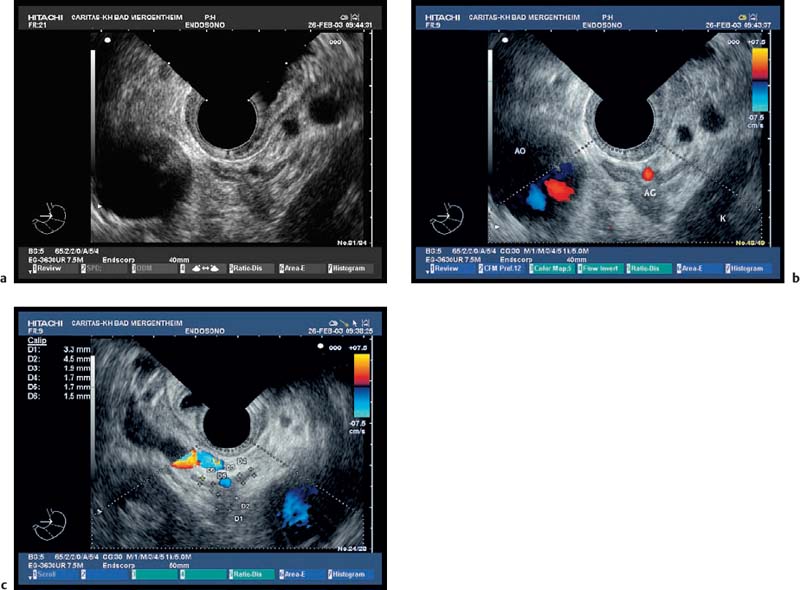
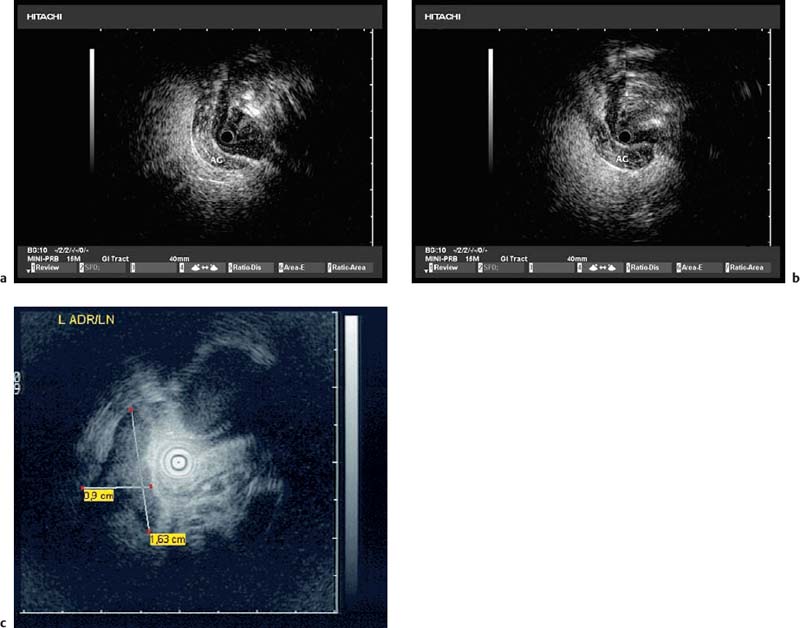
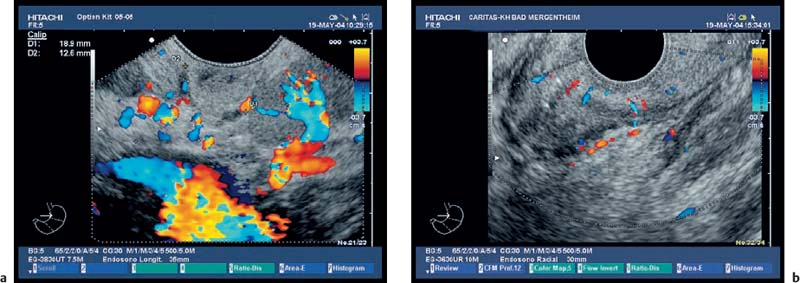
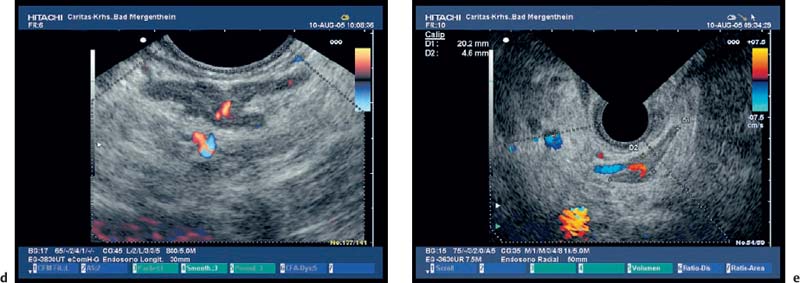
21 Endoscopic Ultrasound Imaging of the Adrenals Endosonographic imaging of the adrenal glands, and thesystematic use of the method in diagnostic procedures for adrenal diseases, have been reported for over 15 years. Endosonographic imaging of the left adrenal gland was first described by Chang et al.1 In a small group of 31 patients, the normal left adrenal gland was delineated using endoscopic ultrasonography (EUS) in 97% of cases; detection of the right adrenal gland was only reported in one patient, with a J-shaped stomach. Imaging of the right adrenal gland was therefore initially found to be more problematic. In the meantime, a great deal of experience has been gained in carrying out endosonographic imaging of the adrenal glands and in assessing the value of this diagnostic technique.2–18 Both the imaging quality and precise identification of healthy—i.e., morphologically normal—tissue in the adrenals have markedly improved. In particular, modifying the imaging technique for the right adrenal gland made a substantial contribution to progress in this area. It is now possible to distinguish between the medulla and cortex in both adrenals, very small tumors can be identified, and in particular, atrophic adrenals can be demonstrated as a manifestation of autoimmune Addison disease. Due to the complementary role of transabdominal and endoscopic ultrasound for examining the adrenal glands, both methods are described here. Cadaver studies. The transabdominal and endoscopic examination technique has recently been validated in corpses. To establish the correct identification and echo pattern of the adrenal glands, the sonographic appearance was documented. Right adrenal gland. The right adrenal gland is examined in a slightly left lateral position, with the patient’s right arm raised above the head to widen the intercostal space. The right adrenal gland is located using the upper pole of the kidney, the inferior vena cava, the crus of the diaphragm, and the margin of the liver as guiding structures. The inferior vena cava, as the medial border, can always be delineated, as well the crus of the diaphragm. For correct identification, the typical echo pattern (bright, dark, bright, dark, and bright echo lines), defined by the pathological anatomical study, has to be visualized. The thickness was measured as 5 ± 1mm (range 4–8mm). The thickness of the adrenal wings, measured in their middle representative symmetrical portion in healthy control individuals, was comparable to the EUS findings. Both were slightly larger than the documented diameters in the cadavers. This may have been due to pressure from the directly applied transducer on the adrenal gland, or differences in blood filling. Left adrenal gland. The left adrenal gland can be examined with the patient in a supine or slightly (right) oblique position, with the left hand raised above the head to widen the intercostal space. Typically, it is seen between the upper pole of the left kidney, pancreatic tail, spleen, crus of the diaphragm, and aorta. In some cases, better visualization is achieved by applying the transducer ventrally, documenting the celiac trunk, splenic and left renal vessels, pancreas, aorta, and left kidney. Identification of normal adrenal glands, and particularly the right adrenal gland, is possible with transabdominal ultrasonography in most healthy individuals. Reported differences in the detection rate of the adrenal glands may also be due to differences in the equipment used. However, EUS is capable of detecting almost all left and most right adrenal glands, if required. Endosonographic imaging of the adrenals is easier with a longitudinal echoendoscope, but is also possible with radial transducers. Using these instruments, the adrenal glands can be visualized best by sector scanning; switching the frequency from 7.5 to 5.0 MHz is sometimes useful, as it improves the imaging of the right adrenal gland, which is frequently further away from the transducer than the left adrenal gland, within a range of < 30 mm. In addition, the device also provides the option of carrying out EUS-guided fine-needle aspiration biopsy of adrenal masses in patients who may benefit from cytological and histological assessment. Fig. 21.1a–e a A normal left adrenal gland imaged using conventional B-mode. b, c Color Doppler imaging, showing the hilum with the afferent artery (b) and efferent vein (c). AG, adrenal; AO, aorta; K, kidney. d Longitudinal scanning. e Radial scanning. The adrenal hilum and adrenal vessels can be delineated with both methods. Miniprobe ultrasound with longitudinal scanning is of no value (not shown). Sedation. The echoendoscope is inserted with the patient lying on the left side. Since imaging of the adrenals often involves detection or exclusion of very small morphological changes, sufficient sedation is mandatory. The authors use different approaches to sedation. One author (C.F.D.) always uses propofol sedation without local anesthesia; the other (P.H.K.) prefers the following approach: after administering local anesthesia of the pharynx with a spray, and an intravenous injection of atropine (0.25 mg), premedication is administered with pentazocine (30 mg) and diazepam (10–20 mg). Left adrenal gland. Landmarks for correct identification of the left adrenal are the cranial pole of the left kidney, the distal pancreatic tail, and the splenic vessels. Typically, after entering the stomach the transducer is kept toward the left posterior gastric wall and shows a variable section of the abdominal aorta at 45 cm; a little more caudally, the upper pole of the left kidney is seen. The transducer should be angulated slightly medially and retracted. The adrenal gland is seen on the way between the upper pole of the left kidney and the aorta, just below the splenic vein. The fact that it typically overlaps the aorta ventromedially by ≈ 0.5 cm is very helpful in finding the correct position. In some cases, the left adrenal gland can also be seen with the transducer in the ascending part of the duodenum. For correct identification, the typical sonographic echo pattern (bright, dark, bright, dark, and bright echo lines) has to be documented. The mean EUS examination time for the left adrenal gland has been reported tobe2 ± 1 minutes, starting on entry into the stomach, demonstrating that the procedure is not time-consuming (Fig. 21.1). Due to its proximity to the posterior gastric wall, miniprobe ultrasonography of the left adrenal gland is also possible (Fig. 21.2). Right adrenal gland. Imaging of the right adrenal gland is easiest to carry out when the transducer is placed in the antrum, just in front of the pylorus, after which the patient should lie on the right side. The transducer is now flexed fully toward the right, so that the tip of the echoendoscope is behind the angular notch. With the transducer in this position, the echoendoscope is carefully retracted until the landmarks (the cranial pole of the right kidney, inferior vena cava, caudal parts of the liver, and the portal vein) can be identified. After this, the right adrenal gland can be imaged behind the inferior vena cava. As in the transabdominal examination, this technique makes it possible to distinguish between the echoes generated by the adrenal medulla and those generated by the cortex (Fig. 21.3). Fig. 21.2a–c Imaging of a normal left adrenal gland (AG) using miniprobe technology next to the pancreas. Fig. 21.3a, b a The right adrenal gland, between the markers. b
 Transabdominal Examination Technique
Transabdominal Examination Technique
 Endoscopic Ultrasound Examination Technique
Endoscopic Ultrasound Examination Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree