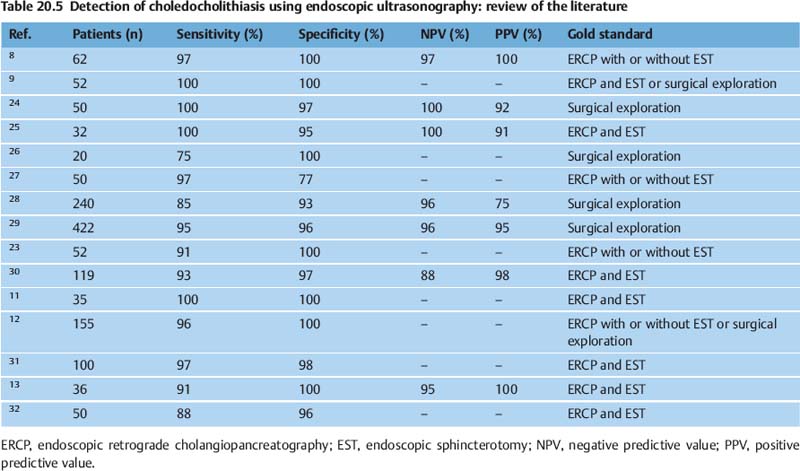
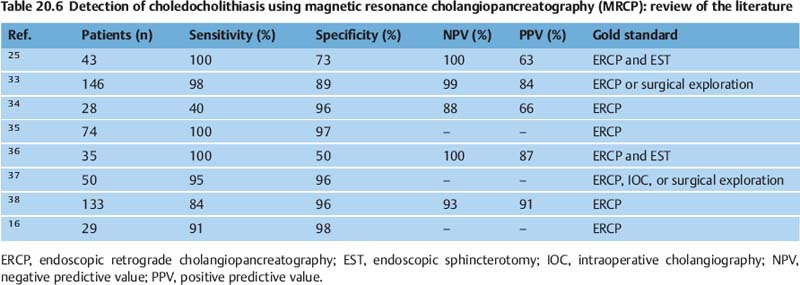
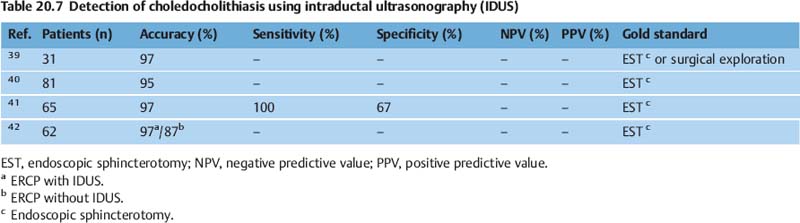
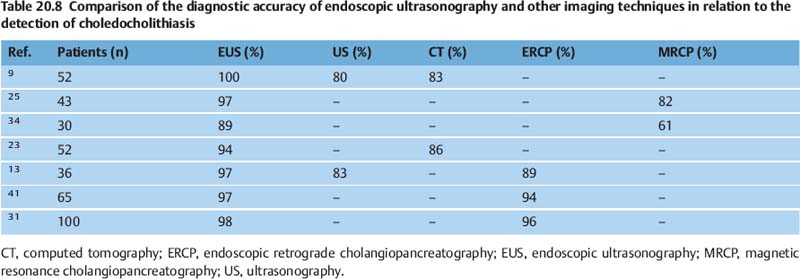
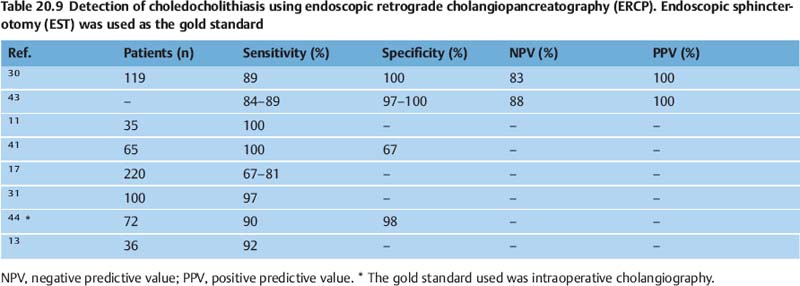
20 Endosonography of the Hepatobiliary System The term “cholelithiasis” refers to the presence of gallstones in the extrahepatic biliary tract. Depending on the location of the concrement, a further distinction is made between cholecystolithiasis and choledocholithiasis. A combination of the two conditions can be expected in 15% of patients. Reliability of Examination Methods for Detecting Gallstones The reported accuracy of examination methods is measured using four indices: sensitivity, specificity, and positive and negative predictive values (Table 20.1). Cholecystolithiasis can be detected by transabdominal ultrasound with a high level of sensitivity (Fig. 20.1, Table 20.2),1–7 but choledocholithiasis is more difficult do diagnose transabdominally (Table 20.3).8–16 Tables 20.4, 20.5, 20.6, 20.7, 20.8, and 20.98,9,11–13,16–44 present a review of the literature for the different methods used. Choledocholithiasis can be detected with conventional endoscopic ultrasonography (EUS), which is routinely used as a diagnostic procedure. Endoscopic retrograde cholangiopancreatography (ERCP) is currently regarded as the diagnostic gold standard, with a reported success rate of 90–96%. However, the value of diagnostic ERCP may have been considerably overestimated, as the rate of correctly diagnosed choledocholithiasis appears to be much lower—particularly since small gallstones (< 3 mm in diameter) with normal or even dilated bile ducts are easily overlooked even in ERCP.
Term | Definition |
Sensitivity (%) | True positives/(true-positives + false-negatives) |
Specificity (%) | True-negatives/(true-negatives + false-positives) |
Positive predictive value (PPV) (%) | True-positives/total positives |
Negative predictive value NPV (%) | True-negatives/total negatives |
Accuracy (%) | True-positives + true-negatives)/total number |
Youden index (%) | Sensitivity + specificity − 1 |
Ref. | Sensitivity (%) | Specificity (%) |
1 | 98 | 94–98 |
2 | 70 | 100 |
3 | 97 | 92 |
4 | 91 | 99 |
5 | 98 | – |
6 | 91 | 100 |
7 | 87 | 93 |
Fig. 20.1 Transabdominal imaging of choledocholithiasis. The lack of acoustic shadowing is a typical phenomenon in primary choledocholithiasis.
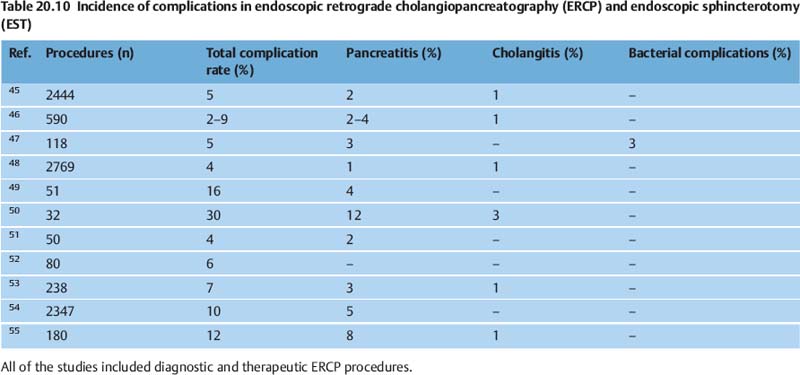
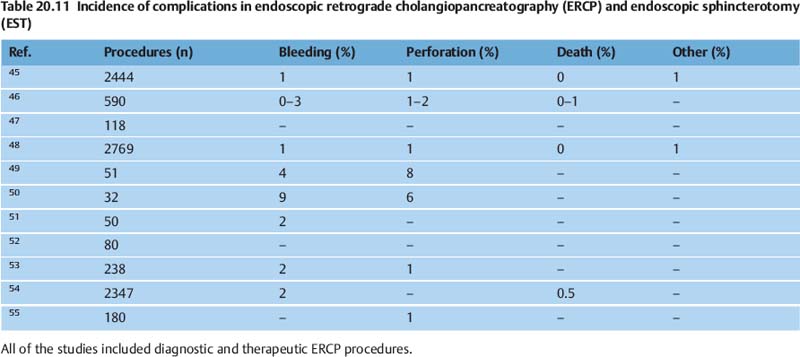
A combination of ERCP with endoscopic sphincterotomy (EST) is the treatment of choice in patients with choledocholithiasis, but this is an invasive technique with a significant risk of early and late complications. Typical early complications include pancreatitis, cholangitis, cholecystitis, bleeding, and perforation. In addition, EST leads to permanent dysfunction of the sphincter of Oddi. Late complications include recurrent gallstones (3–20%) and papillary stenosis (2–6%). The total rate of complications is reported to be in the range of 2–30%. A review of the literature on the incidence of various complications in ERCP and EST is presented in Tables 20.10 and 20.11.45–55
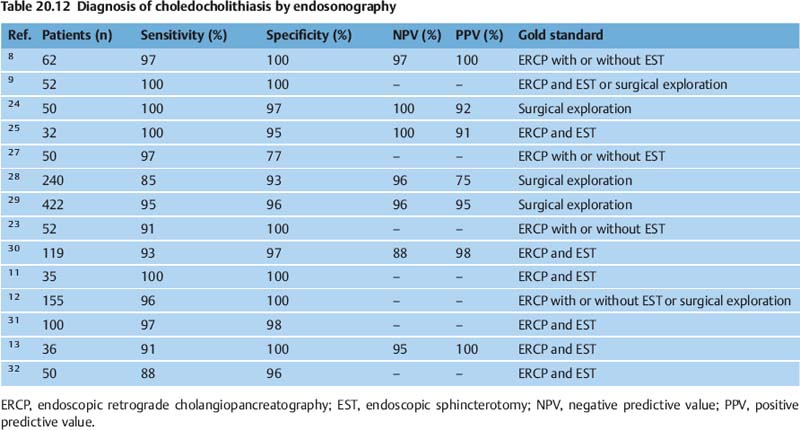
In conditions with equivocal signs or symptoms suggesting choledocholithiasis, EUS is a reliable low risk-method to establish a correct diagnosis and indication for EST. Table 20.12 presents a review of the literature.8,9,11–13,23–25,27–32
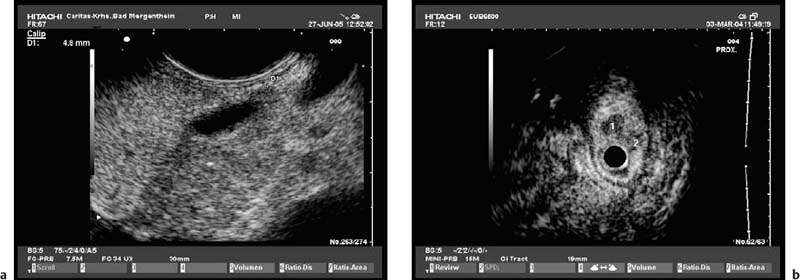
EUS provides excellent visualization of the proximal and distal common bile duct (Fig. 20.2), and of the ampulla and left intrahepatic bile ducts, with a very high sensitivity for even very small stones. In 96% of patients, the entire length of the common bile duct can be visualized, but imaging of the bile ducts of the right lobe of the liver and the hepatic hilum is more difficult. The results of endosonography have been shown to be independent of the size of the concrement or the diameter of the bile duct, and gallstones smaller than 2 mm have been detected even in dilated bile ducts. Another major advantage of endosonography is the very low rate of morbidity, mortality, and severe complications associated with the procedure. In summary, conventional EUS is a safe, reliable, and minimally invasive method of detecting choledocholithiasis.
Fig. 20.2a, b a A normal duodenal papilla (between the markers) in routine conditions.
b In a few patients, the orifices of the common hepatic bile duct and pancreatic duct can be imaged separately. The common bile duct orifice (1) and the pancreatic duct orifice (2) are indicated here. ( Videos 20.1–4.)
Videos 20.1–4.)
The relevance of endosonography for diagnosing cholecystolithiasis before cholecystectomy has yet to be examined and can only be determined in large prospective studies including sufficient numbers of patients with and without cholecystolithiasis. Unexpected diagnostic results, such as benign papillary stenosis and anatomic variations in the bile duct system, need to be taken into account in advance.
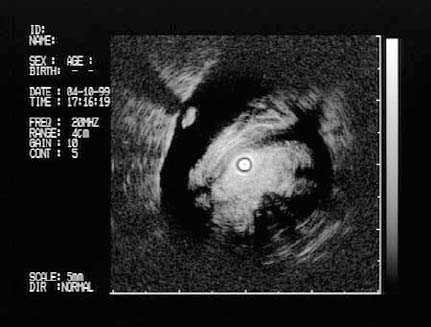
Fig. 20.3 Imaging of choledocholithiasis using extraductal ultrasound (EDUS). Ideally, minusculeconcrementsonlyafewmillimeters in size (microlithiasis) can be identified even in bile ducts of normal width. Concrements of this type may not be visible on endoscopic retrograde cholangiopancreatography.
Miniprobe EUS and Extraductal Ultrasound
EUS miniprobes introduced through the working channel of a regular endoscope can be used in the same way as ordinary endoscopy accessories such as biopsy forceps. With a penetration depth of ≈ 2 cm, they allow visualization of considerable areas of important anatomy around the upper gastrointestinal tract. Catheter probes may be able to cover most of the indications for conventional diagnostic EUS; this would certainly apply to pathological structures in the intestinal wall. Interventional procedures may be reserved for longitudinal scanners with stiff shafts and wide working channels.
The distal common bile duct (CBD), running from the major duodenal papilla up to the liver just behind the duodenal wall, is certainly within the reach of diagnostic miniprobe EUS. Extraductal ultrasonography (EDUS) of the distal CBD for the detection of choledocholithiasis, with the miniprobe in a duodenal position, was investigated in a prospective study including 119 patients with suspected choledocholithiasis.30 The probe was introduced through a duodenoscope and first placed on the duodenal papilla to image the sphincter, and then moved slightly more cranially to scan the distal CBD and pancreatic duct. A diagnosis of choledocholithiasis was made when hyperechoic structures not adherent to the ductal wall were detected, with or without acoustic shadowing (Fig. 20.3). ERCP with EST and pull-through of a Dormia basket were used as the gold standard. The EDUS diagnosis of choledocholithiasis was confirmed in 33 of 34 patients (97%). As expected, EDUS failed to detect peripheral lesions. The study shows that EDUS can reliably detect pathological lesions in the distal common bile duct, particularly small concrements, and can therefore avoid the need for sphincterotomy with the associated complications.
Additional diagnostic applications of EDUS for the duodenal papilla were evaluated in another prospective study including 150 patients with similar diagnostic issues and methods. It was shown that in addition to choledocholithiasis, chronic pancreatitis, adenomas of the papilla, adenomas of the bile duct, and primary sclerosing cholangitis (PSC) were capable of being detected reliably using this method.56 In summary, EUS or EDUS is indicated before cholecystectomy, especially in patients who are at intermediate risk, and these techniques appear to be superior to other diagnostic methods. In addition, EUS is definitely indicated for staging of carcinoma of the ampulla of Vater. EUS is less important in the staging of cholangiocellular carcinoma than it is for pathologic processes in the papilla. Intraductal ultrasonography (IDUS) has diagnostic value particularly in stenoses of unknown origin in the common bile duct.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree